Two studies have used electrophysiological methods to directly assess brain activity evoked by symptom provocation prior to and following treatment. A study that assessed cortical activation (EEG) while viewing trauma-related pictures in subjects with PTSD compared with wait-list control subjects reported that, prior to treatment, both groups exhibited greater activation in the right hemisphere.
62 Following successful treatment [cognitive behavioral therapy (CBT)], there was a reduction in right hemisphere activation in frontal regions. This correlated with symptom improvement, suggesting normalization.
62 In the other EEG study, PTSD subjects were assessed before and after treatment while listening to a script of their trauma.
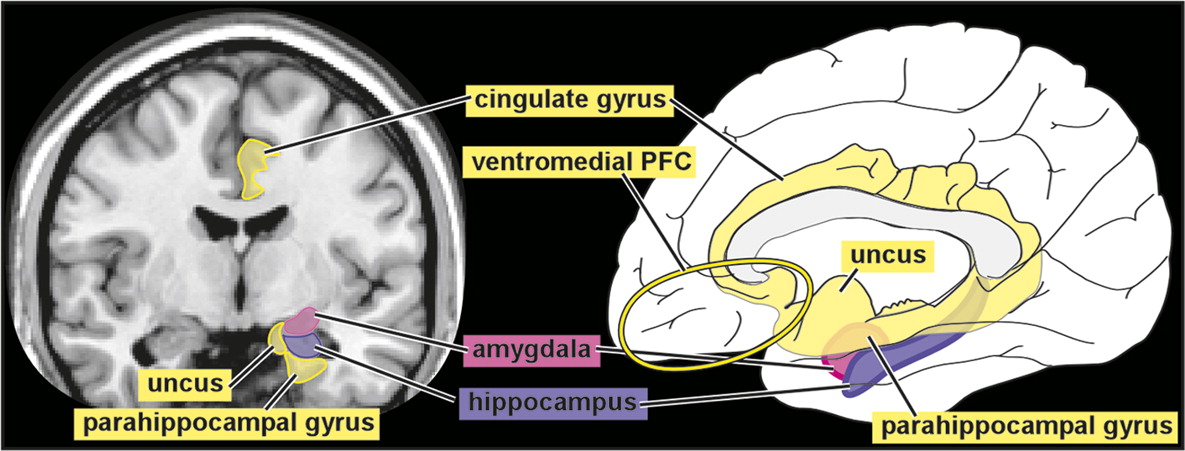
63 Before treatment, the PTSD group exhibited a significantly higher cortical activation than trauma-exposed control subjects in the bilateral orbitofrontal and anterior cingulate cortices (delta, alpha, and beta 1 bands), bilateral parahippocampal gyri (delta and theta bands), and bilateral posterior cingulate cortex (theta band). After successful treatment (eye movement desensitization and reprocessing therapy), the PTSD group demonstrated significantly increased cortical activations during script listening in the right fusiform gyrus (delta, theta, alpha, and beta 1 bands) and the visual cortex (delta and theta bands). A connectivity analysis revealed decreased connectivity (theta band) between the left visual cortex and right fusiform gyrus. The authors of this study noted that these results suggest a shift in maximal cortical activation during script listening from prefrontal and limbic areas to primary and higher-order visual areas and normalization of visual processing.
63 Thus, both EEG studies suggested that treatment promoted normalization of processing.
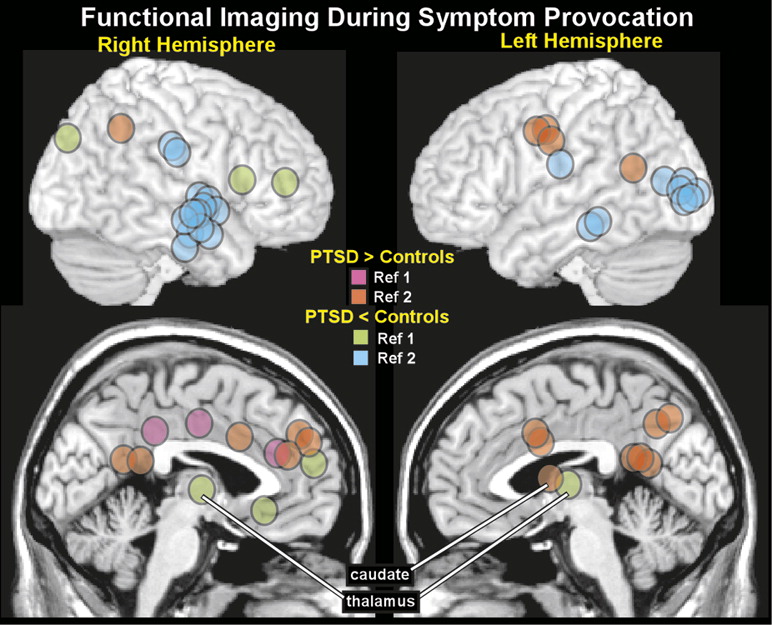
Several studies have used indirect functional imaging methods to assess treatment-related changes. Three studies have reported changes in CBF (SPECT). Two studies compared CBF increases induced by listening to a personal trauma script in subjects with PTSD to both waitlist and trauma-exposed control subjects.
3,5 In one study, CBF was higher in the right insula and superior/middle frontal gyri in the PTSD group compared with trauma-exposed control subjects.
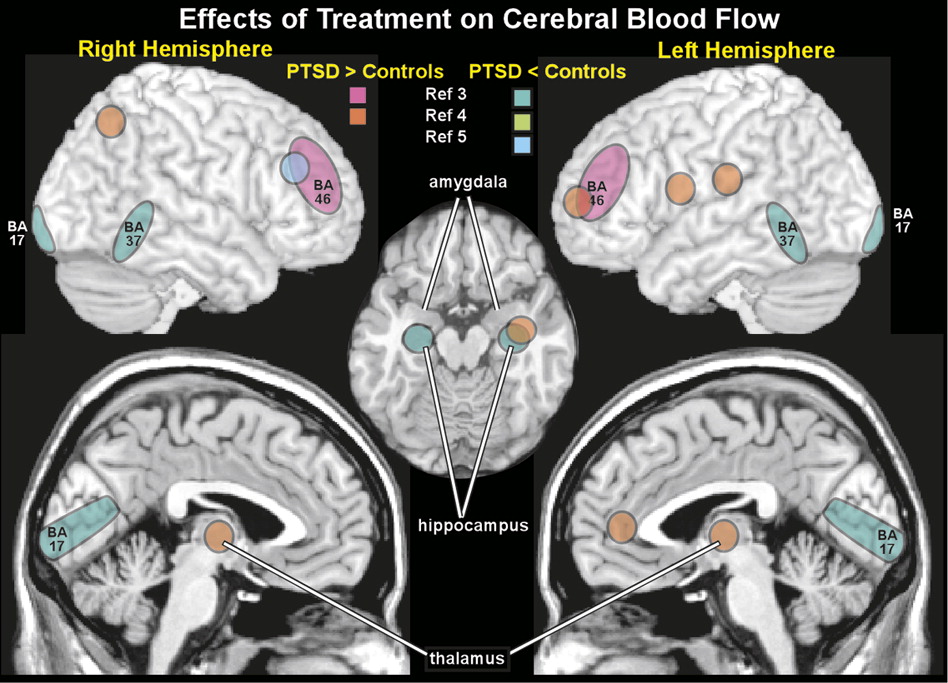
5 Treatment (brief eclectic psychotherapy) was associated with decreased CBF in the right middle frontal gyrus, suggesting some normalization of function (
Figure 3). CBF was decreased in the right uncus in waitlist control subjects. Symptom improvement correlated with CBF changes in the bilateral superior/middle frontal gyrus and left superior temporal gyrus. In the other study, CBF was decreased in bilateral temporal poles, mesial temporal, superior/middle temporal, and orbitofrontal cortices compared with trauma-exposed control subjects.
3 Following treatment (eye movement desensitization and reprocessing therapy), pretreatment differences (volume of interest) in CBF between treatment responders (11 of 15 patients) and trauma-exposed control subjects were no longer significant, suggesting normalization. However, within-subject analyses did not reveal significant changes pre-post treatment. When treatment responders (11/15) were compared with nonresponders (4/15), CBF was decreased in the temporal cortex (BA37), visual cortex (BA17), and hippocampus; CBF was increased in the dorsolateral PFC (BA46) (
Figure 3). The third study examined CBF changes in subjects with subthreshold PTSD before and after treatment and waitlist control subjects during recall of trauma-related material.
4 After successful therapy (brief psychotherapy with cognitive restructuring and exposure components), within-subject analyses identified significantly decreased CBF in the left amygdala and increased CBF in the left dorsal anterior cingulate cortex, dorsolateral and ventrolateral PFC, and hippocampus, as well as bilateral parietal lobes (BA 40, BA 7) and thalamus (
Figure 3). Correlational analyses indicated significant positive correlations between the change in CBF of the left PFC and both the left thalamus and left parietal lobe. Furthermore, symptom reduction was positively correlated with the left PFC CBF and negatively correlated with the amygdala CBF.
4 Another study used near infrared spectroscopy to measure functional activation (based on increased regional concentration of oxyhemoglobin) during trauma recall within the lateral prefrontal cortex in subjects with PTSD prior to and following eye movement desensitization and reprocessing therapy.
64 After treatment, within-subject analyses indicated significantly less activation in this area; these changes were associated with reduction in symptoms. An fMRI study compared brain activations during trauma reminders in police officers with subthreshold PTSD to both waitlist and trauma-exposed control subjects (all police officers).
65 At baseline, both subthreshold PTSD groups had higher activity in the left amygdala and lower activity in the orbitofrontal and medial PFC than trauma-exposed control subjects. Following treatment (cognitive restructuring and exposure therapy), activity was increased in the orbitofrontal and medial PFC and decreased in the amygdala, suggesting normalization of activity. Another fMRI study compared brain activations during an emotional face memory task early in treatment for PTSD and 6–9 months later, when 65% no longer met diagnostic criteria.
66 There was a positive correlation between memory-related activation in the amygdala (modulation of memory by emotion) and ventromedial PFC (episodic memory) and CAPS at both time points. In contrast, changes in memory-related activation in the anterior hippocampus and subgenual anterior cingulate cortex significantly correlated with degree of recovery, but not with current CAPS. Studies using other types of tasks (e.g., attention, concentration, social cognition, emotional faces, affective Stroop) have also documented changes in brain activations following treatment.
67–72 Although differing greatly in both research methodology and subject characteristics, overall, these studies indicate that effective psychotherapy can be associated with both compensatory changes and normalization of brain activity.