The AMA reaffirmed its support for parity coverage of mental illness and substance abuse and for access to mental health services after hearing testimony from a parent and patient advocate about problems related to coverage and reimbursement for treatment of eating disorders.
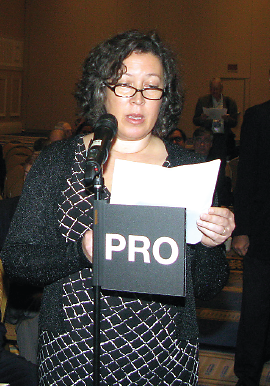
Laura Collins, the founder of F.E.A.S.T. (Families Empowered and Supporting Treatment of Eating Disorders), testified at last month’s Interim Meeting of the AMA House of Delegates in Washington, D.C., in support of a resolution calling on the AMA to advocate for federal legislation requiring full insurance coverage of medically appropriate treatments for eating disorders (ED), including inpatient, outpatient, and maintenance care.
Collins explained that despite the parity law and the Affordable Care Act, not all insurance policies cover comprehensive treatment for eating disorders. “Why do we need a full spectrum of ED treatment covered by insurance? Because EDs are treatable, but we’re not doing it,” Collins said. “Yes, eating disorders are treatable brain disorders. They are not a ‘problem with food’ or a weight issue. They are not a choice by the patient nor are they caused by bad parenting or size 0 models. . . . Untreated, or treated inadequately, eating disorders maim and kill. When my daughter became ill, I learned for the first time that my dear 14-year-old girl had a 1 in 10 chance of dying of her anorexia.
“What I didn’t know then was that newer treatments can have far higher rates of recovery in a much shorter time. Others need more. But few were getting any. We need insurance coverage to save lives: early intervention and access to care across settings works. . . . The current situation for American families facing a newly diagnosed eating disorder is grim. We face a revolving door of emergency care instead of access to the care needed early on. We second-mortgage homes, drain retirement, but more often simply don’t pursue care due to financial constraints—for a treatable problem. These patients are not dying of their disorder; they are dying from lack of access and lack of coordination.”
The resolution was introduced by the delegation from Indiana but received the support of the Section Council on Psychiatry and the Neuroscience Caucus—a group of organizations within the AMA House (including APA and the Section Council on Psychiatry) interested in advancing issues relevant to neuroscientific research and physicians treating patients with neuropsychiatric disorders.
David Fassler, M.D., alternative delegate for the American Academy of Child and Adolescent Psychiatry, also testified in support of the resolution. “It’s estimated that eating disorders affect over 20 million children, adolescents, and adults,” he said. “These are very real illnesses with serious and, at times, even fatal consequences. The best chance for successful treatment is a comprehensive plan, individualized to the needs of the patient. Unfortunately, many insurance plans still don’t provide adequate coverage for the evaluation and treatment of eating disorders.
“The AMA has clear and consistent policy in support of mental health parity,” Fassler said. “And based on this policy, the AMA has been a critical and effective ally in the ongoing legislative and regulatory efforts to require insurance companies to provide appropriate coverage for the treatment of mental health and substance use disorders. Yet despite the gains of recent years, many policies still lack adequate coverage for the treatment of eating disorders.”
During hearings on the resolution, other delegates supported the intent of the motion, but expressed concern about putting the AMA on record in support of new health mandates. In its place, the House reaffirmed existing policy in support of parity and access to mental health treatment. That policy calls on the AMA to continue to work with national medical specialty societies and other professional and patient advocacy groups to identify and eliminate barriers to access to treatment for mental illness; advocate that psychiatrists and other physicians who provide treatment for mental illness be paid by both private and public payers for the provision of evaluation and management services, for case management and coordination efforts, and for interpretive and indirect services; and advocate that all insurance entities facilitate direct access to a psychiatrist in the referral process. ■