Adolph Meyer, once the dean of American psychiatry, has received a lot of bad press in recent decades, some of it pretty brutal, maintains Paul McHugh, M.D.
For instance, Edward Shorter in his History of Psychiatry wrote that Meyer was a “second-rate thinker and a verbose writer,” while Richard Noll in American Madness said that “he had confidence but it outstripped his competence.”
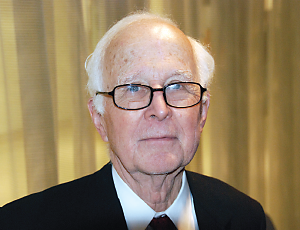
Not so fast, said McHugh, a University Distinguished Service professor of psychiatry at Johns Hopkins in a February lecture in Baltimore.
Meyer may have had his flaws but his influence remains strong 60 years after his death, McHugh emphasized. That influence has largely come down to the present filtered through the work of his successors—many of whom worked or still work at Hopkins.
Meyer started out modestly as an immigrant pathologist, dissecting brains of deceased patients at the Illinois State Hospital in Kankakee in 1893.
“Meyer realized that he knew nothing about psychiatry, but neither did anyone else at the time,” said McHugh. “Emil Kraepilin’s landmark fifth edition wouldn’t be published until 1896, and Freud was still fussing with cocaine.”
So Meyer sought to explain to the few psychiatrists at Kankakee that learning something from clinical pathology required a correlation with the clinical history of the living mental patient. He went out on the wards and provided the doctors with a form for taking the comprehensive history and physical exam he believed were needed to gather data.
“Meyer believed psychiatric patients needed to be closely studied as individuals,” he said. “It was a sophisticated common-sense approach that suggested treatment and research directions.”
After stops in Worcester, Mass., and New York, Meyer moved to Baltimore and Hopkins in 1910, where he soon developed three core ideas.
First, he articulated his concept of psychobiology—the scientific study of life at the psychological level, said McHugh. For Meyer, the patient’s life and social environment were central to understanding his condition. Disorders were reactions or responses to something going on in the patient’s life.
Second, mental disorders emerge from that life, not from a single cause, he believed. Mental disorders do not “strike” the patient like a broken arm, said Meyer. They have multiple origins. This led Meyer to oppose the eugenics movement, because he observed too many nonhereditary causes of mental illness.
Finally, the psychiatrist’s job is not to diagnose disorders but to “formulate patients,” working to understand problems arising from the patient’s entire life. “Formulation” would take into account personal choice, accident, potential, and assumptions, as well as history and symptoms.
Meyer’s broad view of patients extended beyond just providing therapy. He admired Jane Addams’ Hull House in Chicago, advocated for the care of vulnerable families, and argued for systematic study of populations.
Yet Meyer’s role in this early version of the biopsychosocial model got obscured by the rise of psychoanalysis, said McHugh.
Meyer retired from Hopkins in 1940, 10 years before his death. A small group of psychiatrists and others, many at Hopkins, carried his influence over the “psychoanalytic gap” and up to the dawn of the biological psychiatry age.
Leo Kanner, M.D., described autism in 1943. Paul Lemkau, M.D., founded the Department of Mental Health in Hopkins’ School of Public Health and conducted some of the first surveys on mental illness. He cross-checked DSM-III diagnoses against intensive workups performed at Hopkins’ Phipps Clinic.
Jerome Frank, M.D., collected data on many patients and did not find similar causes but rather similar presentations. Jane Murphy developed labeling theory, while Hilda Lewis published studies refuting the idea of a single cause for mental illness.
Meyer’s view of psychiatry still resonates in contemporary psychiatry, despite what his detractors say, argued McHugh.
Now, studies of epigenetics are revealing that genes do not rigidly predict behavior or illness, as the eugenics movement mistakenly believed. Psychiatric epidemiology is leading to new understanding of the extent of mental illness and showing the importance of making care available in patients’ communities. New insights into geriatric psychiatry consider the patient’s condition, history, and the environment and are “Meyerian to the core,” said McHugh.
Finally, there are people such as Hopkins psychiatry professor Kay Redfield Jamison, Ph.D., whose bestselling books about her own experiences with mental illness have helped undercut stigma and draw patients into treatment.
“In short, if Meyer were in the room with us, he would say, ‘I feel right at home,’ because he would be,” said McHugh. ■