Understanding how the teenage brain functions under normal circumstances can be challenging. But, for researchers studying major depressive disorder (MDD)—the leading cause of morbidity and disability among adolescents—developing a sense of how the brains of teens with MDD differ from those without may offer new insight into prevention and treatment.
With advances in neuroimaging—notably functional magnetic resonance imaging (fMRI), which measures brain activity through changes in the levels of blood flow—there has been a growing interest in studying abnormalities in the brain structure and function of people diagnosed with depression.
“Most of these imaging studies have focused on one specific brain region that is believed to be connected with a certain symptom,” said Ian Gotlib, Ph.D., the David Starr Jordan Professor of Psychology at Stanford University and director of Stanford’s Mood and Anxiety Disorders Laboratory. “And those are important studies for our scientific understanding, but what has been lacking [in youth] has been an integrated look at a depressed brain and how these regions interact with each other.”
Gotlib believes that developing such integrated models is important, given the Research Domain Criteria (RDoC) initiative set forth by the National Institute of Mental Health (NIMH), which aims to view mental disorders through the prism of biological and neurological measures.
In an effort to identify common brain abnormalities and characterize their relationship with specific psychological dysfunctions, Gotlib and his colleagues conducted a meta-analysis of 14 fMRI studies of children and young adults (246 MDD patients and 274 matched controls aged 4 to 24). Their findings were published September 2 in JAMA Psychiatry.
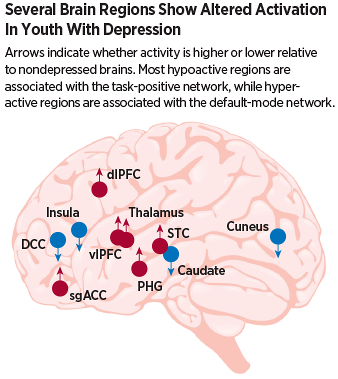
The combined picture showed several consistent anomalies that fell into two main categories, and together they helped explain some of the disparate symptoms seen in depressed teens.
Children and adolescents with depression displayed increased activity related to the processing of negative emotions, which could explain common symptoms such as over-sensitivity to emotional stimuli and an inability to regulate their own emotions. They also had diminished activation in areas associated with executive functioning, which could lead to symptoms like excess rumination and lack of motivation.
The changes in specific brain regions also generally paralleled findings seen in adults with MDD, though there were a couple of unexpected alterations.
“The major surprise we observed was that the ventrolateral prefrontal cortex, one of the areas involved in regulating emotions, was hyperactive in youth,” Gotlib told Psychiatric News. “And the traditional lore has been that is an underactive area in adult depression.”
Gotlib suggested that such changes in activity as an adolescent with depression grows older may reflect an adjustment to compensate for overstimulation. “You can imagine a scenario where this region gets exhausted with the excess activity and trying to modulate emotions, and therefore the connections become downregulated over time,” Gotlib said.
As for his lab’s future goals, they involve taking this knowledge gained from the imaging studies and testing whether focused interventions can alter maladaptive patterns of brain activation. “If we know that a patient has faulty circuits related to emotion regulation, for example, could we train them to think or act in certain ways that could change their activity patterns?”
This study was supported by grants from NIMH as well as fellowships from the National Science Foundation and Stanford University. ■
An abstract of “Meta-Analysis of Functional Neuroimaging of Major Depressive Disorder in Youth” can be accessed
here.