A study published February 16 in Translational Psychiatry has identified a genetic variant that might help predict those who are prone to cannabis-induced psychosis.
A team in the United Kingdom enrolled 442 young cannabis users (aged 16 to 23) and tested their working memory and psychotic symptoms both while intoxicated and drug free; they also collected DNA samples and tested for the presence of variants in two genes: AKT1 and COMT.
These two genes were chosen as they have been shown to be connected with cannabis and psychosis risk, though previous research has focused on people with a familial history of schizophrenia. This work sought to test whether these genes have any influence in people with no inherent risk.
Also, while many previous studies used participant recollection for marijuana use, investigators in this trial actually watched all the participants smoke and took cannabis samples for forensic analysis to confirm the presence of the active ingredient THC.
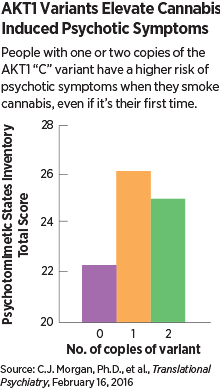
They found that people with the AKT1 variant known as rs2494732 were indeed more likely to show elevated psychotic symptoms like visual distortions or paranoia following cannabis use. The COMT variant showed no association, and the only other variable of any sort that was indicative of acute psychosis was baseline schizoptypal score (the presence of symptoms like social discomfort or odd behaviors).
The analysis also showed that length of cannabis use did not moderate this risk bestowed by the AKT1 variants; that is, long-term users had the same risk of an acute episode as first-time smokers.
Working memory was not affected by variants in either gene, and the only trait linked with memory problems was gender, as women had worse memory performance than men while intoxicated.
While the study did focus on acute psychosis, senior author Val Curran, Ph.D., a professor of psychopharmacology at University College London, noted that acute reactions are considered a good indicator for chronic psychosis down the line.
As for possible mechanisms, AKT1 encodes a protein that happens to be a target of the dopamine D2 receptor (DRD2). The association of the neurotransmitter dopamine with drug use and mental health is well appreciated, and recent research has found that genetic variants in DRD2 are associated with psychosis risk and antipsychotic drug response.
Curran and her colleagues suggested in their paper that people with the AKT1 variant may release excess dopamine when they smoke cannabis, thus increasing the risk of psychotic symptoms. (As an interesting parallel, psychosis is one of the most common side effects of the dopamine-triggering agents used to treat Parkinson’s disease.)
This study was funded by grants from the Medical Research Council UK. ■
“AKT1 Genotype Moderates the Acute Psychotomimetic Effects of Naturalistically Smoked Cannabis in Young Cannabis Smokers” can be accessed
here.