To diagnose a patient with premenstrual dysphoric disorder (PMDD), which is characterized by significant premenstrual changes in mood and behavior that resolve with the onset of menses, it is recommended that clinicians track the frequency, severity, duration, and cycling of a woman’s daily symptoms over a two-month period.
Because obtaining such detailed daily symptom records from patients can be difficult, many clinicians rely on retrospective self-reports from patients; a 2014 survey of 87 practicing physicians found that only 11.5 percent routinely used 60-day monitoring for making a PMDD diagnosis.
“Retrospective reports do seem fine for many conditions, but for some reason we don’t yet understand, we can’t rely on this kind of analysis for PMDD,” said Tory Eisenlohr-Moul, Ph.D., a postdoctoral fellow in reproductive mood disorders at the University of North Carolina (UNC). Additionally, because there are no concrete rules for what constitutes a significant change in mood before and after menstruation, or even what defines a cycle, interpreting the data can be difficult.
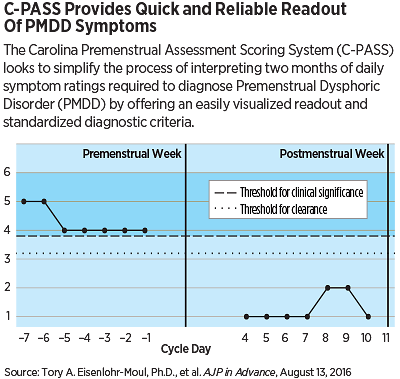
Eisenlohr-Moul and colleagues recently developed a PMDD scoring system that they believe offers a standardized and simplified approach to diagnosing PMDD. They described this system, known as the Carolina Premenstrual Assessment Scoring System (C-PASS), in the August 13 AJP in Advance.
Instead of requiring a clinician to interpret two months of daily symptom data across four diagnostic dimensions (symptoms, severity, cyclicity, and chronicity), clinicians enter the daily symptom ratings provided by the patient over two months, and the program computes whether the patient meets the criteria for a PMDD diagnosis. The program can also be used to determine whether a patient has menstrually related mood disorder (MRMD)—which applies to women who experience distress and impairment sufficient to warrant treatment, but do not meet the full DSM-5 criteria for PMDD.
To field test C-PASS, the team entered two months of daily symptom scores provided by 200 women who had participated in a PMDD study at UNC. They then compared the diagnoses computed by C-PASS with the diagnosis made for these women by David Rubinow, M.D., the Meymandi Professor and Chair of Psychiatry at the UNC School of Medicine, a leading authority on PMDD who helped champion its inclusion in DSM-5.
The C-PASS program identified 38 women with PMDD, 46 with MRMD, and 116 with no diagnosis, which was in agreement with Rubinow’s assessment for 189 of the 200 cases. Among the 11 disagreements, the authors believe that C-PASS was correct in seven of the disagreeing cases going by clinical definitions, while the program made an inaccurate diagnosis in the other four disagreements because it did not adequately measure postmenstrual symptom improvements.
“Overall [the program] performed very well and offers a good starting point toward achieving a consistent diagnosis across clinics and research labs,” Eisenlohr-Moul said. She added that further validation is needed by testing C-PASS in additional patient groups, and her group continues to fine-tune the program based on clinician feedback.
Further down the road, she envisions linking C-PASS with public facing digital tools where women concerned about the possibly having this condition could input their daily symptoms into apps that automatically calculate and send updates on symptoms to their practitioner. Such information could be used to evaluate the condition on a weekly basis, determine whether a diagnosis can be made, or evaluate the effectiveness of treatments.
“There will still be a time lag required for making a proper PMDD diagnosis,” Eisenlohr-Moul said. “But we can streamline the time management portion at least and ease the decision-making process.”
This study was supported by grants from the National Institute of Mental Health. ■
“Toward the Reliable Diagnosis of
DSM-5 Premenstrual Dysphoric Disorder: The Carolina Premenstrual Assessment Scoring System (C-PASS)” can be accessed
here. C-PASS worksheets can be found in a variety of formats
here.