The ability to accurately predict at-risk individuals who will transition to psychosis from those who will not could help clinicians connect patients to care faster. In recent years, researchers have increasingly turned to neuroimaging technology in search of biomarkers for psychosis.
A study by researchers at the University of Alberta in Edmonton and IBM’s TJ Watson Research Center in Yorktown, N.Y., now suggests that differences in brain connectivity may predict not only which patients have schizophrenia, but also the severity of specific symptoms.
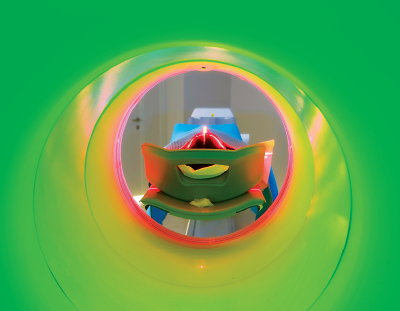
These findings, which were published in NPJ Schizophrenia, came from an analysis of functional MRI (fMRI) scans from 95 people, including 46 patients with schizophrenia or schizoaffective disorder and 49 matched controls.
The participants underwent the fMRI scans while performing a task known as the Auditory Oddball. This test involves listening to a series of repetitive tones and pressing a button whenever a different-pitched, “oddball” tone is heard. This test was chosen because auditory problems are a common schizophrenia symptom.
Using a computational approach known as “link-weighting,” the researchers compared the relative strength of brain activity in patients with schizophrenia with that of controls. Link-weighting involves measuring neural signals (or links) between different clusters in the brain (or nodes).
On average, patients with schizophrenia had greater activity in several brain regions than controls, particularly in links connecting the thalamus and motor cortex.
Based on the differences in link-weights, the researchers could differentiate patients with schizophrenia from controls with 74 percent accuracy. Other predictive studies using brain scans have reached higher accuracies, but study investigator Guillermo Cecchi, Ph.D., director of the computational psychiatry group at IBM Research, noted previous studies employed a single MRI machine for more consistency.
The fMRI images used in this study came from the national Function Biomedical Informatics Research Network Data Repository (fBIRN), which collects scans from a wide range of machines employing different types of imaging software. According to Cecchi, this made comparing images much more challenging.
“That we could reach 74 percent accuracy when working across different sites is actually encouraging,” he said. “There is room to improve, but this is a first step to developing a model for prediction that could really be universal.”
Cecchi and his colleagues also found they could predict the severity of specific symptoms in the schizophrenia patients using the imaging data. They assessed connectivity patterns in relation to patient scores on nine global assessment scales and found five where link-weighting scores were tied to severity: alogia, apathy, attention, bizarre behavior, and formal thought disorder. In contrast, the severity of affective flattening, anhedonia, hallucinations, and delusions did not appear to be associated with these connectivity patterns.
What was interesting, noted Cecchi, is that the neural links that predicted symptom severity were not the same ones that showed the strongest difference between the schizophrenia patients and controls. The areas associated with symptom differences included the sensory cortex and precuneus, a brain region involved in visuospatial processing and self-reflection.
Cecchi thinks this speaks to the complexity of schizophrenia, as neural connections that do not appear predictive of a disordered state greatly affect how symptoms manifest.
This study was supported by IBM, Alberta Innovates Health Solutions, and the Natural Sciences and Engineering Research Council of Canada. The fBIRN is supported by grants from the National Institutes of Health. ■
“Learning Stable and Predictive Network-Based Patterns of Schizophrenia and Its Clinical Symptoms” can be accessed
here.