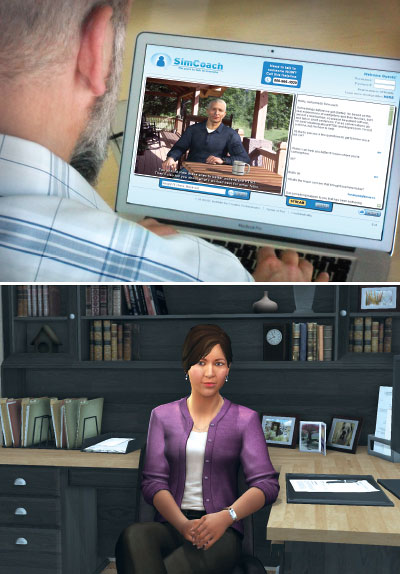
In many respects, Molly Porter is like any other human resources specialist conducting a job interview. She is dedicated, thorough, and knows the right questions to ask. The only difference is that Molly isn’t real; she’s a virtual avatar on a video monitor, and her function today is to help patients recovering from psychosis develop important social skills.
“The stress of an interview can be tough enough for an average job seeker, but that is exponentially magnified in someone coping with a severe mental illness,” Matthew Smith, Ph.D., M.S.W., an associate professor of social work at the University of Michigan, told Psychiatric News. Smith has been exploring the effects of “Molly training” on patients with psychosis and autism, among other groups. “Molly allows a person to practice interviewing without having the pressure of real consequences,” he said.
While role-playing with other people can benefit people with psychosis, virtual reality (VR) training programs offer the advantage of forcing individuals to interact with people who are less familiar, said Skip Rizzo, Ph.D., director for medical virtual reality at the University of Southern California Institute for Creative Technologies. Another perk of VR training is that it can be done at any time.
“Someone without a psychiatric disorder might wonder how beneficial a conversation with a piece of software can be,” Rizzo said. “But these programs create an environment where someone can feel safe.”
Interviews with Molly training last approximately 20 to 30 minutes. Users can adjust Molly’s personality (friendly, professional, or curt) and the level of difficulty of the questions she asks.
To develop a more realistic and natural feel, this software (which was developed by a company known as Simmersion) uses over 2,000 video clips of a real person; an algorithm “listens” to the user’s words and then plays an appropriate response from the archive.
VR Training Improves Communication
The concept of using computer programs to prepare for interviews is not new; programs like Molly training have been used as training modules since the 1990s, though their initial design was to help professionals improve communication in instances such as interrogating a witness or conducting a behavioral therapy session. More recently, researchers have seen the potential for VR programs to help patients as well.
Clinical studies are currently evaluating the ability of VR-based programs to help servicemembers and veterans with posttraumatic stress disorder engage in dialogue about their symptoms, improve communication in people who have had a stroke or traumatic brain injury, and bolster social skills in people with autism.
Pilot work done by Smith and his colleagues has shown that people with psychosis who completed about 10 hours of Molly training sessions had about twice the odds of receiving a job offer after six months compared with patients who did not receive Molly training. The people who used the program also reported that it was helpful and easy to use.
Smith acknowledged that while participants in his study were all in a position in their lives to start job seeking, he thinks similar VR coaching programs could be used earlier in the recovery process as well. “[VR] could be a starting point to get patients engaged in recovery and help them boost fundamental skills like empathy or theory of mind,” he said. (“Theory of mind” refers to the intrinsic understanding that other people possess their own values and beliefs.)
Moving Patients Into Virtual World Not Without Risks
The major concern about using VR earlier in psychosis recovery—where it would be more a therapeutic tool than a skill training tool—is that VR applications might be harmful to people whose symptoms typically include feeling detached from reality, said Lucia Valmaggia, Ph.D., a clinical psychologist and head of the Virtual Reality Lab at King’s College London. “But we conducted some studies using immersive environments and found that when done properly, VR does not increase any feeling of detachment or create other distress. [Patients] understand what is real versus virtual.”
This past March, researchers in the Netherlands published one of the first clinical trials showing that VR-assisted behavioral therapy is not only feasible, but it can help reduce paranoid thoughts and anxiety in patients with psychosis. The VR sessions involved placing the patient in a virtual environment to encourage interaction and eye contact with digital avatars.
“The beauty of VR is that it combines both ecological validity and experimental validity,” said Valmaggia, who in addition to her psychosis research is also exploring VR to help people with eating disorders improve their body image. “You can control the settings to have a well-regulated environment so nothing unexpected occurs, as opposed to taking a person out to a pub to interact.
“Now, every psychiatric therapy has the risk of making the patient’s condition worse, and VR, as an emotionally evocative technology, is no exception,” Rizzo continued. “We have to be careful, so our treatment efforts do not go in the other direction.”
Smith agreed. “There is a lot of excitement in technology-based mental health care, but we have to do our due diligence,” Smith said. “We are taking the approach that interventions aren’t ready for the public until they can be considered an evidence-based tool.”
Developing an evidence base is critical, but Valmaggia wonders how feasible it can be given how quickly VR technology is changing. The gold standard for medications—long-term randomized clinical studies, which can take years from concept to completion—may not be appropriate, since the technology will have moved on, she said.
“It’s a moving target to be sure,” Rizzo said when describing what the goals of psychiatric VR might be. “Remember, this is still a young discipline. … [T]here is still much we don’t know about how people behave in the real world. Now we have to figure out human behavior in virtual worlds.” ■
Smith’s study, “Virtual Reality Job Interview Training and 6-Month Employment Outcomes for Individuals With Schizophrenia Seeking Employment,” can be accessed
here. Valmaggia’s study, “Virtual Reality and Paranoid Ideations in People With an ‘At-Risk Mental State’ for Psychosis,” is available
here. “Virtual-Reality-Based Cognitive Behavioural Therapy Versus Waiting List Control for Paranoid Ideation and Social Avoidance in Patients With Psychotic Disorders: A Single-Blind Randomised Controlled Trial” is located
here.