When economists Anne Casey and Angus Deaton published their landmark 2015 report in the Proceedings of the National Academy of Sciences documenting rising mortality among white, middle-aged Americans, they helped to coin a term: “deaths of despair.”
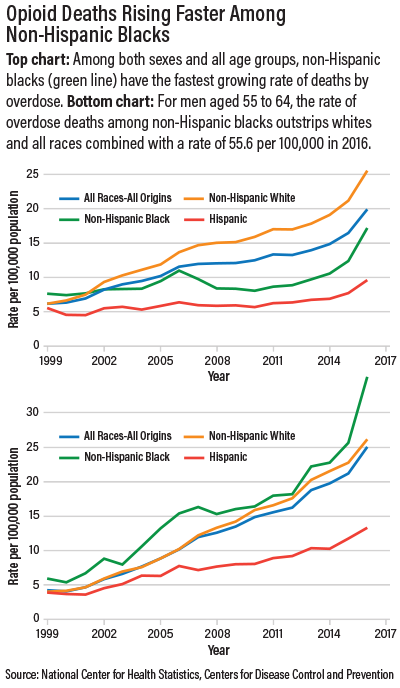
The rising death rate among whites—driven by increasing suicide rates, diminishing overall health, and, especially, the opioid epidemic—was linked, they said, to economic anxiety. In this way did their report help to cement an image already widely prevalent—that the new opioid crisis is a “white” problem affecting white Americans and linked with social and economic causes: decreasing wages, disappearing jobs, and a diminishing standard of living. But recent data from the National Center for Health Statistics show that the fastest rising rate of opioid-related deaths is among African Americans (see chart).
How did the opioid crisis come to be widely regarded as a “white” problem rooted in socioeconomic causes, when drug abuse has plagued inner-city black and minority communities for decades, and the response has been overwhelmingly punitive?
Not by chance, according to Helena Hansen, M.D., Ph.D., vice chair of APA’s Council on Minority Mental Health and Health Disparities.
In an address at the spring educational conference of the Black Psychiatrists of America (BPA) in Memphis in March, she said a conscious and deliberate (and deceptive) strategy by the pharmaceutical industry beginning in the 1990s targeted a vast white suburban and rural market with the introduction of OxyContin as a “minimally addictive” painkiller. This was followed by Food and Drug Administration approval of buprenorphine in 2002 and its marketing to a white audience as a treatment for opioid addiction.
Her remarks were based on her research, funded by the National Institutes of Health and the Robert Wood Johnson Foundation, involving observations and over 200 interviews with pharmaceutical executives, policymakers, addiction scientists, physicians, and patients.
The “whitening” of the new class of opioids occurred against the backdrop of a long history in which heroin and other drugs of abuse were similarly “racialized” as the substances of choice among blacks and other minorities—but with a more sinister, criminal imagery that tended to ignore the socioeconomic conditions that had always contributed to addiction among minority communities.
“While narcotics have long been criminalized through association with marginal racial groups, such as turn-of-the-century images of Chinese opium dens, Negro cocaine fiends in the south, and Mexican marijuana madness, we don’t often look at how this can work in the opposite direction, how a drug can assume ‘whiteness’ within a racialized pharmaceutical logic,” Hansen said. “The current generation of opioids was designed to have white racial identities, and in our stratified health care and justice systems, the biotechnologies and social technologies shaping opioid consumption reinforce racial inequalities while at the same time harming whites.”
How Racial Disparities Developed
In her address at the BPA and in comments to Psychiatric News after the meeting, Hansen said there are three components to the way in which drugs of abuse generally have been “racialized” and how prescription opioids, specifically, have been made “white.” These components include deliberate ethnic marketing by the pharmaceutical industry, the attraction of a “magic bullet” solution for addiction that obscures the psychosocial and economic factors in addiction, and a health system in which treatment—especially psychosocial treatment—is unequally accessible according to geography, race, and class.
“In 1996 the FDA accepted the claim that the addictive potential of OxyContin was ‘less than 1 percent,’ enabling Purdue Pharmaceuticals to open an opioid market that had previously been restricted to those with severe acute pain to a new, much larger market of patients with moderate, chronic pain,” Hansen said. “Purdue targeted generalists in white suburban and rural areas, serving patients that the public and the Drug Enforcement Agency (DEA) did not think of as at high risk of addiction and drug trade.”
The strategy, she said, led to a tenfold increase in prescription opioids nationally, with the disproportionate uptake of OxyContin by prescribers in white suburban and rural areas of states like Maine, Ohio, Kentucky, and West Virginia. The technological response by Purdue to the first wave of white prescription opioid overdose deaths—tamper-resistant formulations of oxycodone—combined with new prescription drug monitoring programs led many of these legal OxyContin users to look for heroin when pills became hard to get, creating a new class of addicts. “Most of these newly addicted people were white and many of them middle to upper income,” Hansen said.
In response to this new category of addicts, the FDA approved the synthetic opiate buprenorphine (commercially packaged as Suboxone) for maintenance treatment of opiate dependence in the private offices of buprenorphine-certified physicians. It marked a novel approach to the treatment of opioid dependence, in stark contrast to the tightly regulated use of methadone in clinics located disproportionately in inner-city neighborhoods of color.
“Pharmacologically similar to methadone in that it blocks opiate receptors in the brains of addicted patients, buprenorphine can be prescribed monthly for use at home, while methadone is restricted to DEA-regulated clinics with directly observed dosing,” Hansen said. “To accomplish this, the manufacturers of buprenorphine and the architects of buprenorphine policy had to distinguish buprenorphine symbolically and spatially from methadone.”
A not atypical ad for Suboxone showed “Mike,” seated in his Ohio diner. He is flanked by American flags, talking about returning to coaching his son’s baseball team and singing in the church choir after buprenorphine rescued him from a prescription opioid habit following a back injury. In this way was opioid addiction and its treatment rendered “white.”
Hansen argued further that trends in neuroscience had the effect, however unintended, of underscoring the “whitening” of the opioid epidemic. The Decade of the Brain promoted the idea of addiction as a brain disease, stripped of its environmental, socioeconomic, and psychosocial context, with the message that “anyone” could become an addict.
Problem Demands Psychiatric Response
Hansen acknowledges the beneficent motive in this, intended to counter the idea of addiction as a moral failing. But in a majority white culture, Hansen said, “anyone” was code for “white”—in contradistinction to addicted persons of color, long associated with heroin and street drugs traded criminally in urban communities.
Finally, this racial and geographic segmentation is further aggravated by grossly unequal access to care, she said.
The “white” opioid epidemic today has raised to prominence, in a new way, the importance of underlying socioeconomic influences, never adequately acknowledged when addiction was regarded as a criminal problem of people among communities of color. “Now that the image of the addicted white unemployed rust belt worker is circulating in the press, we have to lobby for economic revitalization, especially in communities of color, which have long been dying from the drug trade as an economy of last resort,” Hansen said.
She added that the opioid crisis and the national response to it “tap into our conflicting cultural logics about whether addiction is a moral, social, or biological problem.”
It’s an area that demands a psychiatric response. “The excitement has been around addiction medication with the fantasy that this would preclude the need for mental health care and psychosocial support, which has never been as popular,” she said. “We have refused to recognize that addiction is rooted in social problems mediated by mental illness. Psychiatrists have to get into this arena—we are faced now with a whole generation of patients in need of mental health treatment.” ■
The Casey and Deaton report, “Rising Morbidity and Mortality in Midlife Among White Non-Hispanic Americans in the 21st Century,” can be accessed
here. The National Center for Health Statistics report, “Drug Poisoning Mortality in the United States 1999-2016,” is available
here.