Screening for Allele Could Cut Incidence of Carbamazepine Skin Rashes
Patients with the rare allele HLA-B*15:02 are known to be at a greater risk of carbamazepine-induced Stevens-Johnson syndrome (SJS), a severe skin rash. Because of this risk, the Food and Drug Administration (FDA) recommends that patients with ancestry from areas where HLA-B*15:02 is prevalent should undergo genetic screening before starting treatment with carbamazepine.
A study published in JAMA Neurology now shows that screening for the related HLA-A*31:01 allele, which is more common than HLA-B*15:02, may also be clinically useful. Investigators in Japan screened 1,130 patients who were prescribed carbamazepine for epilepsy, schizophrenia, bipolar disorder, or other conditions for HLA-A*31:01. The 198 patients who tested positive for HLA-A*31:01 were prescribed alternative medications.
The investigators identified 23 cases of adverse skin reactions in this population, resulting in a 2 percent incidence rate. Historical medical data reported a 3.4 percent rate in people taking carbamazepine or related drugs, meaning the screening reduced the number of adverse reactions by about 40 percent.
“Although cost-effectiveness analyses are required, the use of HLA-A*31:01 screening to reduce the rate of carbamazepine-induced cADRs [cutaneous adverse drug reactions] in routine clinical practice appears to be warranted,” they wrote.
Liver Cancer Linked To Alcohol Found to BeMore Lethal
Patients with alcohol-related liver cancer often do not live as long as patients with liver cancer that is not associated with alcohol consumption, according to a study in Cancer. The finding highlights the importance of regular liver screenings in patients with alcohol use disorder.
Investigators from Henri Mondor Hospital in Crȳteil, France, and colleagues tracked the health outcomes of 894 patients with newly diagnosed liver cancer for five years; 65 percent of the participants had a history of chronic alcohol misuse.
At the end of five years, the researchers found that the average survival time was 9.7 months in patients with non-alcohol-related cancer and 5.7 months in patients with alcohol-related cancer. Among the patients with an alcohol history, those who were abstinent from drinking at the time of enrollment had slightly better survival rates (5.8 months versus 5.0 months for non-abstinent patients).
When the patients were matched based on the stage of liver cancer at the time of diagnosis, the survival rates were similar between the two groups. The findings suggest that the reduced overall survival in patients with alcohol-related liver cancer may be due to these patients having worse liver function and cancer that was more spread out and diffuse at the time of diagnosis.
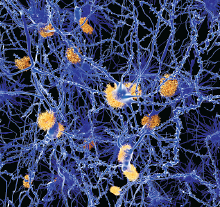
Alzheimer’s Protein Implicated in HIV-Associated Neurocognitive Problems
BACE1, a protein involved in Alzheimer’s disease, may be a promising target for treating cognitive problems related to the human immunodeficiency virus (HIV), suggests a study published in the Journal of Neuroscience.
Although patients with HIV-associated neurocognitive disorders (HAND) and Alzheimer’s have many symptoms in common, it is unclear if these diseases share any similar biological mechanisms. The brains of patients with HAND do not exhibit the amyloid plaques that are found in the brains of patients with Alzheimer’s, but there is some evidence that HAND is associated with alterations in how amyloid fragments are processed.
Researchers at the University of Pennsylvania and colleagues analyzed BACE1 and amyloid oligomers in postmortem brain tissue of patients who were HIV-positive. They found elevated levels of BACE1 and amyloid oligomers in this tissue, but as expected, no evidence of amyloid plaques. When they treated neurons growing in a lab dish with material from HIV-infected white blood cells, the researchers discovered that the neurons started producing more BACE1, eventually reaching toxic levels.
This BACE1 production was dependent on signaling from NMDA receptors, which suggests that inhibiting NMDA and glutamate signals may be a therapeutic option to treat HAND.
Metformin Found to Block Symptoms of Acute Nicotine Withdrawal
An animal study appearing in Proceedings of the National Academy of Sciences suggests that the type 2 diabetes drug metformin can block the symptoms of nicotine withdrawal. If similar effects of the medication are found in smokers, the medication could offer a potential new therapeutic option for smoking cessation, as current medications focus more on preventing nicotine cravings.
For the study, researchers at the Johns Hopkins University School of Medicine and colleagues targeted an enzyme known as AMP-activated protein kinase (AMPK). They found the AMPK pathway is activated in mammals following chronic nicotine use but becomes repressed during nicotine withdrawal. The researchers hypothesized that this shift might contribute to withdrawal symptoms such as anxiety and irritability.
They next tested whether providing metformin—which stimulates AMPK production—prior to nicotine withdrawal might keep the AMPK pathway active once smoking stopped. The researchers found that mice given one week of pre-withdrawal metformin injections still had detectable levels of active, phosphorylated AMPK 24 hours after nicotine withdrawal, whereas mice treated with saline did not. The mice who received metformin also showed almost no anxiety-like behaviors in a pair of behavioral tests 24 hours after nicotine withdrawal.
The researchers noted that these results were achieved using metformin concentrations (250 mg/kg) that did not impact the body weight, food consumption, or glucose levels of the mice under both fed and fasted conditions. ■