Eczema Associated With Increased Suicidality
People with atopic dermatitis—also known as eczema—appear to be more likely to think about and attempt suicide than those without this condition, suggests a meta-analysis in JAMA Dermatology.
Eczema is an inflammatory disease characterized by dry, cracked, and scaly patches of skin. Previous studies have found patients with eczema are at a greater risk of anxiety and depression, but whether these patients are at an increased risk of suicide was unknown.
The meta-analysis by researchers at the University of Southern California incorporated 15 studies, which included over 310,000 eczema patients and 4 million control subjects. The analysis revealed that patients with eczema were 44 percent more likely to exhibit suicidal ideation and 36 percent more likely to attempt suicide compared with patients without eczema. There were not enough data to identify the increased risk, if any, of completed suicides. “In studies comparing patients with mild AD [atopic dermatitis] versus patients with moderate to severe AD, patients with moderate to severe AD were found to have a higher prevalence of suicidal ideation but not completed suicides,” the authors wrote. “Greater disease severity of AD is associated with increased sleep loss, more severe pruritus, and higher depression and anxiety rates, which can all contribute to more suicidal ideation.”
However, the authors cautioned that there is a shortage of data on subpopulations, and more research is needed to better understand the associations between eczema and suicidal behaviors.
Possible Mechanism Identified for Cognitive Symptoms in Schizophrenia
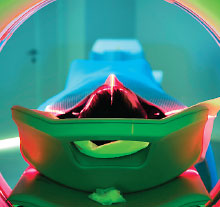
Using positron emission tomography (PET) scans to image patient brains, researchers at Massachusetts General Hospital have uncovered molecular differences that may explain why people with schizophrenia have cognitive difficulties. They observed that key regulatory proteins known as histone deacetylases (HDACs) were present at different levels in the brains of patients with schizophrenia relative to healthy controls.
Reduced HDAC levels had previously been observed in postmortem brain samples from patients with schizophrenia, but this is the first evidence of HDAC deficiency in living individuals. The findings were published in the Journal of Clinical Investigation.
The researchers scanned the brains of 14 individuals with schizophrenia or schizoaffective disorder as well as 17 healthy controls, using a specially designed tracer that radioactively tags HDACs. The scans showed that HDAC expression was significantly reduced in the prefrontal cortex (which regulates working memory, planning, and flexibility) of schizophrenia patients compared with controls. Patients who had less HDAC also had more severe cognitive problems on average.
Unexpectedly, the researchers found that HDAC levels in schizophrenia patients were higher than controls in other brain regions linked with cognition, such as the cerebellum. “These data may suggest that abnormal HDAC expression, in either direction, could have negative effects on cognition,” the researchers wrote.
Overdose Death Data Illuminate Toll of Opioids
Between 2011 and 2016 opioids, benzodiazepines, and stimulants dominated the list of top 10 drugs most frequently involved in overdose deaths, according to a National Vital Statistics Report published in December 2018.
While the ranking of the individual drugs changed from year to year, the top 10 drugs involved in overdose deaths remained consistent throughout the six-year period, according to the analysis conducted by investigators at the National Center for Health Statistics and the Food and Drug Administration. The top 10 drugs included alprazolam, cocaine, diazepam, fentanyl, heroin, hydrocodone, methadone, methamphetamine, morphine, and oxycodone.
Among this group, fentanyl-related deaths showed the most drastic rise, going from 10th most common cause of overdose death in 2011 (about 1,600 overdose deaths) to the top spot in 2016. Over 18,000 overdose deaths in 2016 involved fentanyl—nearly 29 percent of all overdose deaths. The report also revealed that 69 percent of the time when fentanyl was involved in an overdose death, another drug was also found in the person’s system, most often heroin or cocaine.
Overall, the number of drug overdose deaths per year increased by 54 percent during the study period, going from 41,340 in 2011 to 63,632 in 2016. Methadone was the only drug for which total overdose deaths declined during the study, dropping from about 4,500 deaths in 2011 to 3,500 deaths in 2016.
Financial Difficulties Impacting Purchase of Food Linked to Binge Eating
People with limited finances can experience food insecurity—problems being able to afford enough food to support a regular, balanced diet. A study appearing in the International Journal of Eating Disorders reports that food insecurity is associated with higher rates of binge eating disorder (BED). This finding may help explain the observed links between food insecurity and obesity, the authors noted.
Researchers at Yale University surveyed 1,250 adults online about their weight, eating habits, and perceived food security.
They found that adults who reported having low food security (they had to adjust the quality, variety, or desirability of their food purchase to satisfy hunger) or very low food security (they had to adjust food purchases but still went hungry at times) were more likely to have BED symptoms than those with adequate food security. Among respondents who reported BED symptoms, 28.2 percent reported low food security, and 18.9 percent reported very low food security. Participants with very low food security were also more likely to be obese than those in the other two groups.
The “[r]esults highlight the need to devote resources toward policy revisions, preventative interventions, and psychiatric treatments aimed at decreasing the overall association of food insecurity with BED and obesity among low-income Americans,” the authors wrote.
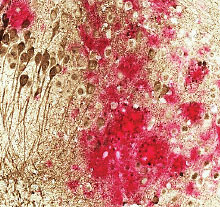
DNA Vaccine Reduces Accumulation of Alzheimer’s Proteins in Mice
Researchers at the University of Texas Southwestern Medical Center have developed a DNA-based vaccine that reduces the accumulation of two toxic proteins associated with Alzheimer’s disease in mice.
Whereas traditional vaccines inject protein fragments (antigens) into the body so the immune system can make antibodies, a DNA vaccine injects pieces of DNA under the skin, which are then made into antigens inside the body.
For the study, the researchers injected either a DNA vaccine they created or a traditional amyloid vaccine into mice that were genetically modified to develop Alzheimer’s disease. Beginning at four months of age through 20 months, the mice received 13 vaccinations.
An analysis of the mouse brain tissue showed that the DNA vaccine reduced amyloid-b levels by up to 40 percent and tau levels by up to 50 percent, with no adverse side effects. The DNA vaccine removed about twice as much amyloid-b and four times as much tau as the traditional vaccine, despite the traditional vaccine producing 10 times as many antibodies.
This study was published in Alzheimer’s Research & Therapy.
Rosenberg RN, Fu M, Lambracht-Washington D. Active Full-Length DNA Aβ42 Immunization in 3xTg-AD Mice Reduces Not Only Amyloid Deposition But Also Tau Pathology? Alzheimers Res Ther. 2018; 10(1):115.