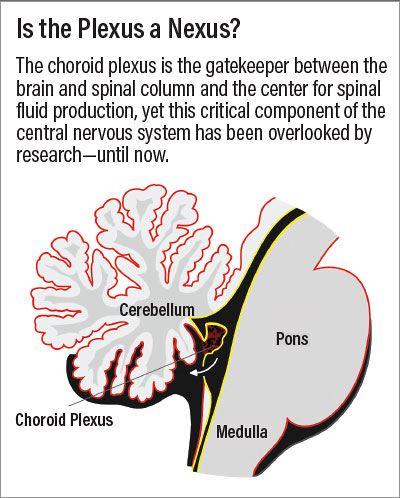
In 1921, researchers first proposed a link between psychosis and abnormalities in the choroid plexus—a cluster of cells and blood vessels at the base of the brain responsible for making cerebrospinal fluid (CSF) and maintaining a barrier between the brain and spinal column. But since then, little research has examined this link. Now a study in the July issue of The American Journal of Psychiatry has brought this brain region back into the fold.
The study, which involved an analysis of over 1,300 brain scans, found that the choroid plexus is significantly larger in patients with psychosis compared with their relatives or healthy people without psychosis. This analysis included patients with multiple psychotic disorders, which suggests choroid plexus enlargement may be a common trait shared across the psychosis spectrum.
Paulo Lizano, M.D., Ph.D., an instructor of psychiatry at Harvard Medical School, and colleagues analyzed MRI scans from participants in a nationwide psychosis study called B-SNIP. The sample included 223 patients with schizophrenia, 141 with schizoaffective disorder, and 190 with psychotic bipolar disorder. The researchers also analyzed the brain scans of 564 first-degree relatives without psychosis and 333 unrelated adults, also without psychosis.
The comparison of scans showed that the choroid plexus was significantly enlarged in patients with a psychotic disorder relative to healthy controls, with family members falling in between. The increased choroid plexus volume was about the same regardless of whether the patients had schizophrenia, schizoaffective disorder, or bipolar disorder.
What’s more, greater choroid plexus volume correlated with worse performance on cognitive tests in these patients, particularly in verbal fluency tests (in which patients have to provide as many words as possible in a certain category in a given time). Choroid plexus volume did not correlate with the severity of other psychosis symptoms like delusions or social withdrawal, however, suggesting that this abnormality specifically affects cognition.
Since the analysis was based on MRI scans taken at a single point in time, Lizano cautioned that it is too early to determine whether the choroid plexus enlargement is a cause or consequence of psychosis or what mechanisms might contribute to the enlargement.
However, as part of this study, the investigators also analyzed the composition of inflammatory proteins in blood samples that were available from 107 B-SNIP participants with psychosis and 52 healthy participants. This additional analysis revealed that patients with larger choroid plexuses also had elevated blood levels of the inflammatory biomarker interleukin 6 (IL-6). Several previous studies have found a connection between elevated levels of IL-6 and schizophrenia.
“This suggests inflammation is part of the [disease] process [in psychosis], but we are in the early stages of this work and want to be cautious in how we interpret these findings,” Lizano told Psychiatric News. “However, the excitement in how neuroinflammation contributes to psychosis has ignited interest in [both] the choroid plexus and how it is involved in brain homeostasis.” He hopes the findings from this study will inspire a vibrant new field of choroid plexus research—only 100 years in the making.
This study was supported by grants from the National Institute of Mental Health, National Center for Advancing Translational Sciences, the Commonwealth Research Center, and a Livingston Award from Harvard Medical School. ■
“Association of Choroid Plexus Enlargement With Cognitive, Inflammatory, and Structural Phenotypes Across the Psychosis Spectrum” is posted
here.