Riluzole Augmentation May Reduce Hyperarousal Symptoms
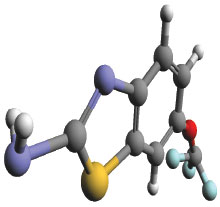
Augmenting antidepressant therapy with the glutamate modulator riluzole may help reduce hyperarousal symptoms in people with combat-related posttraumatic stress disorder (PTSD), according to a new report in the Journal of Clinical Psychiatry.
Researchers at the Uniformed Services University of the Health Sciences in Bethesda, Md., and colleagues conducted a clinical trial involving 74 active-duty service members or veterans with combat-related PTSD who had not responded to treatment with a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI). The participants were randomized to take riluzole (starting at 100 mg/day) or placebo in addition to SSRIs or SNRIs for eight weeks. The researchers assessed the participants’ PTSD symptoms, anxiety, depression, and overall disability weekly.
After eight weeks, the groups did not differ in overall PTSD symptom improvements as demonstrated by changes in scores on the PTSD Check List (PCL) or Clinician Administered PTSD Scale (CAPS). However, participants taking riluzole showed superior improvement specifically in hyperarousal symptoms (subscale D on both the PCL and CAPS). For example, PCL-D scores dropped 5.9 points in the riluzole group compared with 3.4 points in the placebo group after eight weeks. Riluzole was not superior to placebo for the other outcomes assessed.
Though the study focused on military personnel, “hyperarousal may have negative social and occupational consequences in civilian life too, so this augmentation strategy may hold promise for a wide range of persons suffering from residual PTSD symptoms,” said co-author and psychiatrist Col. David Benedek in a press release.
Children Report Worsening of OCD Symptoms Since Start of Pandemic
Investigators at Aarhus University Hospital in Denmark have found that the COVID-19 pandemic has exacerbated obsessive-compulsive disorder (OCD) symptoms in many children and adolescents. The analysis was published in BMC Psychiatry.
The investigators assessed survey data collected between April and May from two sets of youth aged 7 to 21 with OCD: 65 who had been recently diagnosed with OCD and were receiving treatment and 37 who had previously been diagnosed with OCD and completed treatment.
Overall, 45% of the newly diagnosed youth and 73% of the previously diagnosed youth reported increased severity of their OCD symptoms following the outbreak of COVID-19.
In both groups, youth who exhibited unwanted aggressive or sexual thoughts were more likely to exhibit any post-COVID worsening. When assessing youth whose symptoms worsened, those who had an early age of OCD onset and those with a family history of attention-deficit/hyperactivity disorder reported the greatest changes in symptom severity.
Interestingly, the investigators identified no impact of COVID-19 on children with cleanliness-related symptoms. They hypothesized that children with cleanliness symptoms may have felt more secure seeing their family wash hands or use sanitizer more regularly.
“On the contrary, under the circumstances where the media made daily reports on the number of severely ill or the number of persons who died from COVID-19 infection (even younger persons), these youngsters may be more affected by aggressive thoughts or worries that their parents or their grandparents could become ill or even die,” they wrote.
Apathy May Increase Risk of Dementia in Older Adults
Though numerous studies have focused on how depression may increase dementia risk, a study in Neurology now suggests severe apathy later in life—independent of depression—is also a factor. Older adults with severe apathy later in life were nearly 80% more likely to develop dementia than adults with low apathy.
A team at the University of California, San Francisco, assessed data from 2,018 adults aged 70 to 79 who participated in the Health, Aging, and Body Composition (Health ABC) study. The participants, who did not have dementia at the start of the study, were grouped into three categories based on their responses to a modified version of the 15-point Apathy Evaluation Scale: low apathy (38% of participants), moderate apathy (37% of participants), and severe apathy (25% of participants).
Over a nine-year follow-up period, 381 participants developed probable dementia (25% of the severe apathy group, 19% of the moderate apathy group, and 14% of the low apathy group). After adjusting for several variables (including race, age, smoking, cardiovascular history, and clinical depression), adults with severe apathy had nearly 1.8 times the risk of dementia compared with adults with low apathy. Adults with moderate apathy had about 1.3 times the risk of dementia compared with those with low apathy, but this risk was no longer statistically significant after adjusting for depression.
“As apathy is typically clinically apparent and highly distressing to family, a brief evaluation of apathy may be a helpful tool to identify older adults at increased risk of dementia,” the authors wrote.
Cannabis Fails to Reduce Use of Opioids, Study Suggests
Some observational studies have suggested that the legalization of cannabis has helped reduce opioid-related hospitalizations and deaths, as people substitute opioids with cannabis when treating pain. A study published in Addiction suggests people were more likely to use opioids illicitly on days they used cannabis. Researchers at Columbia University and the New York State Psychiatric Institute examined data from 211 adults in the greater New York metropolis with at least one substance use disorder. As part of the study, participants were asked to call or text into an interactive voice system to answer questions about their substance use for 90 days. At the start of the study, the participants also reported on their current levels of pain.
The researchers looked for trends in the participants’ cannabis and/or opioid use over 90 days in association with their reported pain. They found that adults who used opioids were 1.86 times as likely to use them on days they also used cannabis, and this was true regardless of their baseline pain levels or severity of their opioid use disorder.
“While this study bears replication with other populations, the results suggest that cannabis is not an effective means of limiting non-medical opioid use and casts doubt on this potential therapeutic indication,” the researchers wrote.
COVID-Related Xenophobia Found to Impact Mental Health
Numerous polls have shown that the emergence of COVID-19 has renewed racist stereotypes and xenophobia toward Chinese Americans (also known as Sinophobia). A study published in Pediatrics has identified that this racial discrimination has worsened the mental health of many Chinese American adults and youth.
Researchers at the University of Maryland, Baltimore County, and colleagues surveyed 543 U.S. parents (mostly mothers) who identified as Chinese with children aged 4 to 18, as well as 230 of their children (those aged 10 and older). The participants were asked whether they felt they had personally been the target of in-person or online racial discrimination due to COVID-19 (direct discrimination) or whether they felt their group had (vicarious discrimination). The participants were also asked questions about mood symptoms and overall well-being.
Nearly half of the parents and youth reported being directly targeted by COVID-19-related racial discrimination in person or online, while more than three-quarters reported vicarious discrimination through what they heard or read. In addition, about half of the parents and youth reported that they believed the media perpetuated Sinophobia.
Direct or vicarious discrimination or Sinophobia was associated with increased depressive or anxiety symptoms in adults. In youth, discrimination and Sinophobia were associated with increased anxiety and internalizing symptoms (such as social withdrawal and sadness), but only Sinophobia was associated with externalizing problems such as hyperactivity or conduct issues.
“Our results suggest that 18.7% to 23.91% of [Chinese American] youth had a slightly elevated to substantial risk of clinically significant mental health problems; these percentages are higher than the U.S. norm,” the authors wrote. “Health care professionals must attend to the racism-related experiences and mental health needs of Chinese American parents and their children throughout the COVID-19 pandemic via education and making appropriate mental health referrals.” ■
Cheah CSL, Wang C, Ren H, et al. COVID-19 Racism and Mental Health in Chinese American Families. Pediatrics. 2020. 46(5):e2020021816.