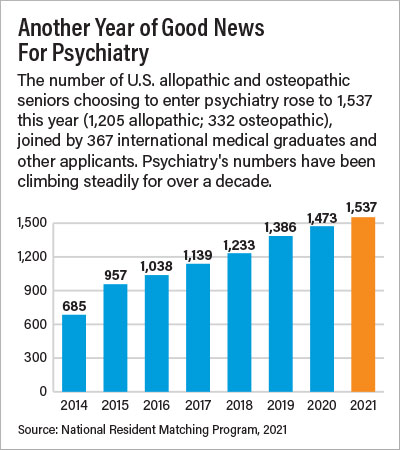
A total of 1,537 U.S. senior medical school graduates—1,205 from allopathic and 332 from osteopathic schools—matched into psychiatry residencies during this year’s National Resident Matching Program (NRMP). That’s up from 1,473 last year.
Additionally, 367 international medical graduates and other applicants also matched into psychiatry, bringing the total to 1,904 medical school graduates. Only three positions went unfilled.
Psychiatry’s numbers have been increasing yearly since 2011-2012, and this year’s increase over 2020 was greater than that of all other specialties. The percentage of allopathic graduates matching in psychiatry rose to 6.5%—10 years ago it was 4.1%.
“Psychiatry is clearly becoming more popular with medical school graduates, and that is certainly welcome news given the enormous unmet psychiatric need today, especially in the wake of the COVID-19 pandemic,” said APA Director of Education Tristan Gorrindo, M.D. “Medical students today recognize psychiatry as the medical specialty that integrates mind, brain, and body.”
Gorrindo urged program directors and mentors to educate trainees about the benefits of membership in APA; residents can visit the
APA website for information and resources that APA offers to residents.
The NRMP is sponsored by the American Board of Medical Specialties, the AMA, the Association of American Medical Colleges (AAMC), the American Hospital Association, and the Council of Medical Specialty Societies.
“From 2011 to 2021, the number of U.S. allopathic seniors applying to psychiatry has nearly doubled, from 640 to 1,205 in 2021,” said Michael Travis, M.D., president of the American Association of Directors of Psychiatric Residency Training (AADPRT). “This represents a jump from 4.1% of all U.S. allopathic seniors to 6.5%. No other core specialty has seen a similar increase. The reasons for this are multifaceted, but I think it represents a recognition that psychiatry is both a holistic and a lifetime specialty. We have opportunities to coordinate all parts of our patients’ care and do this across our patients’ life span.”
Travis told Psychiatric News that a common theme in personal statements the last few years has been “Whatever specialty I rotated through in my 3rd year, psychiatric issues had a major effect on etiology and outcome of the patients’ presenting condition.”
He added, “I also think that the increased interest in psychiatry reflects a greater understanding of psychiatric neuroscience and how this relates directly to what we say to our patients and their families, and our patient management decisions. With medications like brexanolone, we are entering an era of pathophysiologically based treatments for psychiatric illnesses. It is an exciting time to be going into the field, and I think psychiatrists and the organizations to which we belong are doing a great job of communicating this excitement.”
Wide Range of Options Offered
Sallie DeGolia, M.D., president-elect of AADPRT, offered similar comments. “I would love to think that the stigma around psychiatry has significantly decreased and no longer is a barrier to students selecting our field, but it still exists,” she told Psychiatric News. “I do think the intense interest in neuroscience over the past decade plays a role in students’ interest in the field. I am also hoping that we are communicating better with undergraduate medical educators and medical students around the enormous value of seeking a career in psychiatry—we are increasingly the one field that truly bears witness to the patient’s internal suffering and their conflicts and can promote meaningful change through longitudinal relationships.”
She added that as issues around physician wellness have become prominent, psychiatry has likely become more appealing.
“Not only are we probably more family friendly and flexible than other fields, but we have intentionally supported the mental health of our residents,” DeGolia said. “We are a diverse field so finding meaning, which mitigates burnout, is not difficult. We can work in a variety of settings and pursue many interests—teaching, research, clinical, leadership, program development, advocacy.”
Sidney Weissman, M.D., a past APA trustee and past president of AADPRT, said events of the past year may have heightened the interest in psychiatric careers.
“The murder of George Floyd has focused us on the catastrophic impact of racism on our fellow citizens’ well-being,” he said. “At the same time, COVID-19 has made all Americans aware of the importance of mental health, and we are experiencing as a society a greater concern about mental health and wellness.”
Weissman noted as well that the past year has been a unique one for graduates. Since March 2020 classes and clinical work have generally been by Zoom, and students in many schools were not allowed to take elective clerkships other than at their home institution. Residency interviews happened almost entirely by video.
New Guidance Intended to Help Incoming Residents
Because of the sweeping changes the pandemic brought about for medical education, four leading medical education groups published “Transition in a Time of Disruption: Practical Guidance to Support the Move From Undergraduate Medical Education to Graduate Medical Education.”
The guidance—published by the American Association of Colleges of Osteopathic Medicine, the AAMC, the Accreditation Council for Graduate Medical Education, and the Educational Commission for Foreign Medical Graduates—is intended as a toolkit for institutions seeking to help an incoming class of interns that has had an unprecedented experience in undergraduate medical training.
The resource was created by a work group with members from the undergraduate-to-graduate medical education continuum and is divided into three sections: a framework and list of questions medical schools, residencies, and learners should review during this transition; a matrix of possible activities to help learners and residency programs implement a successful transition; and a compendium of resources to support the transition for both learners and programs.
The document includes a statement from the medical student members of the work group. “It should come as no surprise to hear that our final year of medical school was unlike that of any class that came before us,” they wrote. “The global pandemic disrupted clerkships, cancelled electives, rescheduled exams, and moved residency interviews online. More gravely, some of us lost loved ones, friends, and maybe suffered illness ourselves. Now, as we look forward to the transition to residency, we once again find ourselves in uncharted territory, preparing to begin the next phase of our careers amid uncertainty of an ongoing global pandemic and following an interview cycle like none before.” ■
Information about the NRMP and the 2021 data are
here.
“Transition in a Time of Disruption” is posted
here.