Deaths by suicide declined by almost 6% from 2019 to 2020, according to a report in JAMA based on data from the Centers for Disease Control and Prevention (CDC).
The decline is good news in an otherwise grim report that revealed a 17.7% increase in overall deaths in 2020, with most of those directly attributable to COVID-19.
“The reported decrease in deaths by suicide makes us hopeful that protective mental health measures are having a positive impact amid a time of collective distress,” said Christine Moutier, M.D., chief medical officer for the American Foundation for Suicide Prevention (AFSP), in a statement. “While we don’t know the exact contributors to the reported decline in suicides, research does show us that prioritizing and having open, honest dialog about mental health on the individual and national levels, implementing practices that reduce suicide risk in clinical and community settings, and seeking help early and when indicated can reduce suicide deaths.”
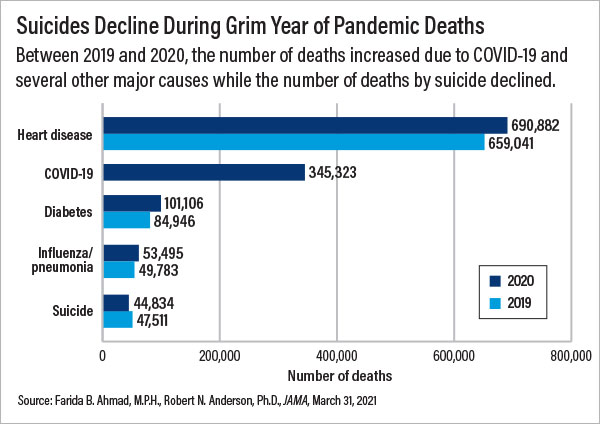
In the JAMA report, Farida B. Ahmad, M.P.H., and Robert Anderson, Ph.D., of the CDC’s National Center for Health Statistics looked at deaths that occurred from January through December 2020, as reported in the National Vital Statistics System. A total of 44,834 deaths by suicide occurred in 2020, a decrease of 5.6% from the 47,511 suicides in 2019. In contrast, the overall number of deaths increased by 503,976 (17.7%) in 2020, with 345,323 of those attributable to COVID-19.
While the reported decline in suicide deaths is encouraging, Moutier cautioned that much remains unknown about the impact of COVID-19 on suicides. “Suicide is complex, risk is dynamic, and an individual’s personal risk factors combined with precipitants such as evolving experiences with isolation, depression, anxiety, economic stress, suicidal ideation, and access to lethal means may lead to periods of increased risk,” the AFSP statement noted.
Importantly, the decrease in the total number of suicide deaths could possibly mask increases among subgroups that have been disproportionately affected by the pandemic. “We do not yet have the data to consider suicide in specific populations based on demographic factors such as age, gender, and racial/ethnic background or social determinants such as income, access to health care, and stressors that minoritized communities may experience,” Moutier said. “Additionally, we know there can be a time lag in the manifestation of distress even months after the acuity of a traumatic or stressful period is over.”
AFSP President Maria A. Oquendo, M.D., Ph.D., who also is a past APA president, agreed and noted especially the increase documented in a 2019
Pediatrics report on Black adolescents showing that suicide attempts rose by 73% between 1991 and 2017, and injury by attempt rose by 122% (
Psychiatric News).
“The data for 2020 are not yet available, but increases in suicide rates among Black youth and other minority populations in the prior few years require attention,” Oquendo told Psychiatric News.
Regarding the overall drop in suicide in 2020, Oquendo said it is not entirely surprising that people are less likely to die by suicide in the wake of a collective, community trauma.
“Suicidologists have long observed that suicide rates tend to decline after a catastrophe,” she said. “The reason is unknown, but some hypotheses include the possibility that individuals become more externally focused given the environmental threat, that the community cohesion that sometimes follows catastrophe has beneficent effects, or that community suffering makes personal suffering more tolerable.”
Beyond the encouraging overall decrease in suicide, the JAMA report is a stark portrait of the grim toll the pandemic has taken on the American population. Along with the more than 345,000 known COVID-19 deaths in 2020, increases were also noted for several other leading causes of death (see chart).
“These increases may indicate, to some extent, underreporting of COVID-19—that is, limited testing in the beginning of the pandemic may have resulted in underestimation of COVID-19 mortality,” the authors wrote. “Increases in other leading causes, especially heart disease, Alzheimer disease, and diabetes, may also reflect disruptions in health care that hampered early detection and disease management. Increases in unintentional injury deaths in 2020 were largely driven by drug overdose deaths. Final mortality data will help determine the effect of the pandemic on concurrent trends in drug overdose deaths.”
They added: “The effects of the pandemic are likely to continue through 2021 as well because COVID-19 has already caused more than 100,000 deaths this year. However, the effects of COVID-19 on mortality trends may be mitigated in 2021 given better detection and treatment options as well as increasing natural and vaccine-related immunity.” ■
“The Leading Causes of Death for the U.S. in 2020” is posted
here.