Researchers Uncover Mechanism Underlying Autoimmune Encephalitis
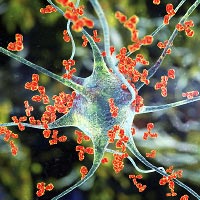
Autoimmune encephalitis is a rare but severe neurological disorder in which antibodies attack receptors in the brain, leading to psychosis, movement disorders, and seizures. Investigators at the University of Texas Southwestern Medical Center and colleagues used advanced microscopy to visualize for the first time how autoantibodies attach to and disable GABA-A, a receptor that works to calm down excited neurons. Their findings were published in Cell.
The investigators used an approach called cryo-electron microscopy (cryo-EM) to develop a 3D map of a GABA-A autoantibody (acquired and purified from an 8-year-old patient with autoimmune encephalitis) attached to the receptor.
The model revealed that the autoantibodies bind to the GABA-A receptor in two distinct spots that inhibit function, resulting in overexcited neurons. One antibody attaches to the GABA-A binding pocket but does not activate the receptor, locking it in what the investigators called a “resting-like state.” Another antibody attaches to a side area of the receptor that is typically the binding site for such medications as diazepam as well as muscle relaxants.
These structural analyses combined with electrophysiological measurements provide mechanisms … of inhibitory neurotransmission by autoimmune antibodies and can explain the clinical symptoms of patients with GABA-A receptor encephalitis at the atomic level.
Visitor Suspensions Linked to Rise in Certain Prescriptions
Older adults hospitalized in the first months of the COVID-19 pandemic received more benzodiazepines on days when visitors were not allowed, according to a report in the Journal of the American Geriatrics Society.
Researchers at the University of Pennsylvania conducted a retrospective analysis of benzodiazepine and antipsychotic use among patients 65 and older who were hospitalized at one of four Mid-Atlantic hospitals between March 1 and May 31, 2020. After excluding seniors who were admitted to intensive care or died during this period, the sample included 2,931 patients who spent 14,497 days in acute care. This included 2,358 days when visitors were allowed and 12,139 when they were not.
Overall, 31.5% of patients received a benzodiazepine and 10.2% received an antipsychotic while hospitalized (4.0% received both). The researchers found that the odds of benzodiazepine use were lower on the days when visitors were allowed versus not allowed. Antipsychotic use, however, did not significantly differ depending on visitation policies.
The researchers noted the reason for the benzodiazepine difference during visitation restrictions was unclear: “A lack of caregiver support may lead to increased incidence of delirium, agitation, or anxiety, which in turn leads to increased benzodiazepine use,” they wrote.
“Our findings underscore the importance of caregivers for ensuring quality care for older adults and support efforts to better integrate caregivers into care teams,” the researchers concluded.
Aripiprazole May Help Reduce Hyperprolactinemia
Hyperprolactinemia, or increased production of the hormone prolactin, is a common side effect of several antipsychotics and can result in weight gain, insulin resistance, and sexual dysfunction. A meta-analysis published in Translational Psychiatry suggests that patients experiencing antipsychotic-induced hyperprolactinemia might benefit from taking aripiprazole or vitamin B6.
Researchers at Peking University in Beijing compiled data from 31 clinical studies that tested pharmacological strategies for hyperprolactinemia in 2,954 adults with schizophrenia. The studies in the meta-analysis included both placebo trials as well as head-to-head medication trials involving six strategies: switching antipsychotics (to aripiprazole, olanzapine, or quetiapine); adjunctive low-dose (5 mg) or high-dose (10 mg) aripiprazole; adjunctive metformin; adjunctive dopamine agonists; adjunctive vitamin B6; or adjunctive Peony-Glycyrrhiza decoction (PGD), a traditional herbal medicine.
Three of the six strategies were superior to placebo at reducing prolactin levels: adjunctive aripiprazole, switching to aripiprazole, or adjunctive vitamin B6. When the researchers compared patient outcomes according to their prolactin levels at baseline, they found that the interventions had no effect on patients whose prolactin levels were under 50 ng/ml.
The findings “indicated that the intervention for patients with [antipsychotic]-induced [hyperprolactinemia] less than 50 ng/ml might be not necessary,” the authors wrote.
Patients with prolactin levels between 50 ng/mL and 100 ng/mL experienced drops in prolactin levels when taking adjunctive aripiprazole and/or B6. Patients with prolactin levels above 100 ng/mL only showed a response to adjunctive low-dose aripiprazole, they noted.
The researchers also explored side-effect profiles and found that only adjunctive high-dose aripiprazole was associated with greater effects than placebo. Combined with the broader efficacy of 5 mg aripiprazole, the researchers suggested that aripiprazole augmentation is better at low doses.
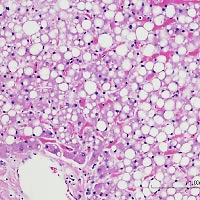
Nonalcoholic Fatty Liver Disease Associated With Elevated Risk of Dementia
Older adults with nonalcoholic fatty liver disease (NAFLD) may be at an elevated risk of dementia, a study in Neurology suggests.
Researchers from Sweden’s Karolinska Institutet used Swedish health registries to identify 2,898 adults aged 65 and older without dementia who received a diagnosis of NAFLD between 1987 and 2016; each of these adults was matched with 10 adults of similar demographics but without NAFLD.
By five years later, 3.6% of the adults with NAFLD and 2.0% of those without NAFLD had received a dementia diagnosis; by 10 years, the rates were 7.5% for adults with NAFLD and 5.5% for those without NAFLD. After adjusting to other risk factors, such as stroke, diabetes, or depression, the researchers calculated that NAFLD was associated with a 38% increased risk of any dementia, with a greater risk observed for vascular dementia compared with Alzheimer’s dementia. When breaking down the population by age groups, the researchers found that NAFLD only increased the risk of dementia if the diagnosis was made before 75 years of age.
Patients who had comorbid NAFLD and a vascular problem were at an even greater risk of dementia; for instance, adults with NAFLD and a history of stroke were three times as likely to develop dementia compared with those with neither condition.
“These results are in accordance with the major hypothesis that the association between NAFLD and dementia is mainly driven by vascular damage in the brain,” the researchers wrote.
Psychosis-Focused Outpatient Program Shows Promise
Patients with psychosis who participated in an intensive six-week outpatient program saw symptom improvements, a study in Psychiatric Research & Clinical Practice has found.
The program—called the UCLA Thought Disorders Intensive Outpatient Program (TD IOP)—combines both group-based and individual support focused on social and life skills training, improved self-care (like diet and sleep), medication management, and case management. Participants meet three times a week for at least six weeks.
For this study, the team assessed symptom changes and personal feedback from 92 people with psychosis who participated in the study between May 2018 and June 2020; 71 of these participants completed the full program.
Overall, participants showed clinically significant improvements in five of eight psychosis-related domains (listed in the Clinician-Rated Dimensions of Psychosis Symptom Severity scale): hallucinations, delusions, disorganized speech, depression, and mania. Abnormal movements, negative symptoms, and cognition did not significantly improve. Ninety-three percent of participants experienced improvement in at least one symptom domain.
“Additionally, most participants (73.2%) completed the program either with a reduction or no change in antipsychotic dose, indicating improvements cannot be attributed to medication alone,” the authors wrote.
Participant feedback on the program was also positive (scoring the program an 86.6 out of 100). Participants particularly valued the socialization offered by TD IOP along with the emphasis on skill building and ready access to providers, the authors wrote.
Brain Lesions Offer Clues On How to Treat Addiction
Studying the brains of people who quit smoking after experiencing brain damage has led researchers to a neural circuit that they believe may be a good therapeutic target for addiction. The findings were published in Nature Medicine.
“Neuromodulation trials have shown some promise in treating addiction but have been limited by the fact that the optimal therapeutic target was unknown,” the investigators wrote.
To identify potential targets for treating addiction, the investigators examined CT or MRI scans from 129 daily smokers who experienced localized and clearly identifiable brain lesions. This group included 34 patients who quit smoking without difficulty (no relapses or cravings) within one day of their lesion.
The lesions in the patients who quit were in many different brain regions, but they were all connected to a large brain circuit associated with addictive behaviors. In contrast, the lesions in the brains of the people who continued to smoke regularly did not map onto this circuit.
The investigators next examined a set of scans from 186 different individuals who completed an alcoholism risk assessment following a focal brain lesion. Lesions associated with lower alcoholism risk showed similar connectivity to lesions that disrupted addiction to smoking, the researchers wrote. Further, one of the nodes in this circuit is in a region targeted by transcranial magnetic stimulation therapy for smoking cessation (which was recently approved by the FDA).
“Now that our study has identified a target—a specific human brain circuit—we hope to test whether targeted neuromodulation to this brain circuit provides sustainable symptom relief to our patients,” senior author Michael D. Fox, M.D., Ph.D., of Brigham and Women’s said in a Harvard news release. ■