A recent imaging study that reconstructed a cubic millimeter of human cortical tissue at nanometer scale is providing new insight into the complexities of human neural circuits.
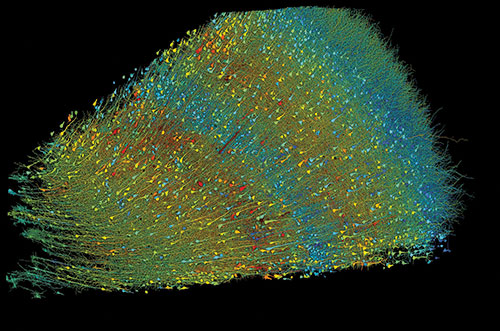
The study, by Alexander Shapson-Coe, M.D., Ph.D., et al, published in Science, was conducted at Harvard University in conjunction with Google Connectomics, and supported in part by the National Institutes of Health (NIH) BRAIN initiative. [BRAIN is an acronym for Brain Research Through Advancing Innovation Neurotechnologies®.] The one cubic millimeter sample—approximately the size of a single sesame seed—was extracted during a surgical procedure to treat refractory epilepsy.
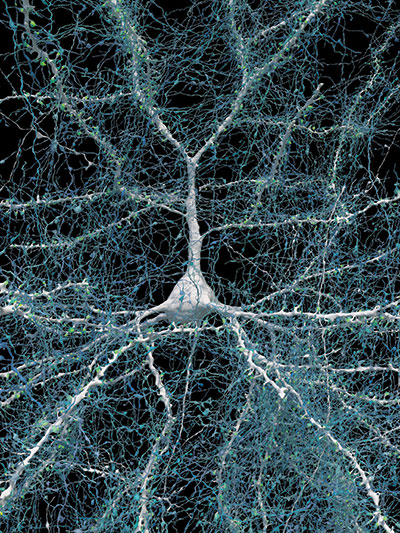
Whether or not this technology will ultimately translate from bench to bedside remains to be seen. It does, however, represent a significant step in development of connectomics—an evolving technology that is helping scientists look deep into the brains of animals and humans. Connectomics involves mapping how individual neurons are connected to one another to form functional networks, according to Harvard Medical School Associate Professor of Neurology Wei-Chung Allen Lee, Ph.D. In an article published in Harvard Medicine News in 2023, Lee commented that “the goal is to create connectomes—detailed structural maps of connectivity where we can see every neuron and every connection.” A perfect connectome would allow scientists to see how every neuron was connected to every other neuron, he noted.
The current effort mapped out more than one quadrillion voxels of cortical tissue. (A voxel is a three-dimensional cubic analog of a pixel).
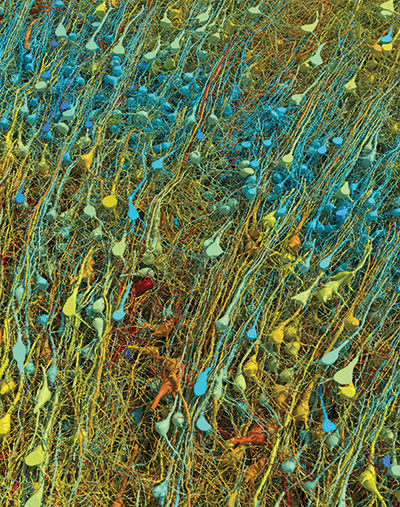
The sample extended through all layers of the cortex. The scientists were able to reconstruct images of thousands of neurons and more than 100 million synaptic connections. Among the novel findings were the discovery of a previously unrecognized class of directionally oriented neurons in deep layers, and what they described as “very powerful and rare multisynaptic connections between neurons throughout the sample.”
In their discussion, the authors acknowledged the challenges facing the use of such data to create connectomes that can be clearly correlated with human behavior. Some of the anomalies observed in this brain fragment—such as some neuronal fibers called axons curling into extensive spirals—may be unique to the individual or may be associated with the neuropathology or pharmacotherapy of epilepsy, the authors said. Further, human experience, as well as genetics, alter neural circuits, which presents the challenge of meaningfully comparing neural circuits between human brains that have been shaped by different experiences.
“What are the prospects for this study to have an impact on patients who have neuropsychiatric disorders?” wondered Douglas Kim, Ph.D., a program officer in the National Institute of Mental Health (NIMH) Division of Data Science and Technology and project director for the NIMH grant that helped support the Science study. “The research team had access to a very small sample of human brain tissue from this patient undergoing surgery for epilepsy.” At this point the study represents a technology development effort—not a clinical research project—but the detailed micrographic mapping of even this small sample is the end result of years of technology development, he noted.
The question, then, is how we eventually take the accumulated data from this study and future reconstructions of human or animal brain samples and “convert [them] into knowledge that may be helpful to human patients suffering from neuropsychiatric diseases,” Kim said. That is going to be “a long and important journey.”
There are many different avenues being pursued in neuroscience to try and address significant brain diseases, and this new study highlights another important step along the way, he noted.
There are certain limitations inherent in the reconstruction of living human brain tissue, Kim observed. Only a small subset of patients with neuropsychiatric disorders undergo neurosurgery, and only a fraction of those patients have brain tissue removed, he noted. This greatly limits both the number of potential samples available and their size.
If, however, further explorations of similar brain samples show similar aberrations such as axon whorls, then perhaps a brain-wide synaptic difference may be considered relevant to a specific neuropsychiatric disorder. “Perhaps one day this type of small sample study will help reveal markers of certain diseases, neuropsychiatric, or otherwise,” said Kim.
Employing connectomics may also be a meaningful way to examine human memory, said Sheena Josselyn, Ph.D., a senior scientist at The Hospital for Sick Children in Toronto and a Professor in the departments of psychology and physiology at the University of Toronto.
Advanced brain mapping research in rodents has made startling progress, Josselyn said. Scientists are now able to identify the neurons involved in a particular rodent memory, and—using invasive technologies—erase and reactivate that memory. “This is really the stuff of science fiction,” she said.
Despite the differences in complexity between human and rodent brains, the principles of memory formation are similar, Josselyn added. Although researchers cannot do highly invasive neuron manipulations in living humans, Josselyn is optimistic that these 3D reconstructions of living tissue might be useful proxies. Someday, connectomics could be applied to treat disorders of “too much” memory (as in PTSD) or “too little” memory (as in Alzheimer’s disease and other dementias).
In addition to funding from the BRAIN Initiative and NIMH, this study was supported by the National Science Foundation, Intelligence Advanced Research Projects Activity-Department of Interior, and the Stanley Center for Psychiatric Research at the Broad Institute. ■