Black box warnings and physician safety communications about the risk of valproic acid during pregnancy have failed to boost contraceptive use or reduce the number of pregnancies among women taking this medication, according to a recent
study in
JAMA Network Open.
“Exposure to valproic acid during pregnancy is a significant issue; it has a very potent teratogenic risk, causing very severe fetal malformations, including spina bifida, as well as neurocognitive defects and autism, which are lifelong,” senior study author Almut G. Winterstein, R.Ph., Ph.D., a distinguished professor in the Department of Pharmaceutical Outcomes and Policy and director of the Center for Drug Evaluation and Safety at the University of Florida, told Psychiatric News.
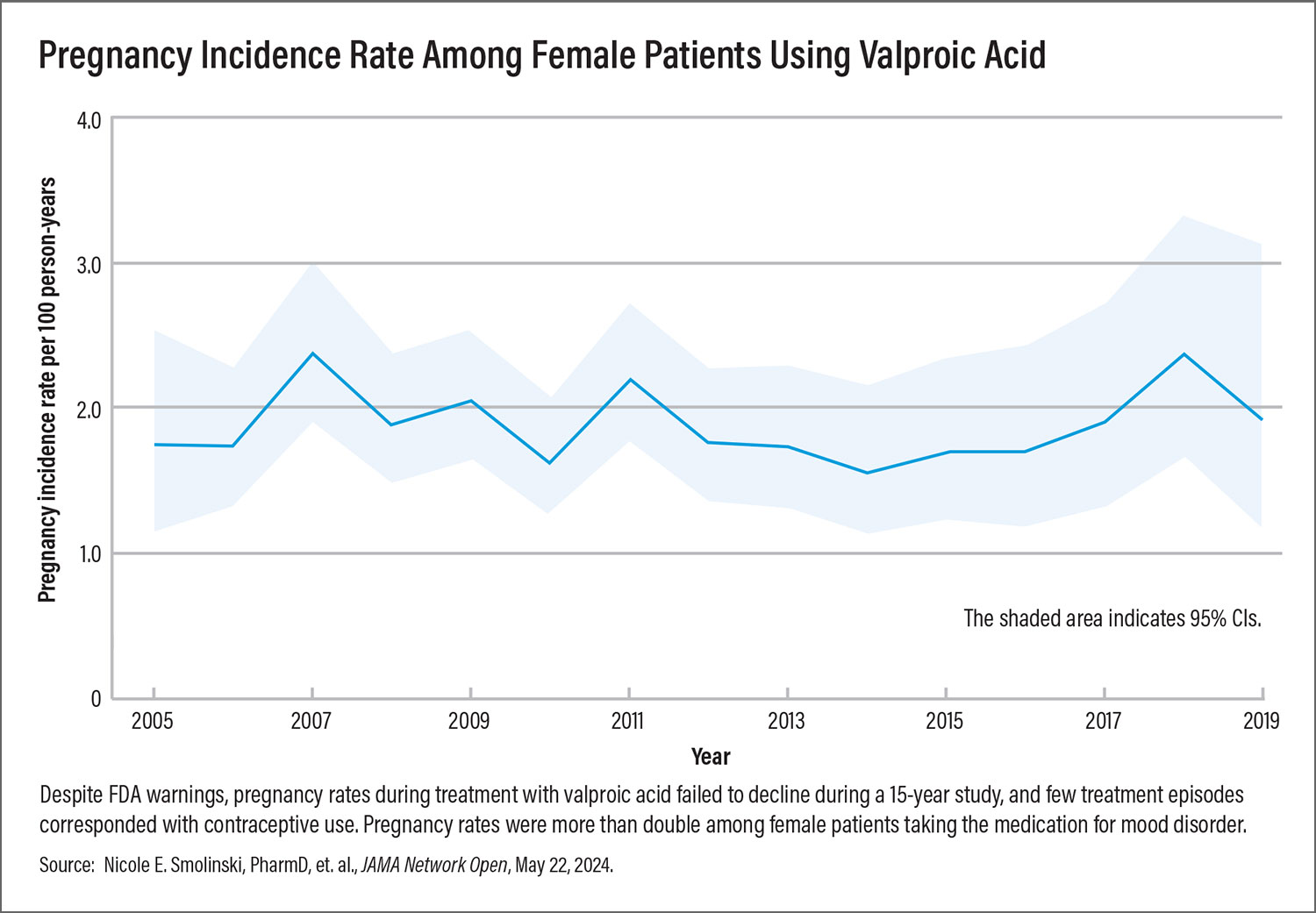
Yet Winterstein and colleagues found pregnancy rates among women taking valproic acid actually increased slightly over the 15 year-period they studied: from 1.7 per 100 person-years in 2005 to 1.9 per 100 person-years in 2019. More than one-quarter of women (28%) were still prescribed valproic acid at least one time after getting pregnant, while fewer than one-quarter of valproic acid treatment episodes (22%) overlapped with prescription contraceptive use of even one day.
Researchers looked at pharmacy and health claims data for 70,000 insured females of childbearing age (aged 12 to 44) treated with valproic acid at any point between 2005 and 2019. Mood disorders was the most common indication for which valproic acid was prescribed to these women (43% of treatment episodes), followed by migraines (20%), and epilepsy (15%).The researchers identified 723 pregnancies among the sample.
Women with mood disorders had the highest rate of pregnancy (2.32 per 100 person-years), while women with epilepsy had the lowest (1.22 per 100 person-years).
Winterstein said the results demonstrate the need for the Food and Drug Administration (FDA) to create a formal Risk Evaluation and Mitigation Strategy (REMS) program, as some other countries have done, to mitigate prenatal exposure to valproic acid. (Other forms of the drug are valproate or divalproex sodium.) She also worries that state restrictions or bans on abortion imposed in recent years may make it more difficult for women whose fetuses were exposed to obtain abortion care.
Gap in Preconception Care Training
“The findings are pretty shocking,” said Sarah Nagle-Yang, M.D., Deputy Executive Director of the Colorado Center for Women’s Behavioral Health and Wellness, and associate professor of psychiatry at the University of Colorado School of Medicine. There is a gap within psychiatric training on the importance of assessing patients’ reproductive potential, providing preconception care, and informing patients about the risks posed by a given treatment on potential pregnancies, she added.
Fully half of all pregnancies are unplanned, even among the general population, she said. People with bipolar disorder are at increased risk of unplanned pregnancies due to impulsivity or hypersexuality that may be associated with an illness episode. “With any woman of childbearing age, providing preconception counseling as a part of medication treatment should simply be a part of our everyday care.”
When prescribing valproic acid or working with patients who don’t want a future pregnancy, even more directive contraception counseling is needed, Nagle-Yang added. Research shows that over time long-acting reversible contraceptives (LARCs) such as intrauterine devices and implantable devices are 20 times more effective than other contraceptives because they are not user dependent.
“For patients without contraindications having difficulty accessing a specialist physician [to obtain LARCs], I think psychiatrists absolutely should prescribe oral contraceptives. … However, I would explain in my patient counseling that oral contraception is not as effective as LARCs,” she added.
Untreated or undertreated mood disorders also pose a risk in pregnancy, so preconception care must balance the risk of the underlying illness with the risks of medication exposure, Nagle-Yang said. “I also consider the patient’s unique disease course, previous treatment responses, personal strengths, and level of social support.”
Women with mood disorder have multiple treatment options, but Winterstein said that psychiatrists should keep in mind that other anticonvulsants used for mood disorders, such as carbamazepine and oxcarbazepine, also pose significant teratogenic risk. They can also reduce the effectiveness of hormonal contraceptives, including some implants.
Nagle said a better choice for women with childbearing potential is lithium, which is highly effective for all phases of bipolar disorder (valproic acid is only approved for acute mania and mixed episodes) and is demonstrated to have far lower risk during pregnancy than previously hypothesized. Lamotrigine is excellent for individuals experiencing a bipolar depressive episode or as a maintenance therapy.
Reconsider Off-Label Teratogens
“There are a number of other mental illnesses that may be less severe that are also being treated off-label with valproic acid,” said Winterstein, who for six years also served as chair of the Food and Drug Administration’s Safety and Risk Management Advisory Committee. “The question is, is that really the best approach for women of childbearing potential?”
The European Medicines Agency (EMA) did not think so, launching a mandatory
valproate pregnancy prevention program in 2018, after a provider educational program failed to reduce fetal exposures. Clinicians are required to assess each patients’ pregnancy potential, administer pregnancy tests before starting and during treatment, and provide contraceptive care. Specialists must also review the need for treatment annually.
Winterstein believes U.S. regulators should do more as well, even if not as stringent as the EMA. “Some effective REMS can be as simple as a virtual, one-hour prescriber training that walks physicians through the risks of the medication and advises them on proven means of ensuring safety for women with childbearing potential,” she noted.
One resource for psychiatrists who want to increase their skills in reproductive psychiatry is the
National Curriculum in Reproductive Psychiatry, of which Nagle-Yang is a coauthor. It provides comprehensive instruction about the diagnosis and treatment of psychiatric disorders throughout the reproductive life span, including preconception planning and the prenatal and postpartum period.
“I want to challenge my colleagues to expand their vision of their role, to embrace the provision of holistic patient care, which includes a patient’s reproductive care, especially when we’re providing medication treatment,” Nagle-Yang said. ■