The discovery of distinct subtypes of bipolar disorder that are based on an individual’s neurocognition rather than traditional symptom checklists holds the promise of optimizing care, according to a leading researcher who has dedicated more than two decades to the study of the disorder.
“Less than half of people with bipolar disorder describe themselves as having found effective treatments, meaning they’ve had a partial treatment response or intolerable side effects from medications,” said Katherine E. Burdick, Ph.D., the Borus Distinguished Chair in Psychiatry and director of the Mood and Psychosis Research Program at Brigham and Women’s Hospital. She discussed some of her research during a recent webinar for the Brain and Behavior Research Foundation.
“Although bipolar disorder involves substantial disability and substantial societal cost, we are still in a position where we know very little about this disease and new treatments are few and far between,” Burdick said.
She noted that it takes about seven years for someone with bipolar disorder to receive a correct diagnosis after the onset of symptoms—a gap that puts people at risk for inappropriate medications and poor health outcomes.
Bipolar disorder is listed by the World Health Organization as one of the leading causes of disability worldwide, amounting to a $200 billion annual health and economic burden in the United States alone, Burdick said. However, what drives this disability isn’t its acute mania or psychosis, which tend to be relatively short-lived symptoms.
Rather, Burdick and her team have zeroed in on what they believe is the true culprit: significant cognitive impairment that persists in many individuals with bipolar disorder even after affective symptoms are in remission. That’s because intact cognition in areas of the prefrontal cortex related to emotion regulation is necessary for a person to function well in the community, she said. Impaired cognitive control in these regions of the brain puts a person at risk for emotional dysregulation, a core feature of bipolar disorder.
“If we’d like to reach beyond affective remission and really push for full recovery and thriving in people with bipolar illness,” Burdick said, “we need to address cognition directly.”
New Subtypes Based on Cognition
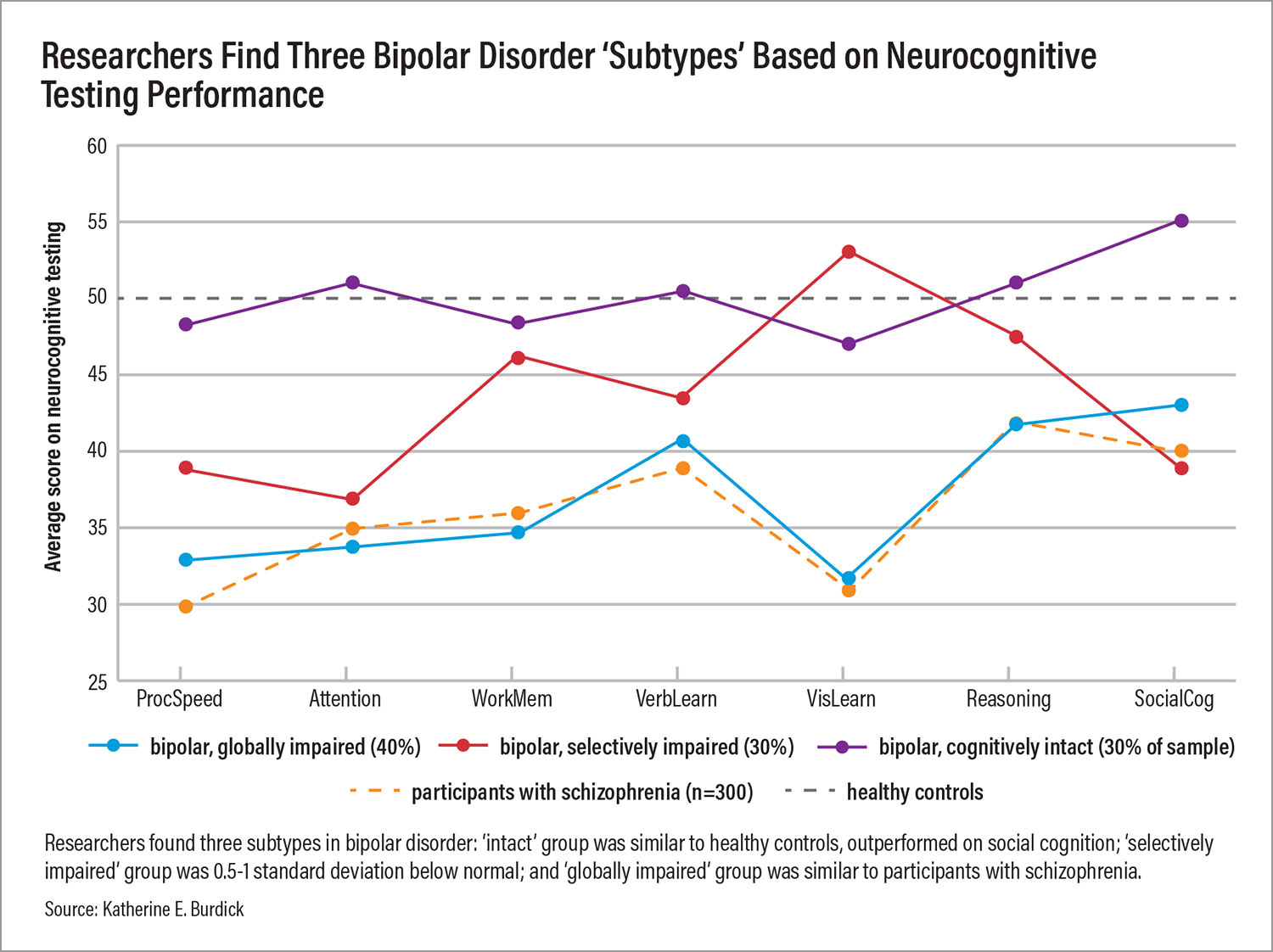
To assess cognition, Burdick and her colleagues have conducted several studies over the past decade for which they gave individuals with bipolar disorder a battery of paper and pencil or computerized tests involving processing speed, attention, working memory, verbal learning, visual learning, reasoning, and social cognition. They compared their results with those of healthy individuals as well as people with schizophrenia.
Using statistical techniques, researchers identified three subtypes of bipolar disorder:
•
“Cognitively intact” (about 30% of people with bipolar disorder): Performed similarly to healthy controls and even outperformed them on at least one measure of social cognition.
•
“Selectively impaired/suboptimal” (about 30%): Showed mild to moderate impairment on processing speed, attention, and social cognition, but performed average or above average on other measures.
•
“Globally impaired” (about 40%): Showed deficits across all cognitive domains at a relatively severe degree and performed similarly to people with schizophrenia.
Did any other symptoms or risk factors set these groups apart from one another? Chiefly, Burdick noted, individuals with suboptimal or impaired cognition were more likely to experience a recurrence of manic episodes, have a substance use disorder, and have more sleep disturbances.
“When we think about the recurrence of mania, substance use disorders, and sleep disturbances,” she said, “all of these are behavioral factors that are modifiable, things that we should be directly targeting for treatment in order to optimize outcomes for individuals with bipolar disorder.”
Targeting Inflammation
Burdick and colleagues are also targeting another modifiable factor that differed among the cognitive subtypes: inflammation. Early in the disease course, pro-inflammatory molecules called cytokines spike during acute mania or severe depression due to the extreme stress of these states, Burdick said. These markers return to normal when affective stability or euthymia is achieved.
“Later in the illness, after about four to five episodes of mania, we see an incomplete recovery of molecular markers in the blood in some people. They indicate chronic but low-grade inflammation.”
Burdick and colleagues have shown that elevated blood levels of one key component of the immune system, tumor necrosis factor alpha (TNF-a), are present in individuals in the cognitively “suboptimal” and “impaired” groups, but not among individuals in the cognitively “intact” group. Additional research by Burdick has shown that TNF-a may contribute to executive function problems. “Targeting this inflammation when present might serve to halt the decline that is associated with the cumulative burden of this disease,” she said.
Burdick and her colleagues’ research into the origins, sequelae, and treatment of bipolar disorder is ongoing. In addition, Burdick serves as one of the scientific directors for the Integrated Network of Breakthrough Discoveries for Thriving with Bipolar Disorder, an initiative that involves more than 100 scientists and clinicians collaborating on a long-term study of 4,000 participants with lived experience of bipolar disorder.
Burdick thinks that this type of longitudinal research, at scale, is especially critical for bipolar disorder because of its complex, dynamic nature. “This is a game changer for the field,” she told Psychiatric News. “Much of the work we have done will finally be scaled up in a way that will reveal novel insights into the disease and improve care for those living with it.” ■