There is growing recognition of the role of nutrition in mental health. Poor dietary habits are now understood as modifiable risk factors for mental health. Further, research suggests that individuals with psychiatric illness are more likely to have poor dietary patterns, disordered eating behaviors, and nutritional deficiency, contributing to both physical and mental health comorbidities. Therefore, there is an urgent need to integrate lifestyle interventions such as nutrition management in treating psychiatric illness (Morkl, et al., 2021).
The World Health Organization highlights nutrition as a key component in reducing the life-expectancy gap between people with psychiatric disorders and the general population (Teasdale, et al., 2020). Similarly, the International Society for Nutritional Psychiatry Research, founded in 2013, has worked to establish a cohesive framework for integrating nutrition into psychiatric care (Jacka, 2017).
However, despite growing evidence, nutrition is rarely integrated into psychiatric practice. Most mental health providers, including psychiatrists, psychologists, and psychotherapists, are unfamiliar with evidence for the benefits of nutrition on mental health. For psychiatrists, sparse nutrition education in medical school curricula may be to blame. Current nutrition training in general medical curricula is limited—only 40% of U.S. medical schools reach established goals of teaching 25 hours of nutrition in preclinical years. It is unsurprising that most psychiatrists report having no specific training in nutrition and are therefore unprepared to incorporate dietary strategies in patient care (Morkl, et al., 2021; Mudd & Angelotta, 2024).
Statistics aside, psychiatrists can and should integrate nutrition management into clinical practice. Although many clinicians may feel underprepared, existing tools and research can support them in delivering dietary advice.
Diet Quality and Mental Health
Research increasingly demonstrates that whole foods and nutrient-dense diets are likely to provide better mental health outcomes than supplementation of isolated nutrients. The historical focus on individual nutrients, such as omega-3 polyunsaturated fatty acids or vitamin D, is shifting because we know that individuals consume whole foods, not isolated nutrients (Jacka, 2017). Traditional diets that are rich in vegetables, fruits, lean proteins, and whole grains and limited in highly processed foods provide nutrients that promote resilience against psychiatric disorders. However, individuals with severe mental illness often have excessive caloric intake, low diet quality, and poor nutritional status compared with the general population (Sarris, et al., 2015).
Therefore, diet quality is important to consider when managing psychiatric illness. High-quality diets, characterized by higher intake of fruits, vegetables, fish, and whole grains, have been linked to improved well-being and reduced likelihood of depression (Collins, et al., 2021; Jacka, 2017). On the other hand, low-quality diets, characterized by high overall fat intake, high sugar intake, and low fruit and vegetable consumption, are associated with greater odds of psychological distress, increased anxiety-like behavior, and increased odds of self-reported depression. Importantly, these relationships are stable across cultures, sociodemographic factors, and education level (Collins, et al., 2021).
Assessing diet quality in clinical practice: Although there are not yet practice guidelines around assessing diet quality in a psychiatric clinical setting, psychiatrists can implement existing tools, such as MyPlate, an evidence-based tool from the U.S. Department of Agriculture that translates dietary guidelines into practical advice for patients. Through the MyPlate app, patients can take a dietary quiz to assess their intake against USDA recommendations. Key MyPlate recommendations include:
•
Half of the plate should consist of fruits and vegetables.
•
Emphasize whole grains and minimize refined grains.
•
Vary protein sources and limit red meat.
•
Reduce intake of added sugars and saturated fats.
Clinicians can encourage patients to use this app to track progress and set personalized dietary goals. For more motivated patients, MyFitnessPal offers detailed dietary tracking tools. However, interdisciplinary collaboration with dietitians often yields the best outcomes. Studies show that integrating nutritional assessments within an interdisciplinary team significantly improves patient adherence and outcomes (Kolasa & Deen, 2005).
Evidence-Based Dietary Patterns
While diet quality is important, research highlights specific dietary patterns with therapeutic value for mental health.
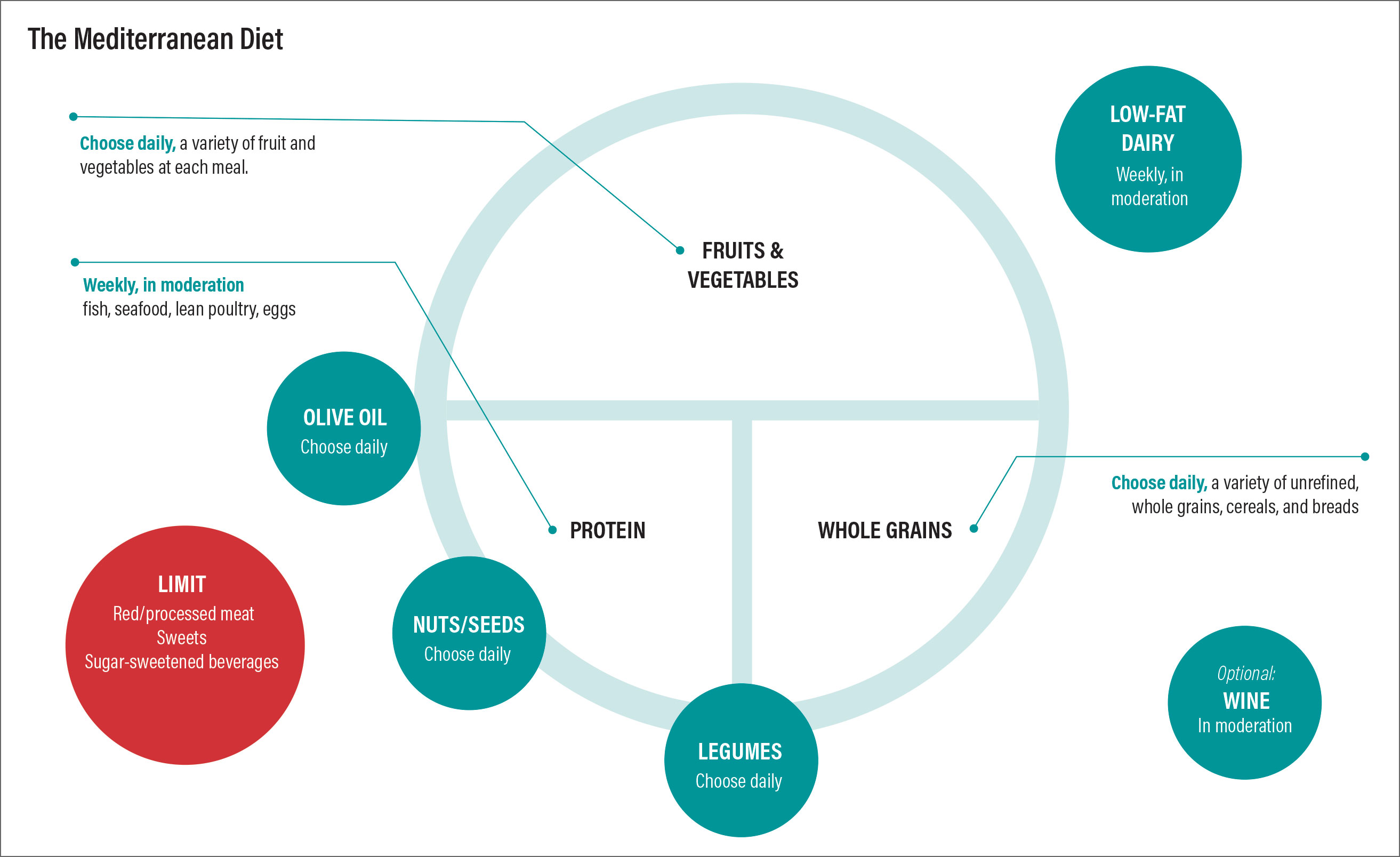
Mediterranean-style diet: A Mediterranean-style diet, rich in fruits, vegetables, olive oil, fish, and legumes, has shown the most robust evidence for mental health benefits. Studies indicate that this dietary pattern reduces the risk of depression and anxiety in multiple randomized controlled trials. Its neuroprotective effects may be attributed to anti-inflammatory, antioxidant, and vascular benefits (Jacka, 2017). Key components include:
•
Emphasis on plant-based foods (e.g., vegetables, fruits, legumes)
•
Intake of healthy fats from olive oil and fish
•
Limited consumption of sweets and protein from animal sources (especially red meat)
•
Optional moderate consumption of wine
Other dietary patterns: While a Mediterranean-style diet has established benefits for mental health, emerging evidence suggests that other dietary patterns could offer similar support for mental health:
•
The DASH diet (Dietary Approaches to Stop Hypertension) was developed to prevent and control hypertension. This dietary pattern has been linked to improvement in obesity, metabolic syndrome, gestational diabetes, type 2 diabetes, stroke, and coronary heart disease (Shabbir, et al., 2022).
•
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) is a hybrid of the Mediterranean-style and DASH diets and was designed to promote brain health in aging (Morris, et al., 2015).
•
The ketogenic diet, a high-fat, low-carbohydrate regimen, has been used successfully to manage epilepsy. Emerging research suggests that it may also reduce depressive symptoms and improve outcomes in schizophrenia, though more studies are needed (Bostock, et al., 2017).
While a Mediterranean-style diet has well-documented benefits for mental health, other dietary patterns—such as the DASH, MIND, and ketogenic diets—show promise but require further research. Existing patient-facing resources on these dietary patterns, such as the American Heart Association’s resources on a Mediterranean-style diet, can be utilized in nutrition counseling within clinical practice.
Supplements in Psychiatric Care
While whole foods are preferable, supplements can serve as adjuncts when dietary changes are challenging. In fact, a growing number of randomized controlled trials and meta-analyses demonstrate mental health benefits of nutraceuticals (nutrient-based natural products) and phytoceuticals (plant-based natural products). This growing evidence base was recently summarized in clinical guidelines from the World Federation of Societies of Biological Psychiatry and the Canadian Network for Mood and Anxiety Treatments; see Table 1 (Sarris, et al., 2022).
However, supplements have limitations. The use of dietary supplements without coordination with a patient’s primary care provider increases risk of adverse events or drug interactions. Variability in product quality must also be considered. Supplements verified by the United States Pharmacopeia (USP) represent the highest-quality standard, ensuring that products contain the labeled ingredients at the declared potency and amounts, are free of harmful contaminants, release into the body within a specified time, and are manufactured under FDA Good Manufacturing Practices. Additionally, navigating pharmacodynamic and pharmacokinetic interactions between psychotropic medications and supplements is complex, often theoretical, and requires familiarity with reliable resources, such as the National Institutes of Health Nutrient Recommendations and Databases.
Special considerations are also necessary for certain populations. In the perinatal period, there is limited safety and efficacy data on supplements for mental health. Similarly, using single nutrients to treat psychiatric disorders in children has shown limited success. Factors such as microbiome variability, fixed incomes, and difficulties meeting recommended daily allowances for macronutrients and micronutrients further complicate supplement use for many patients, but particularly in older adults. Finally, the use of supplements as monotherapy for severe psychiatric conditions—such as major depressive disorder, bipolar disorder, or schizophrenia—raises concerns regarding their appropriateness and efficacy (Sarris, et al., 2022).
Although certain supplements have shown benefits in managing psychiatric conditions, their use comes with important caveats. Dietary supplements should be considered only as adjuncts to conventional care and used cautiously, ensuring no contraindications with prescribed psychotropic medications.
Barriers to Implementing Dietary Interventions
Patients with psychiatric illness encounter unique challenges in maintaining a healthy diet. The relationship between mental illness and nutritional status is bidirectional, shaped by both structural and illness-related barriers. Structural barriers—such as limited access to healthy foods, insufficient social support, low socioeconomic status, taste preferences, and daily habits—affect individuals with psychiatric illness and the general population alike. However, individuals with severe mental illness are at greater risk for food insecurity due to financial instability or tenuous housing. In addition to these structural barriers, patients with psychiatric illness often experience illness-related obstacles. Certain psychotropic medications can increase appetite, while cognitive impairment or reduced motivation can hinder ability to shop for and prepare healthy meals (Teasdale, et al., 2017).
Ongoing research aims to better understand the barriers faced by individuals with psychiatric conditions; however, providers can implement practical strategies in the meantime, including:
•
Familiarize patients with local food banks and nutrition programs to address food insecurity.
•
Collaborate with social worker and dietitian colleagues to provide comprehensive support.
•
Use motivational interviewing techniques to address cognitive and motivational barriers.
Growing evidence indicates that nutritional interventions should play a central role in psychiatric care. This emerging body of research highlights the importance of improving diet quality, adopting specific dietary patterns, and incorporating supplements when appropriate to support mental health outcomes. By incorporating nutrition management into routine care using existing resources, psychiatrists can empower patients to take charge of both their mental and physical health. Looking into the future, ongoing research efforts aim to further validate and standardize these interventions in psychiatric practice.
Author acknowledgement: I would like to thank Cara Angelotta, M.D., my program director, for her guidance on various iterations of this work. ■