The Use of Holographic Memory Resolution® to Improve the Physical and Biopsychosocial Symptoms of Chronic Pain: A Feasibility, Mixed Methods Study
Abstract
Objective
Methods
Results
Conclusions
Trial registration
HIGHLIGHTS
METHODS
Design and Setting
Sample
Procedures
Participant recruitment
Intervention
| Session | Description of session |
|---|---|
| 1 | Relaxation techniques are introduced, and each participant is invited to close his/her eyes which places the individual in alpha/theta EEG state. They are then asked to identify and describe a safe place or create an imaginary safe scene. The participant is then invited to identify any associated sensory features (ASF) (i.e., olfactory, tactile, gustatory, auditory, visual) or color(s) associated with their emotion(s) experienced in the safe place. Breathwork and the use of ASF are incorporated to diminish distraction, negative intrusion, negative self‐talk, and disruptive thoughts, which could potentially invade their safe place. HMR® processing of memories continues if time allows (see Session 2 as below). Participants are then invited to practice accessing their safe scene several times a day but not while driving or operating equipment. Permission was obtained from each participant at the end of each session to continue with the next session |
| 2 | The practitioner asks the participant what life events occurred since last session and when ready to proceed, are invited to re‐engage in relaxation and safe scene techniques. If the participant has difficulty with accessing their safe scene using color or ASF, these techniques are revisited. The practitioner then asks if the participant is ready to continue. The participant is next asked to metaphorically identify the presence of any pain, pressure, tightness, or tension and locate this tension in the body. This is achieved by guiding the participant through a series of nine questions describing the metaphor |
| 1. When you feel this pain/issue, where do you feel this in your physical body? | |
| 2. Is it on the inside, outside, or both? | |
| 3. Size? | |
| 4. Shape? | |
| 5. Color? | |
| 6. Temperature? | |
| 7. Texture? | |
| 8. Weight? | |
| 9. Anything else? | |
| Each metaphor is individualized according to the participant's responses and often tied to a traumatic experience. The participant is encouraged to describe what occurred during the event. Once the participant identifies the historical moment of traumatic encoding and dysphoric feelings generated at the time of the event, they are given the option to continue or stop review of the memory. The participant then identifies the experience that caused the pain or dysphoric memory or issue and is asked to image or integrate a creative solution to help diminish the dysphoric pain/emotions. The participant is encouraged to utilize a color or other ASF from the resolved image and to breathe or transmit this solution to the body‐mind to help diminish the dysphoric symptoms. Utilization of these ASFs fosters comfort and safety while dysphoric symptoms continue to be identified and released, keeping in mind, historical data is not changed but rather the goal is to ameliorate the dysphoric pain/emotions. Once the participant identifies the creative solution and integrates it internally, the practitioner inquires whether the relevant memory‐based pain is diminished or discharged. Next, the practitioner offers various options for mindfully disposing of the dysphoric memories (e.g., blowing them up, vaporizing them) and continues this emotional reframing with the same or additional memories or to move towards closure, grounding, and anchoring to re‐enter them back into the world. To do so, participants are asked to open their eyes, state where they are, describe their surroundings, and acknowledge the work accomplished during the session. The participant is encouraged to continue utilizing their personal colors or other ASFs to maintain safety and fully anchor the integrated solutions at the close of the session | |
| 3 | This session is conducted similarly to Session 2, using the colors, pain, and safe scene. As the participant recognizes they are safe and better understands the use of HMR with consecutive sessions, they are then enabled to explore deeper levels as they personally choose |
| 4 | Conducted similarly using the colors, pain, and safe scene as described in Session 3 |
Instruments
Adverse Childhood Experiences Questionnaire (ACE)
Patient Health Questionnaire (PHQ‐9)
Generalized Anxiety Disorder‐7 (GAD‐7)
Somatic Symptom Scale (SSS‐8)
PTSD Checklist for DSM‐5 (PCL‐5)
Subjective Vitality Scale—State Level Version (SVS)
Statistical Analysis
RESULTS
Sample
| Demographic characteristics | |
|---|---|
| Mean ± S.E. age, years | 49.9 ± 1.94 |
| Female, no. (%) | 51 (85) |
| Race, no. (%) | |
| Caucasian | 52 (87) |
| Black | 1 (2) |
| Asian | 1 (2) |
| Native American | 3 (5) |
| Other | 2 (3) |
| Hispanic or Latino, no. (%) | 4 (7) |
| Marital status, no. (%) | |
| Married or partnered | 33 (55) |
| Single | 14 (23) |
| Divorced | 10 (17) |
| Widowed | 3 (5) |
| Health characteristics | |
| Mean ± S.E. ACEs, score | 4.0 ± 0.30 |
| Symptoms began during COVID‐19 pandemic no. (%) | 5 (8) |
| Symptoms worsened during COVID‐19 pandemic, no. (%) | 24 (40) |
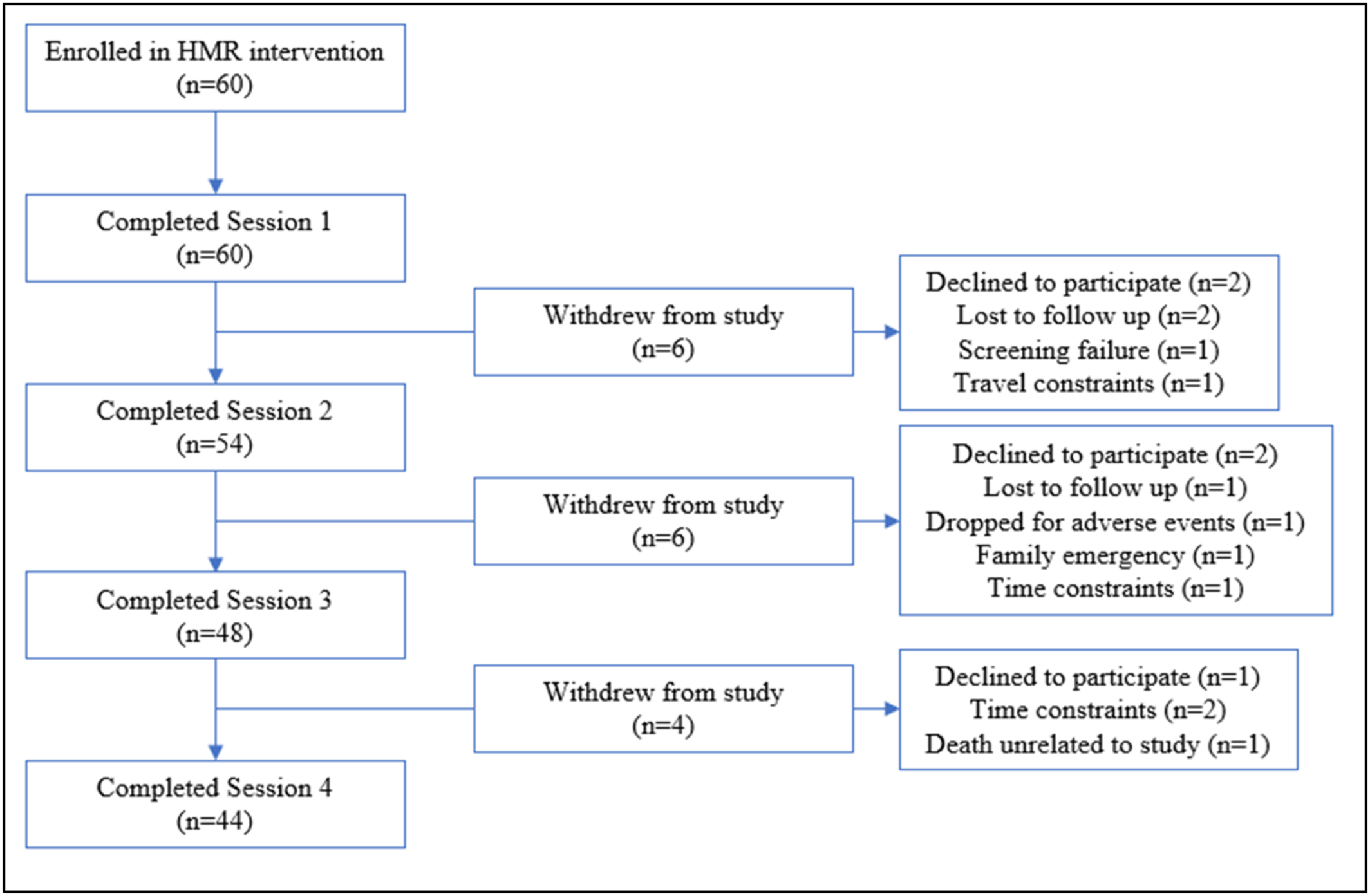
Feasibility
Symptom Outcomes
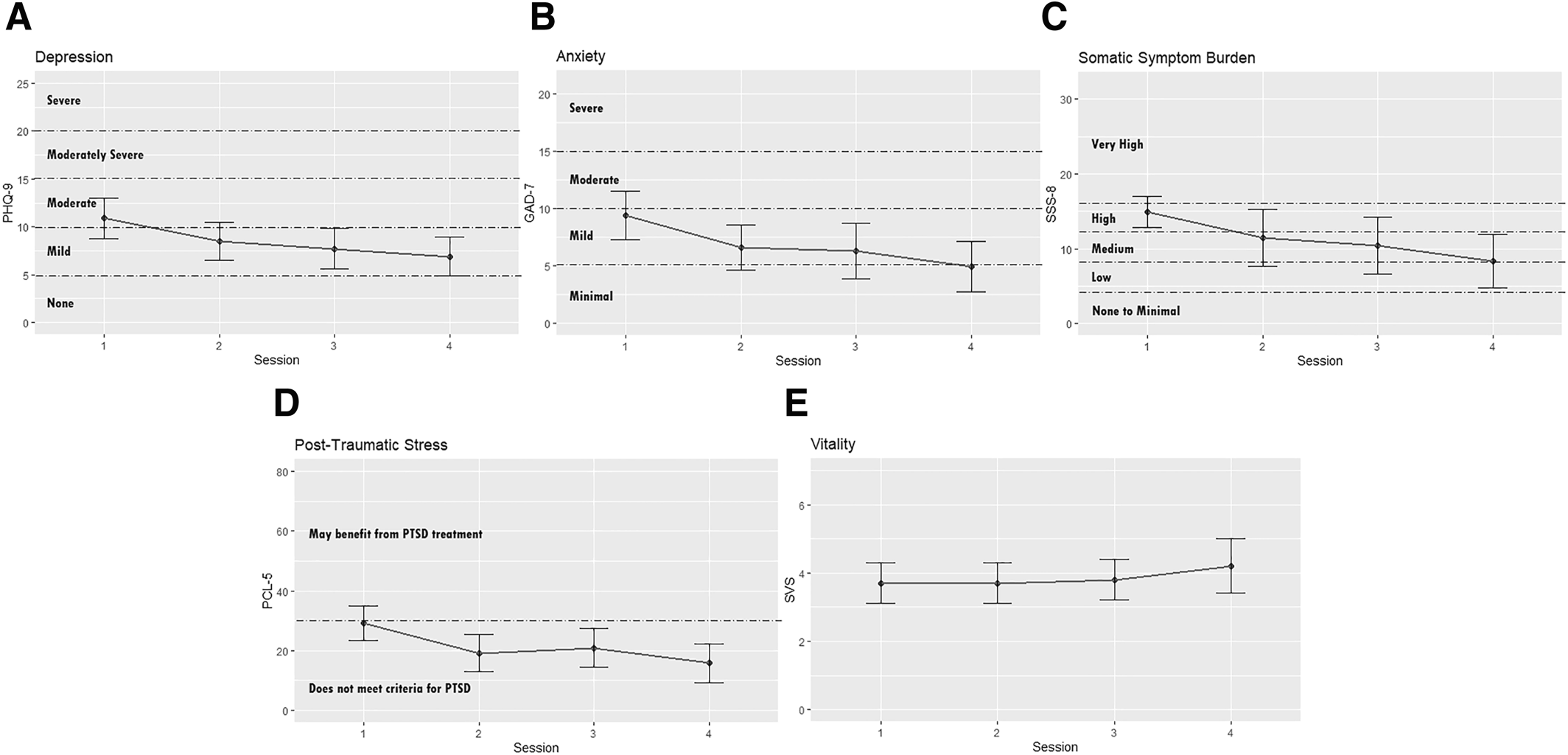
| Variable | Mean (95% CIa) | p‐value | |||
|---|---|---|---|---|---|
| Session 1 | Session 2 | Session 3 | Session 4 | ||
| Depression | 10.9 (8.7, 13.0) | 8.5 (6.5, 10.5) | 7.7 (5.6, 9.7) | 6.9 (4.9, 8.8) | 0.05* |
| Anxiety | 9.4 (7.3, 11.5) | 6.6 (4.6, 8.6) | 6.3 (3.9, 8.8) | 4.9 (2.7, 7.1) | 0.03** |
| Symptom burden | 14.9 (12.7, 17.2) | 11.4 (8.6, 14.2) | 10.4 (7.6, 13.1) | 8.3 (5.7, 11.0) | <0.01** |
| Post‐traumatic stress | 29.2 (23.5, 34.8) | 19.2 (13.0, 25.3) | 20.9 (14.4, 27.4) | 15.8 (9.4, 22.3) | 0.01** |
| Vitality | 3.7 (3.1, 4.3) | 3.7 (3.1, 4.3) | 3.8 (3.2, 4.5) | 4.2 (3.4, 4.9) | 0.72 |
DISCUSSION
Limitations
CONCLUSION
Footnote
REFERENCES
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).