Many youths detained by the juvenile justice system have been victims of childhood maltreatment and have psychiatric disorders. Depending on the sample and measure, 3% to 53% of detained youths have a history of sexual abuse (
1–
6) and 27% to 75% have a history of physical abuse (
1,
3,
7,
8). Recent studies have also found that over two-thirds of detained youths have a psychiatric disorder (
9,
10).
Studies of community, homeless, and clinical samples have documented an association between maltreatment and psychiatric disorders (
11–
18). Despite the high prevalence of maltreatment and psychiatric disorders among detained youths, few studies have examined the association between them in this population. Instead, most studies have focused on childhood maltreatment and its association with drug use (
5,
19–
22). We found only three studies of childhood maltreatment and psychiatric disorders among detained youths (
4,
7,
23). All three reported an association between maltreatment and disorders. Yet, these studies focused on only one or two disorders and had methodological limitations.
Dixon and colleagues (
23) examined posttraumatic stress disorder (PTSD) and childhood sexual abuse among female juvenile detainees in Australia. However, their sample was small (N=100), and the results are of limited generalizability to youths detained in the United States. They also relied on only one screening question to assess sexual abuse. Using one question may result in underreporting; a more reliable and robust approach is to ask a series of specific questions about types of sexual abuse (
24). Two studies of detainees conducted in the United States (
4,
7) had large samples (N>500) but also used only one screening question to assess maltreatment. Gover and MacKenzie (
7) examined the association between childhood maltreatment and depression and anxiety; however, they combined all types of maltreatment for analyses (
7). Gover (
4) focused only on the relationship between childhood sexual abuse and depression (
4).
To our knowledge, no large-scale study of detained youths has examined the relationship between childhood maltreatment and a range of psychiatric disorders. This omission is critical because findings from studies of community, homeless, and clinical samples (
11–
18) may not generalize to detained youths, who are disproportionately poor and male and from racial-ethnic minority groups. Furthermore, the detention center is a potential point of triage for child protection services and psychiatric treatment. Data on the association between child maltreatment and psychiatric disorders will help guide effective protective and therapeutic interventions.
This is the third article to report data on childhood maltreatment among participants in the Northwestern Juvenile Project, a longitudinal study of health needs and outcomes of detained youths. The first report documented the low concordance rates between self-reports and official records of physical abuse; only 17% of those who reported physical abuse had a court record of maltreatment (
25). The second study examined forced sexual victimization as part of a larger study of PTSD and trauma; however, it did not examine physical abuse (
26).
In this article, we present prevalence data on physical and sexual abuse, assessed by self-report and official records. We then present findings on the relationship between types of maltreatment and four types of psychiatric disorders: anxiety, affective, disruptive behavior, and substance use. We hypothesized that all types of maltreatment would be associated with psychiatric disorders, that youths with a history of severe maltreatment would have the highest prevalence rates of disorders, and that patterns of associations between maltreatment and psychiatric disorders would differ for males and females.
Methods
Sampling procedures
Participants were 1,829 male and female youths, randomly sampled at intake into the Cook County Juvenile Temporary Detention Center (CCJTDC) from November 1995 through June 1998 (
27). The sample was stratified by gender, race-ethnicity (African American, non-Hispanic white, and Hispanic), age (ten to 13 years or 14 years and older), and legal status (processed in juvenile or adult criminal court). Within each stratum, we used a random-numbers table to select names from the CCJTDC intake log. Selected demographic strata (for example, females, non-Hispanic whites, and ten- to 13-year-olds) were oversampled to obtain adequate numbers of participants in key subgroups. The final sampling fractions ranged from .018 to .689. Additional information on the sample is available from the authors.
Interviewers described the study to participants and obtained written informed assent (if participants were less than 18 years old) or consent (if they were age 18 or older). The Northwestern University Institutional Review Board, the Centers for Disease Control and Prevention Institutional Review Board, and the U.S. Office of Protection from Research Risks all approved the study and waived parental consent, consistent with federal regulations regarding research with minimal risk. We nevertheless tried to contact parents or guardians to inform them and offer them an opportunity to decline participation. Despite repeated attempts to contact a parent or guardian, none could be found for 44% of the participants. In lieu of parental consent, an independent participant advocate representing the interests of the participants oversaw youths' assent. Federal regulations allow for a participant advocate if parental consent is not feasible.
Participants were interviewed in a private area, almost always within two days of intake; most interviews lasted between two and three hours. Interviewers were trained for a month. Most had a master's degree in the social sciences and experience interviewing high-risk youths; one-third were fluent in Spanish. Female interviewers always interviewed females. Additional information on the study's methods has been reported elsewhere (
27).
The rigors of the detention center's schedule required approximately 5% of the interviews to end prematurely. Because childhood maltreatment was assessed at the end of the interview, these data were missing for 94 participants. The final sample for this analysis (N=1,735) consisted of 1,095 males and 640 females. The sample included 957 African Americans, 287 non-Hispanic whites, 488 Hispanics, and three youths who identified as “other” race-ethnicity. The childhood maltreatment module was more likely to be received by females than by males (N=640, 97%, versus N=1,095, 93%, p<.05) and by non-Hispanic whites than by Hispanics (N=287, 97%, versus N=488, 93%, p<.05). We accounted for potential bias from demographic differences in missing data by weighting the data. The mean age of the 1,735 participants was 14.8±1.4 years (range of ten to 18 years), and the median age was 15 years.
Measures
Self-report of childhood maltreatment.
Interviewers administered the Child Maltreatment Assessment Profile (CMAP), a structured interview based on the Child Maltreatment Interview (
24) and the Child Abuse Module for the National Institute of Mental Health's Methods for the Epidemiology of Child and Adolescent Mental Disorders Study (
28). The CMAP assesses six types of sexual victimization, use of force, and relationship to the perpetrator. There is no screening question. Instead, participants are asked about each type of abuse by each type of perpetrator.
To assess physical abuse, participants were asked how many times they had ever experienced each of five types of corporal punishment by “an adult or person who was in charge” of them. We classified experiences of being “hurt by an adult that resulted in bruises, broken bones, or severe injury” as severe physical abuse. We classified being “hit very hard,” “hit with an object,” or “beaten or kicked” as moderate physical abuse.
Official records of childhood maltreatment.
Project staff searched current and past records from the Cook County Court Child Protection Division for participants' names. These records consist of abuse and neglect petitions that were filed with the court after investigation by the Illinois Department of Children and Family Services (DCFS). Participants who were found by DCFS to have “credible evidence” of physical or sexual maltreatment were considered to have been abused. Petitions for “Excessive Corporal Punishment” and for “Substantial Risk of Physical Injury” were classified as severe physical abuse.
Rates of severe physical abuse and any sexual abuse are based on self-reported data or data from the court records; moderate physical abuse and specific types of sexual abuse are based on self-reported data only.
To analyze the relationship between a history of maltreatment and having a psychiatric disorder, we created an independent variable with five mutually exclusive categories of maltreatment: none, moderate physical abuse only, severe physical abuse, sexual abuse, and sexual and severe physical abuse. Participants classified in one of the latter three categories may have also experienced moderate physical abuse.
Psychiatric disorders.
We used the Diagnostic Interview Schedule for Children (DISC), version 2.3 (
29), the most recent version available at the time of data collection. The DISC 2.3, which is based on the
DSM-III-R, assesses the presence of psychiatric disorders in the past six months. It is highly structured, contains detailed symptom probes, has acceptable reliability and validity, and requires relatively brief training. Data are based on youths' self-report because it was not feasible to interview caretakers.
We began collecting data on PTSD 13 months after the larger study began, when the DISC version IV (DISC-IV) module became available for use; data on PTSD were collected for 898 participants. Of these, three did not receive the CMAP; therefore, PTSD was measured for 895 participants in the sample of 1,735 participants (531 males and 364 females).
For our analyses, we examined four types of disorder: any anxiety disorder (generalized anxiety disorder, overanxious disorder, panic disorder, obsessive-compulsive disorder, separation anxiety disorder, or PTSD), any affective disorder (major depressive episode, manic episode, hypomania, or dysthymic disorder), any attention-deficit hyperactivity disorder (ADHD) or disruptive behavior disorder (conduct disorder or oppositional defiant disorder), and any substance use disorder (abuse of or dependence on alcohol, marijuana, or other substances).
Statistical analysis
All analyses were conducted by using the survey routines in Stata SE, version 11.0 (
30,
31). To generate descriptive statistics and model parameters that reflect CCJTDC's population, each participant was assigned a sampling weight augmented with a nonresponse adjustment to account for demographic differences in missing data (
32). We used logistic regression to compare rates of abuse by demographic characteristics and to compare rates of psychiatric disorders by history of maltreatment. Taylor series linearization was used to estimate model variances. We tested for differences between specific groups (for example, African American youths compared with Hispanic youths) when the overall categorical predictor (in this example, race-ethnicity) was significant at the p<.05 level. Only statistically significant findings (p<.05) are noted in the text and tables.
Results
Prevalence rates of maltreatment
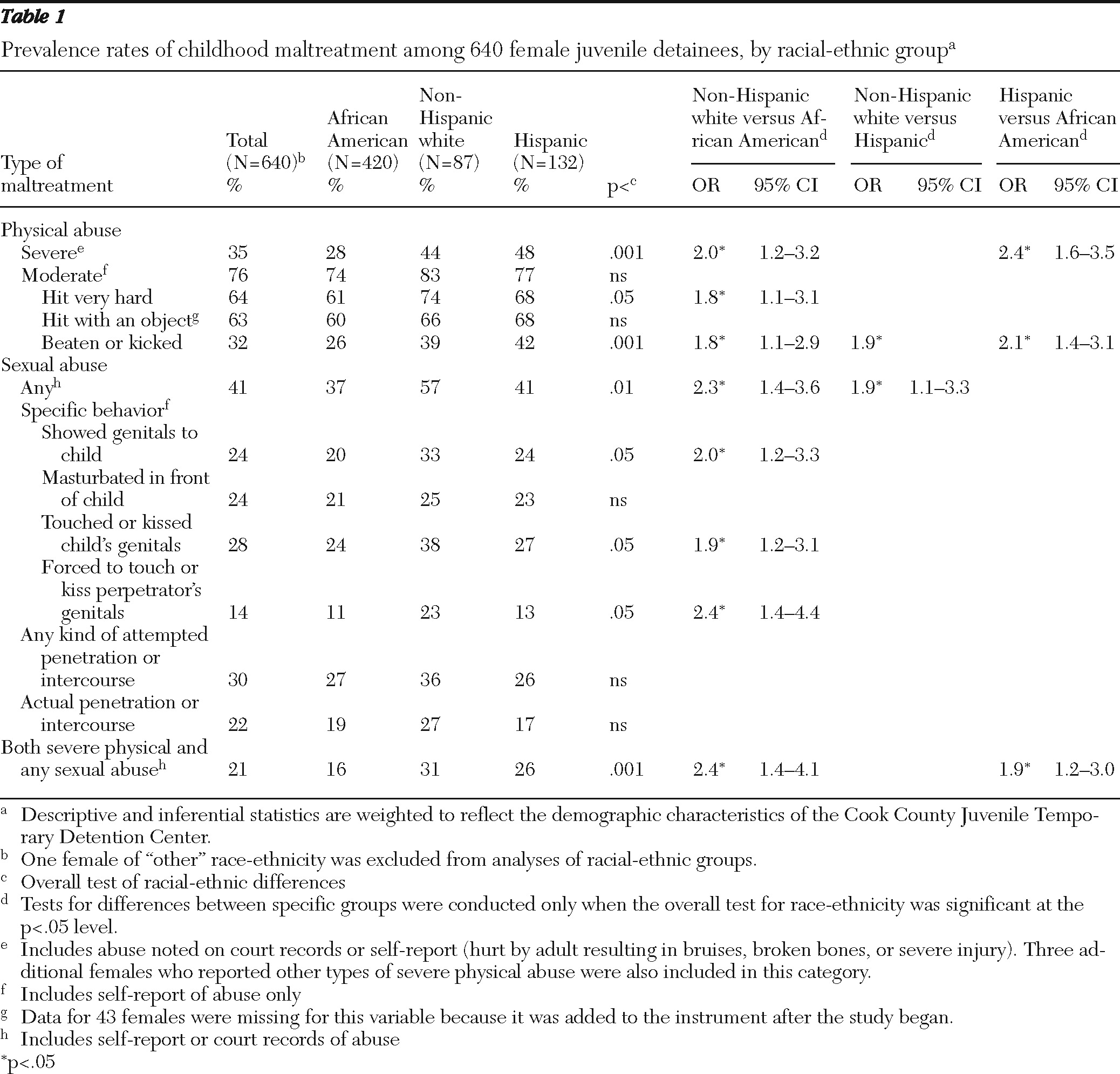
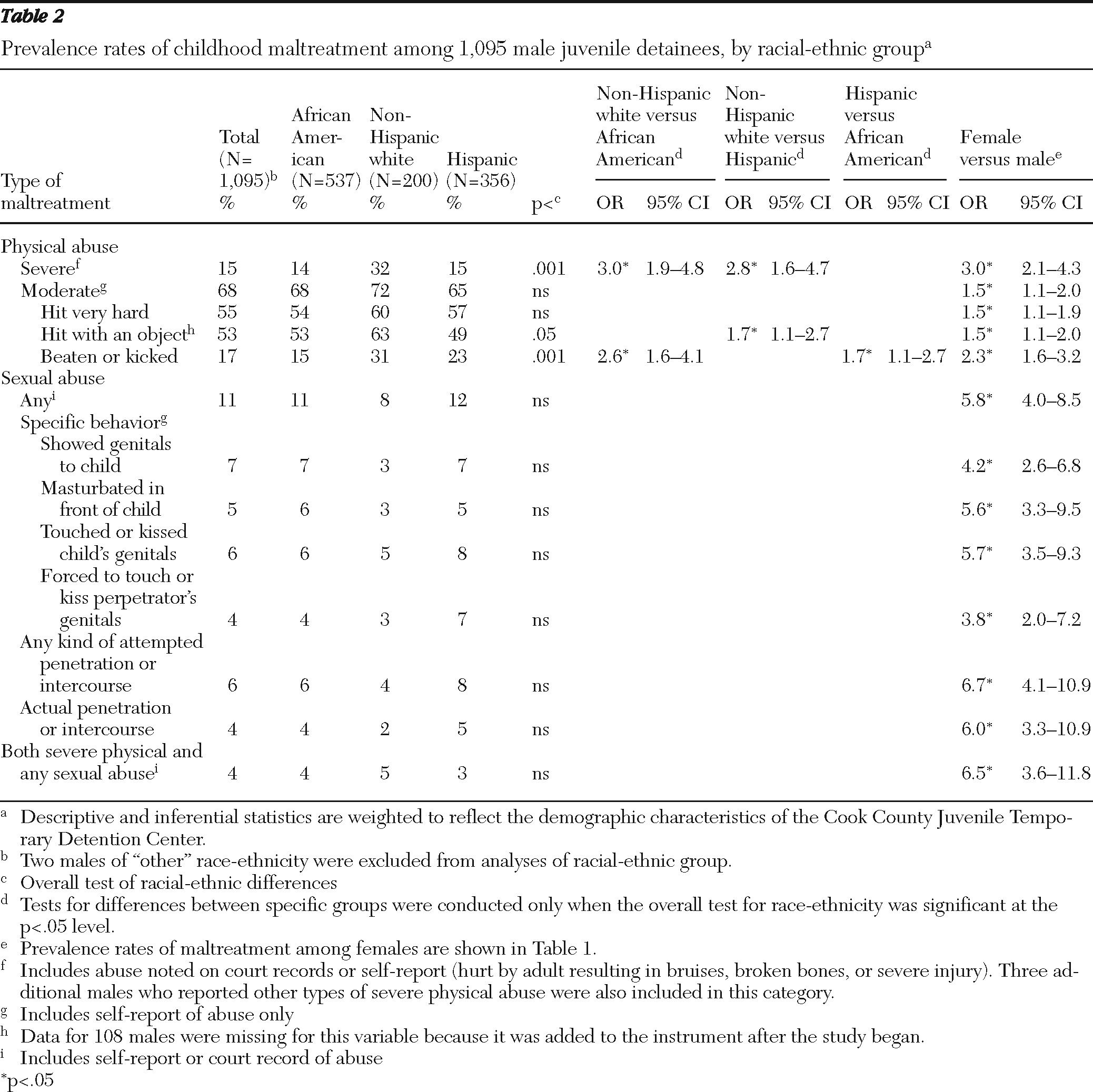
Tables 1 and
2 present prevalence rates of maltreatment among females (
Table 1) and males (
Table 2) by racial-ethnic group and odds ratios (ORs) comparing the groups.
Physical abuse.
More than three-quarters of females and more than two-thirds of males had experienced some type of physical abuse (moderate or severe) (the combined rates are not shown in the tables). More than one-third of females and 15% of males had a history of severe physical abuse. Prevalence rates of physical abuse from official records were low; 3% of females and 1% of males had court records of physical abuse (data not shown). Females had significantly higher rates than males for every type of physical abuse and were three times as likely to have been severely physically abused (OR=3.0, 95% CI 2.1–4.3;
Table 2). Among females, non-Hispanic whites and Hispanics had higher rates than African Americans of severe physical abuse and of being beaten or kicked. Non-Hispanic white males also had higher rates of several types of abuse than African American or Hispanic males, including severe physical abuse.
Sexual abuse.
Forty-one percent of females and 11% of males experienced sexual abuse. Prevalence rates of sexual abuse from official records were low: 1% of females and .1% of males had court records of sexual abuse (data not shown). Compared with males, females had nearly six times the odds of any sexual abuse and were four to seven times more likely to have experienced each type of sexual abuse (ORs in
Table 2). Among females, non-Hispanic whites were more likely to have been victims of sexual abuse than African-American or Hispanic females.
Twenty-one percent of females and 4% of males had experienced sexual and severe physical abuse. Females had more than six times the odds of experiencing both sexual and severe physical abuse compared with males.
Childhood maltreatment and psychiatric disorders
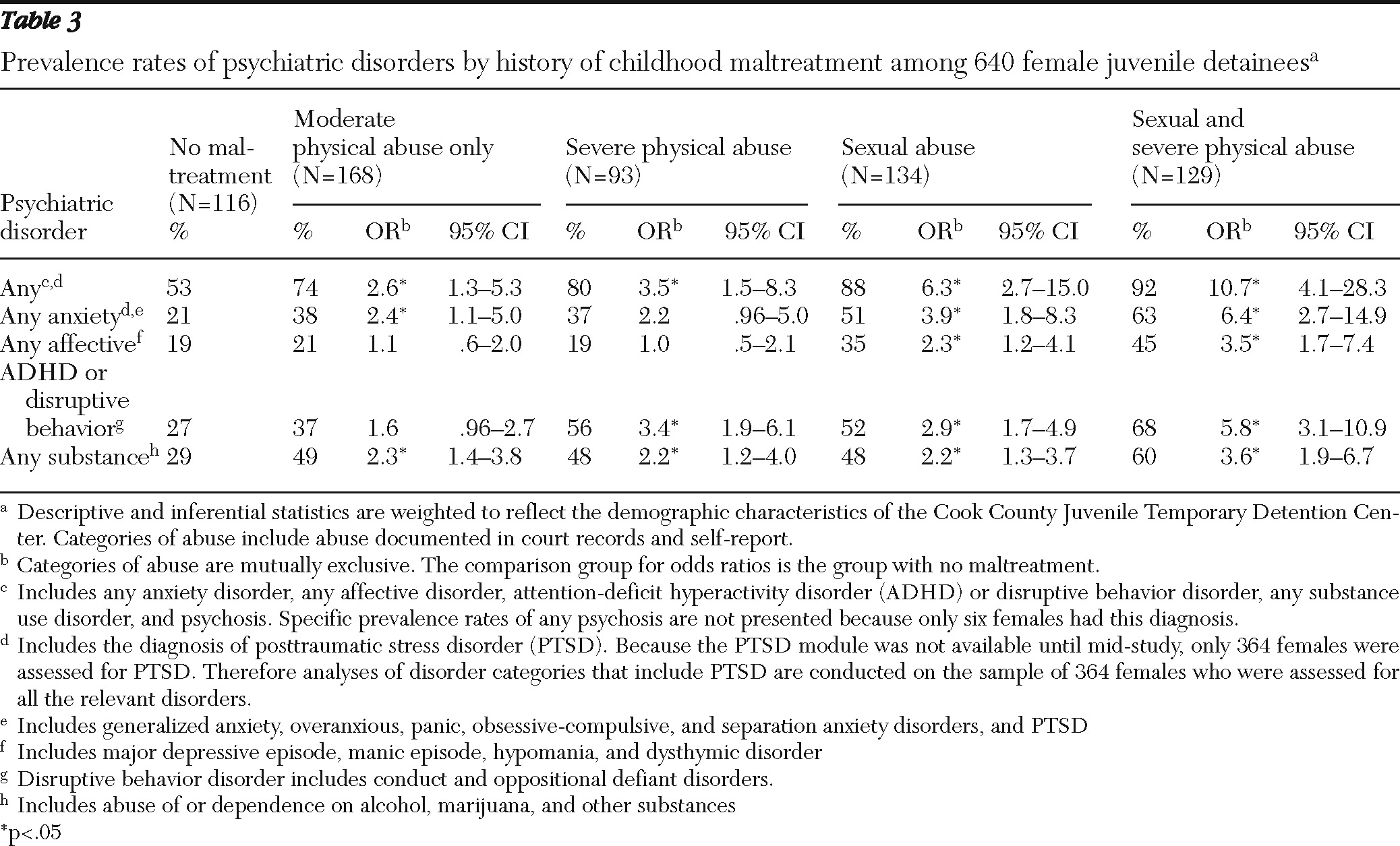
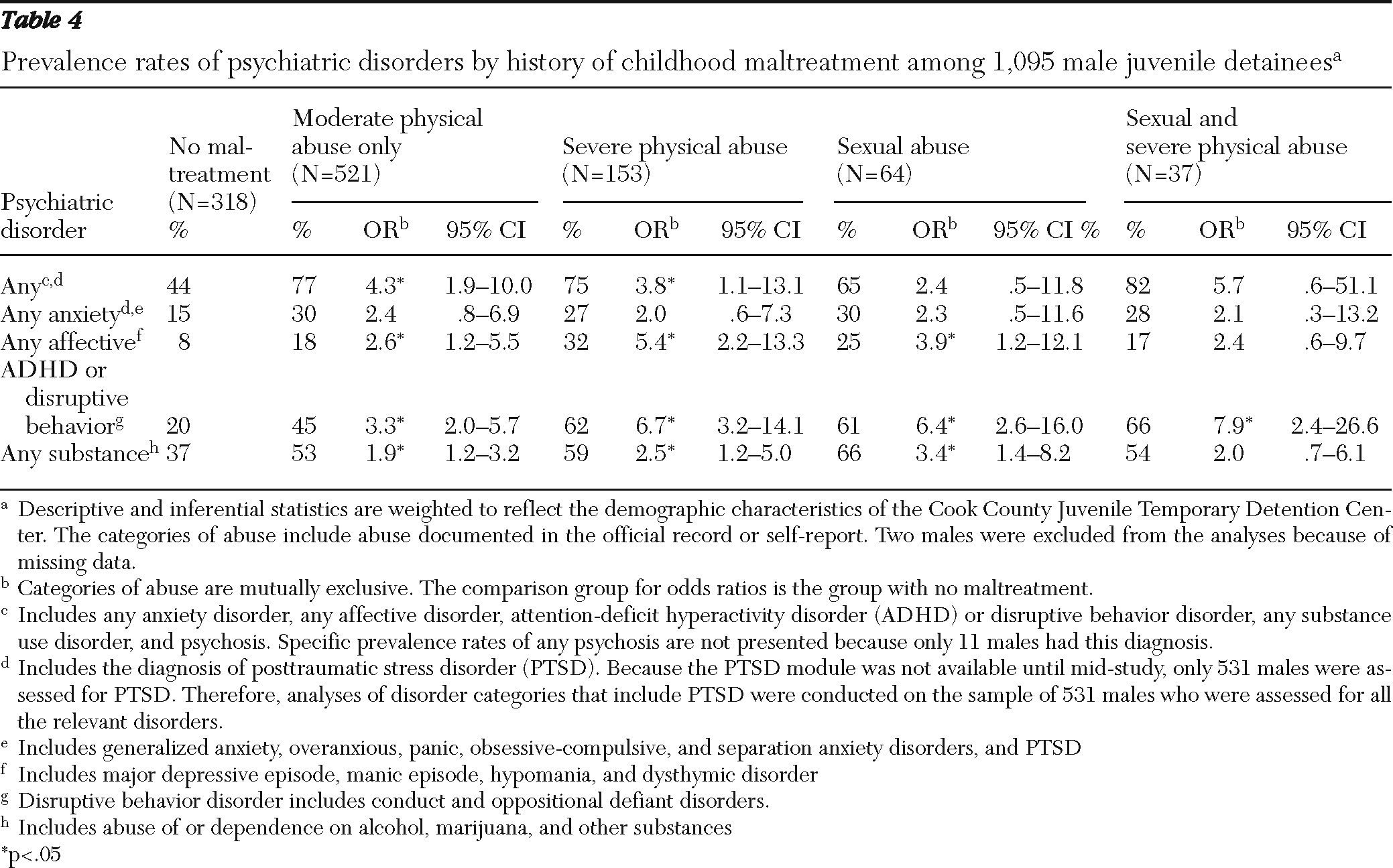
Tables 3 and
4 present prevalence rates and odds ratios describing the association between maltreatment and psychiatric disorders for females (
Table 3) and males (
Table 4). Compared with females who had no childhood maltreatment, females who had been victims of moderate physical abuse (only) were more than twice as likely to have anxiety and substance use disorders; females who had been victims of severe physical abuse were more likely to have ADHD or disruptive behavior disorders and substance use disorders. Females who had been victims of sexual abuse or victims of both sexual and severe physical abuse were more than twice as likely to have every type of disorder examined.
Compared with males who had no childhood maltreatment, males who had been victims of moderate physical abuse (only), severe physical abuse, or sexual abuse were significantly more likely to have all disorders examined except anxiety disorder. The prevalence of ADHD or disruptive behavior disorders was higher among males who experienced sexual and severe physical abuse than among those who had no maltreatment. The small number of males who experienced both sexual and severe physical abuse (N=37) may have limited our power to detect differences as statistically significant.
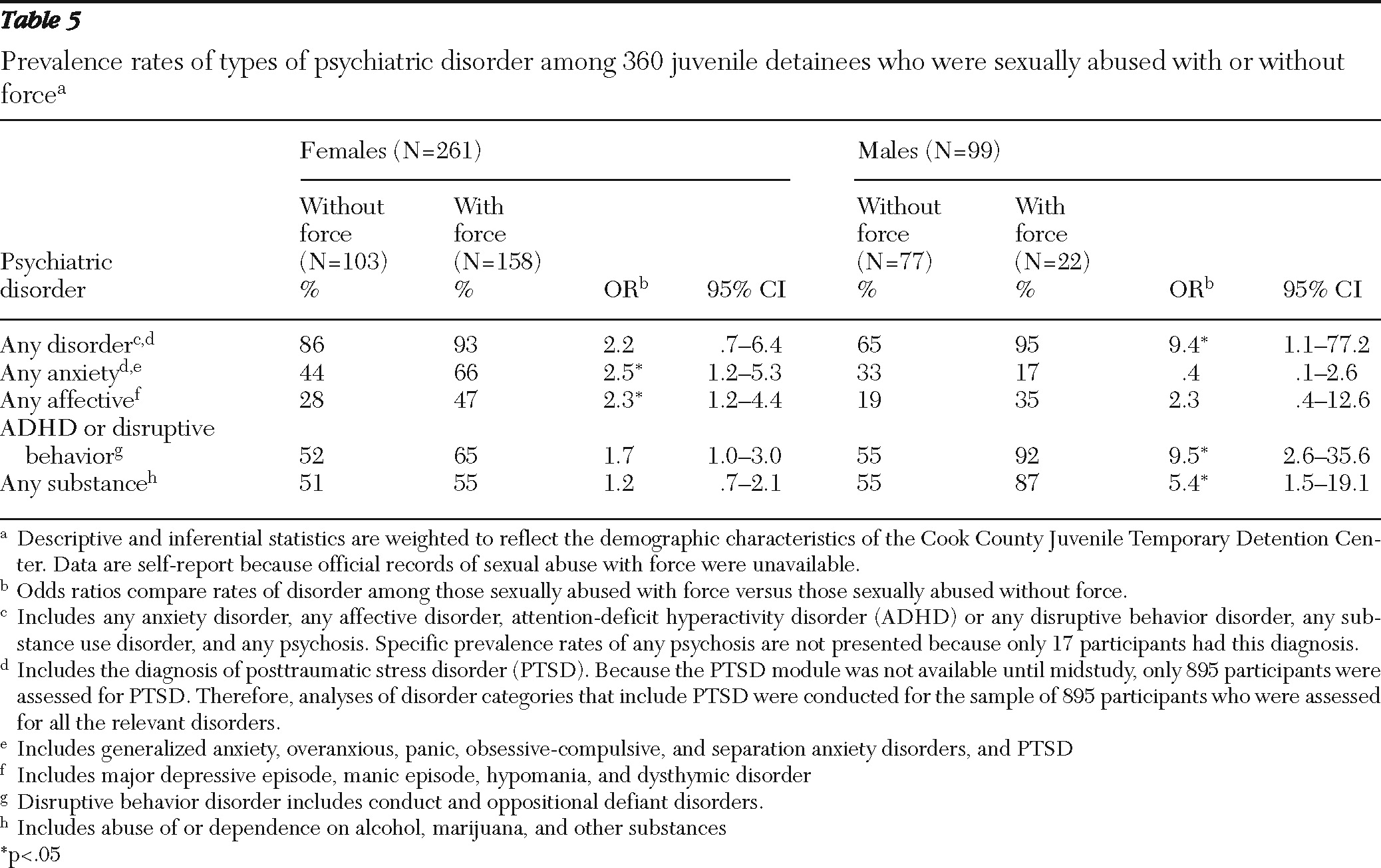
Sexual abuse with force and psychiatric disorders
Among participants who self-reported sexual abuse, 63% of females and 22% of males reported being abused with force. As shown in
Table 5, more than 90% of all youths who reported sexual abuse with force had a psychiatric disorder. Females who were abused with force had significantly higher rates of anxiety and affective disorders than females who were abused without force. Relatively few males reported sexual abuse with force (N=22); however, males abused with force had significantly higher rates of ADHD or disruptive behavior disorders and substance use disorders than those abused without force.
Discussion
The results indicate that detained youths who experienced childhood maltreatment had higher rates of psychiatric disorders than those who had not been maltreated. Nearly every type of maltreatment and combination of types was associated with increased odds of having one or more of the psychiatric disorders assessed. Prevalence rates of disorders were especially high among participants who experienced sexual abuse; nearly all youths who were sexually abused with force had a psychiatric disorder. Consistent with other studies of sexually abused children (
33–
36), our findings show that severity of sexual abuse may increase the odds of having a psychiatric disorder.
These findings are particularly important given the high prevalence rates of maltreatment in our sample and in prior studies of juvenile detainees (
2,
20). The prevalence of maltreatment among detained youths far exceeds the prevalence of maltreatment among youths in the general population (
15,
18). For example, a telephone survey of adolescents in the general population found that 13% of females and 3% of males reported a history of sexual abuse, compared with 41% of females and 11% of males in this study of detainees (
15,
18). The discrepancy is even greater for physical abuse: in the general population survey, 10% of females and 9% of males reported a history of physically abusive punishment, compared with 76% of female detainees and 68% of male detainees in this study (
15,
18).
As in a prior study of delinquent youths (
21), we found higher rates of maltreatment among non-Hispanic white detainees, especially among females. This finding differs from general population studies, which have found similar or higher rates of maltreatment among youths from racial-ethnic minority groups (
37). Our findings may reflect underlying racial-ethnic disparities in the juvenile justice system and the different pathways by which non-Hispanic whites and youths from racial-ethnic minority groups enter the system (
38,
39). For example, non-Hispanic whites, who typically have greater access to services than youths from minority groups (
40), may be less likely to be arrested. Thus non-Hispanic whites who are arrested may have more psychosocial problems, including maltreatment, than youths from minority groups who are arrested.
Prior studies of general population samples have not found consistent gender differences in the associations between types of maltreatment and types of psychiatric disorder (
33,
41). As in previous studies of youths who had been abused (
33,
41), in our study both male and female detainees who reported sexual abuse had high rates of most disorders. Our findings suggest, however, that sexual abuse with force is associated with ADHD or disruptive behavior disorders and substance use disorders among males and anxiety and affective disorders among females. We also found that among females, severe physical abuse alone was associated with ADHD or disruptive behavior disorders and substance use disorders; in contrast, among males, physical abuse was associated with affective disorders. Our data provide some support for the theory that males and females may have different vulnerability to internalizing and externalizing disorders, at least for certain types of maltreatment (
33,
41).
This study had some limitations. The findings were drawn from a single site and may not be generalizable to youths in other detention centers, especially those with different demographic characteristics. Data are subject to the limitations of self-report and official records. Participants were sampled between 1995 and 1998; findings may differ for youths currently in detention. Adolescents may underreport painful experiences, and official records underestimate actual maltreatment (
42,
43).
Statistical power may have been too low to detect some differences. For example, the small number of males who reported sexual abuse may have limited our ability to detect an association between sexual abuse with force and the presence of a psychiatric disorder. Some participants may have tended to endorse positive responses, artificially inflating the association between abuse and disorders. Findings may have differed slightly if a later version of the DISC, based on DSM-IV criteria, were available. Despite these limitations, the study has implications for treatment, public policy, and research on delinquent youths.
Conclusions
Investigate gender differences
Future studies need to investigate whether the relationship between maltreatment and psychiatric disorders is mediated by factors that affect males and females differently. For example, Meyerson and colleagues (
33) studied two dimensions of family environment—conflict and cohesion—among maltreated youths. They found that lack of family cohesion was associated with depression among males who had been maltreated; however, family conflict was a better predictor of depression for females who had been maltreated (
33). Identifying mediators that account for gender differences will help to improve gender-specific prevention and treatment models for victims of maltreatment.
Study resiliency in youths at risk
Not all victims of maltreatment develop psychiatric disorders or become delinquent. Future studies need to investigate characteristics that promote resiliency among youths already at risk. Studies should focus on characteristics that can be altered and examine when protective factors have the most impact.
Identify youths at risk
Our findings highlight the importance of assessing the presence and severity of physical and sexual abuse when conducting routine mental health evaluations in detention settings. Referral and treatment could reduce the youths' risk of revictimization, psychiatric disorders, criminal recidivism, and associated consequences (
44,
45).
Focus on rehabilitation
Rather than adopting the more punitive stance of the adult justice system, the juvenile justice system should continue to focus on the mission of rehabilitation, particularly for youths with histories of abuse. One innovative strategy, adopted by several states and other jurisdictions in the past decade (for example, New York City, Illinois, and Los Angeles County), is to integrate the juvenile justice and child welfare systems (
46,
47). Practical and philosophical barriers notwithstanding (
46), integration of these systems, as well as close collaboration with mental health services, promotes the decriminalization of many delinquent behaviors, prevents unnecessary institutionalization, and provides avenues for delinquent youths to receive necessary protective services and therapeutic services (
48).
In conclusion, this study adds to a body of literature demonstrating that a substantial proportion of youths in detention have been or are being maltreated. Maltreatment has consequences. Depending on the type of maltreatment, between 65% and 95% of youths who had been maltreated had at least one psychiatric disorder. The mental health, child welfare, and juvenile justice systems must collaborate to ensure that these youths receive the protection and care they need when they return to their communities.
Acknowledgments and disclosures
This work was supported by grants R01MH54197 and R01MH59463 from the Division of Services and Intervention Research and the Center for Mental Health Research on AIDS, National Institute of Mental Health, and grants 1999-JE-FX-1001 and 2005-JL-FX-0288 from the Office of Juvenile Justice and Delinquency Prevention, U.S. Department of Justice. Major funding was also provided by the National Institute on Drug Abuse, the Substance Abuse and Mental Health Services Administration (Center for Mental Health Services, Center for Substance Abuse Prevention, and Center for Substance Abuse Treatment), the National Institute of Health (NIH) Center on Minority Health and Health Disparities, the Centers for Disease Control and Prevention (National Center on Injury Prevention and Control and National Center for HIV, STD, and TB Prevention), the NIH Office of Behavioral and Social Sciences Research, the National Institute on Alcohol Abuse and Alcoholism, the NIH Office of Research on Women's Health, the NIH Office on Rare Diseases, the Department of Labor, the Department of Housing and Urban Development, the William T. Grant Foundation, and the Robert Wood Johnson Foundation. Additional funds were provided by the John D. and Catherine T. MacArthur Foundation, the Open Society Institute, and the Chicago Community Trust. The authors thank the participants for their time and willingness to participate. They also thank the talented field staff and the Cook County and State of Illinois systems for their cooperation.
The authors report no competing interests.