Most patients who receive mental health care do not engage in aggression during an inpatient stay, but a substantial minority do. Aggressive patients present a serious challenge to providing a safe and therapeutic environment. Estimates of the proportion of inpatients who are aggressive vary widely, but, overall, a median of 29% for acute and forensic wards over various time periods can be suggested (
1). The group of patients who are aggressive can be divided into a majority who are aggressive once or only occasionally and a minority who are aggressive repeatedly. Flannery's review (
2) estimated that the proportion of aggressive patients who engaged in more than one aggressive act during an admission ranged from 2% to 73% (median=22%). However, it should be noted that the cutoffs for classifying a patient as repeatedly aggressive varied enormously between the studies reviewed; thus direct comparisons are difficult to draw. Grassi and colleagues (
3) used a low threshold, defining repetition as more than one incident, and estimated that 41% of patients met this criterion. Owen and colleagues (
4) and Rutter and colleagues (
5), in contrast, used a high threshold (≥20 incidents) in their studies and estimated that about 11% of patients were in this category.
In terms of managing this problem, Owen and colleagues (
4) reported that there were significant differences in how staff responded to incidents involving repetitively aggressive patients, and this is not surprising. Apart from a small minority of incidents, aggression always takes place within the context of a relationship between staff and patient (
6–
8). This relationship may be only a few hours old, but it is still a relationship based on assumptions and feelings of each about the other. If the patient has been on the ward for at least a few hours and has been repeatedly aggressive, it is likely that staff will develop a certain response, including expectations about the meaning of certain risk behaviors (for example, shouting) and the likely efficacy of various options that they might use to manage the unfolding situation. In this study, we examined this idea by investigating whether the first violent incident in which a patient is involved is managed differently from subsequent incidents involving the same patient in terms of the degree of coercion used. Physical restraint is a coercive intervention that carries a risk of injury for both patient and staff (
9), and it is used as a marker of coerciveness in the analysis presented later (
10). Such coerciveness by staff can be experienced as aggression by patients, regardless of its therapeutic intention (
11).
If the degree of coercion changes with later incidents, there are two possible trends, the negative and positive feedback patterns, which we also investigated. In the first of these, on the basis of ideas of malignant alienation and burnout among people who work with patients who repeatedly self-harm (
12) or are aggressive (
13), it is possible that negative feelings toward the patient may lead to increasingly coercive interventions that are deployed uncaringly, punitively (
14), or as a way of coping with fear (
15). Unresolved feelings about a previous episode of violence (which may have occurred hours or even minutes previously) may increase the appraisal of threat and danger in subsequent episodes of disturbed behavior so that overcontrolling, coercive, and, frankly, hostile behavior is adopted by staff to manage the patient's behavior (
16). Thus, from this perspective, we predicted that, as staffs are exposed to repeated aggression from patients, staff members will increase the coerciveness of their response in reaction to the emotions generated by previous episodes of violence (a negative feedback pattern).
Conversely, if a previous episode of violence has been resolved successfully, confidence and skillfulness among staff members will grow, and the tendency to appraise disturbed behavior as personally threatening or dangerous may decrease. Early “baseline” episodes in the sequence may be dealt with coercively in that the skills to negotiate with and deescalate episodes with this particular patient have not been achieved. In later episodes, these skills may have been achieved, tailored to the individual patient, and thus can be deployed more effectively. Thus, a sense of self-efficacy (
17) could enable less coercive interventions in line with current recommendations (
18). Each episode of violence is dealt with less coercively as each episode is more and more effectively “nipped in the bud” (a positive feedback pattern). For this study we used data from a large series of violent incidents and coercive interventions in a longitudinal survey design to examine these trends.
Methods
Setting
The study took place between 1999 and 2004 in an English mental health service located in an urban area with a population of 1.5 million. It is one of only three organizations in England that provide the full range of mental health services at all three levels of security (that is, maximum- or high-security care; medium-security care; and general adult inpatient services, including acute care, care for older people, services for people with learning disabilities, and substance abuse treatment services). The high- and medium-security settings are forensic and thus distinct from general services in the sense that almost all the patients are detained because of insanity at the time of committing a criminal act or subsequently to it. The average length of stay in each setting varies greatly (about 11 years in high security, one year in medium security, and 36–48 days in general services). The data were drawn from 46 wards (approximately 920 beds) on ten separate hospital and unit sites. The study was approved by a National Health Service Research Ethics Committee, and informed consent was not required from participants because of the anonymous and routine nature of the data.
Data analysis
Incident recording took place as part of the organization's standard audit procedures in which episodes of patient behavior that were actually or potentially harmful to the patient or other people were logged. For incident type, incidents were coded to one of four categories. These categories were physical assault (actual or attempted physical aggression directed at another person), property damage (actual or attempted aggression directed at an inanimate object), threats (verbal threats, verbal abuse or physical intimidation directed at another person), and self-harm (actual or attempted harm to self or verbal threats of such harm). Intercoder agreement on this categorization in a sample coded by two independent raters was 96%, and the kappa coefficient was highly significant. Incident types were distributed as follows: 48% threats, 20% physical assault, 12% self-harm, 4% property damage, and 16% other.
Incidents were then coded according to their ordinal position in an overall sequence of incidents involving a specific patient (first, second, or third incident, for example), up to a maximum of six incidents. The last incident in the series was also noted. It must be noted that this order did not take account of discharge dates, so a series could run across several admissions. The use of physical intervention to manage the incident was precoded dichotomously according to whether a physical intervention had been used to manage the incident. Given the current practice in English mental health care (
19), this will have consisted of manually holding the patient, usually for five to ten minutes, sometimes on the floor, to regain control of the situation (
20). There will have been no recourse to mechanical aids in the restraint. Patient characteristics were recorded for each incident and included gender, age, and race and ethnicity.
Statistical analysis
The number of incidents in which physical intervention was used was calculated, and odds ratios (with 95% confidence intervals) comparing the first incident with all subsequent incidents and comparing the first three incidents in a sequence with all subsequent incidents were calculated with SPSS and the StatsDirect packages. We used the chi square test to compare physical intervention use in first, last, and other incidents. In addition, a regression analysis of factors associated with use of physical intervention was conducted.
Results
Sample
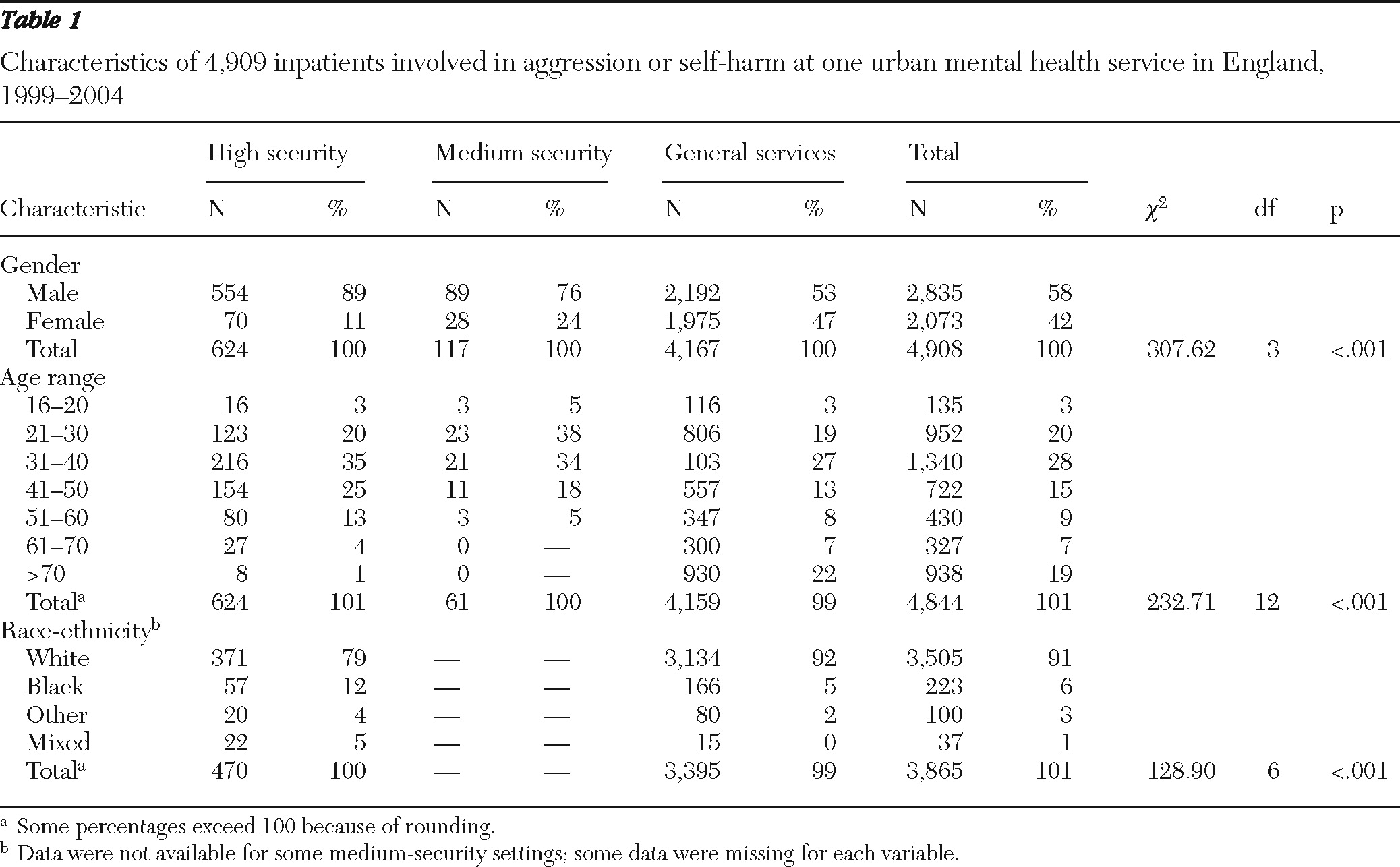
The overall sample consisted of 4,909 patients involved in one or more incidents of aggression or self-harm over a five-year period. The characteristics of this sample are reported in
Table 1. The cutoff years were chosen on the basis of the availability of data and recency in relation to the start of the study. There was some variation between settings in terms of the period covered within the overall time frame of 1999–2004. There were 20,025 incidents in the database overall, but a subset of 9,945 incidents (49.7%) was identified for analysis in the study because these incidents could be placed in a longitudinal sequence linked to an individual patient (discussed later).
Approximately 20% of all incidents were managed with physical intervention. The median length of time between first and last incidents in a series was one year from a maximum possible range of five years. The minimum length of time was one hour, but this is constrained by having one complete hour as the minimum unit of recording across the data sets. The maximum length of a series was five years. The median length of time between each incident in a series was two months. The longest time between two incidents in a series was 30 months.
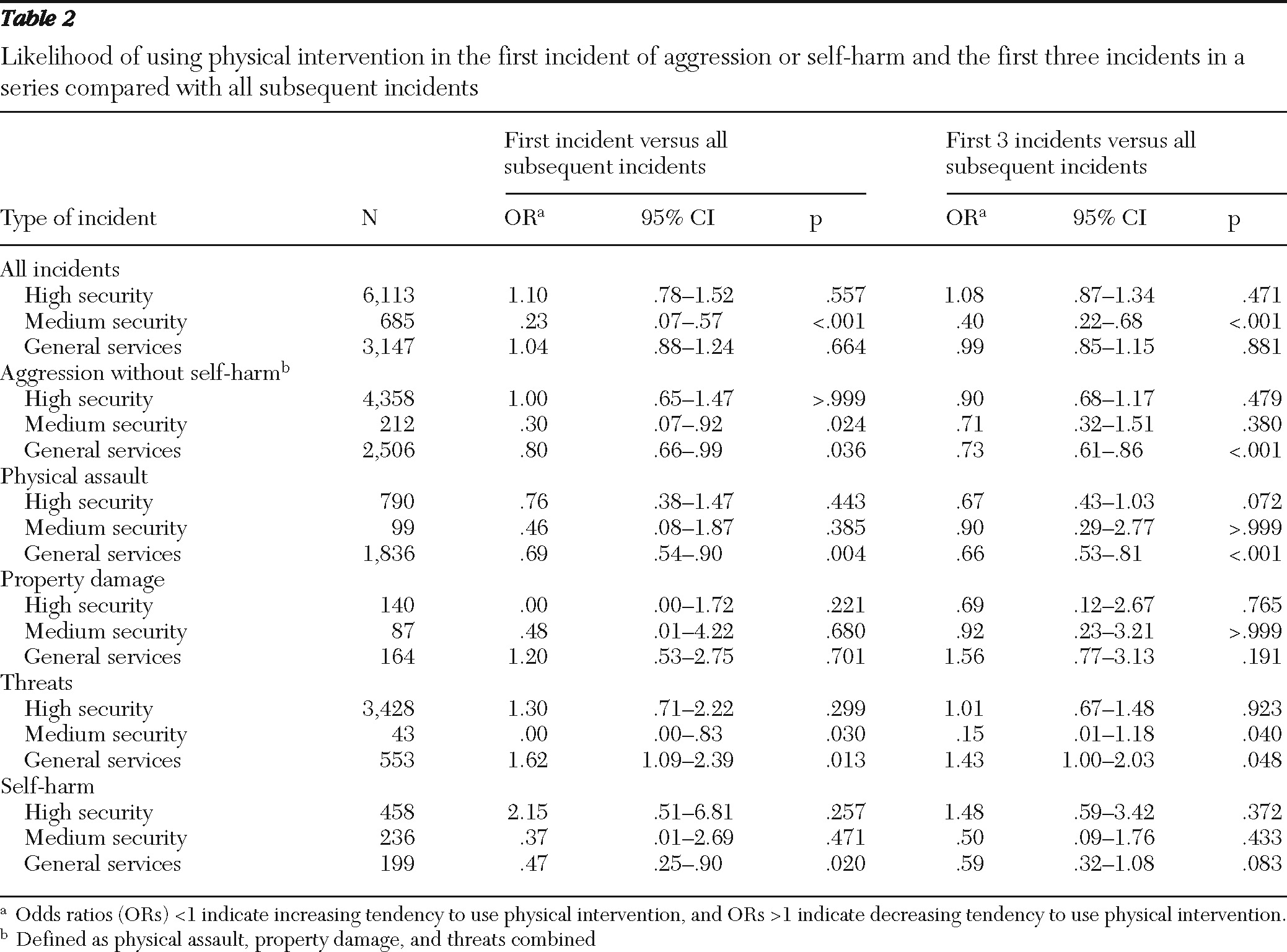
Table 2 reports the odds ratios (and 95% confidence intervals) for the likelihood of using physical intervention in the first incident in a series and in the first three incidents in a series compared with subsequent incidents. Use of physical intervention increased with repeated incidents of physical assault, as illustrated by the significant odds ratio for general services. Of 36 odds ratios reported here, 12 were statistically significant and two approached significance. Several trends are discernible in the results. First, most significant results, and all highly significant results, related to reduced odds ratios (that is, an increased tendency to use physical intervention). Second, the only trend that was the reverse of this—decreasing reliance on physical intervention—was for the management of threats in general services. Third, seven out of 12 of the significant findings were from general services, with the remainder in medium security and none in high security.
Physical intervention was significantly more likely to be used in both the first and last episodes of a series of incidents; it occurred in 42.0% of first incidents compared with 17.9% of subsequent incidents (χ2= 428.92, df=1, p<.001) and 32.9% of last incidents compared with 19.0% of previous incidents (χ2= 62.0, df=1, p<.001).
As noted, incident sequences could extend up to five years and the potential influence, in the most extreme cases, of one incident on another five years later is questionable. In other words, it may be that the observed trends only apply in short sequences. To investigate this possibility, we conducted a regression analysis to establish whether the length of any series of incidents contributed to the likelihood of the use of physical intervention. Controlling for other variables associated with a physical intervention outcome (for example, gender, age, ethnicity, nature of the incident), we found that series duration had very little impact on outcomes (exp β=.993).
Discussion
The primary goal of this study was to examine patterns of physical intervention use by staff encountering repetitive aggression from patients with a mental illness. Two possible trends in the relationship between coerciveness and repeated exposure to such aggression were anticipated. Coerciveness might increase (negative feedback) over time, perhaps because of increasing alienation and burnout, leading to a less caring approach (
14), or it may decrease (positive feedback) as staff develop a relationship with the patient based on greater confidence and willingness to use less coercive methods such as deescalation. Although the causal factors could not be examined in this data set, the trends themselves have been identified and can form the basis for speculation about the role of changes in relationships between staff and patients in such episodes.
A significant positive trend for reduced reliance on physical intervention after the first incident was noted in only one setting: the management of threats in general services. This may reflect increasing confidence among staff after the first episode that the threat would not escalate into physical assault. As such, it suggests that staff are correctly maintaining a proportionate response in the face of some provocation and not overreacting or acting punitively in this situation. Early threats issued at a point when the patient is not well known to the staff may trigger physical restraint relatively often, but as the threats are repeated, there is a process of diminishing returns in that staff perhaps learn that this is indeed “only” a threat and verbal deescalation or some form of nonphysical limit setting will be sufficient to preserve safety.
Significant negative trends indicating an increasing reliance on physical intervention over time were noted in several situations, such as physical aggression in general services and across all incident categories combined in medium security. These trends could be interpreted in a number of ways, including the suggestion that a different, less positive dynamic may be at work. The increased desire to restrain the patient may be out of genuine concern for his or her well-being, or it may reflect growing desperation and alienation from such feelings. Whatever the motivation, because subjection to restraint is highly aversive and often experienced by the patient as an unjustified assault (
21), each episode may cause resentment that forms the basis for future aggression and further restraint in an escalating cycle of aggression and restraint (
22). Nevertheless, it should also be noted that both of these trends can be viewed as appropriate responses to different types of aggressive behavior; that is, a pattern of increased use of physical intervention in response to physical assault and a concomitant decrease in response to threats can be seen as appropriate, proportionate responses rather than indications of distress in staff.
It is worth noting the policy context in which this study took place. During the study period, there was heightened awareness of the dangers of physical intervention after a particular fatal incident in 1998. This led to a number of policy initiatives and evidence-based guidelines (
18) emphasizing the need to reduce reliance on physical intervention. Positive practice standards for the care of people subjected to restraint, a national syllabus for nonphysical interventions and conflict resolution training, and a national reporting system for adverse events were introduced for forensic and nonforensic services. However, by the time these initiatives were implemented, we were at the end of the data collection period for this study, so they are unlikely to have affected staff behavior significantly. Limitations to the existing data set prevent us from assessing the impact of government guidance on the local management of violence in mental health settings. However, it seems highly likely that professional debates and discussions leading up to these policy changes may have played an important role in some of the decreasing trends noted here. What remains to be explained are the contradictory increasing trends that were observed over time in some settings.
The limitations of this study include the large variation in overall length of the incident sequences (one hour to five years) and the interincident periods (up to 30 months), indicating that both short bursts of aggression and long chains of incidents were included. Therefore, different staff members were dealing with specific patients at different times in some sequences. In addition, the data were limited to a window of truncated time so that the definition of an incident as “first” or “last” in a sequence is contestable. Also, the audit instruments on which the study was based provide only one “snapshot” point of view (that of the staff) of a complex interaction between two or more participants. These limitations indicate the need for a qualitative approach to the same issue in the future to further explore the ideas of increasing and decreasing coerciveness.
Conclusions
The principal conclusion of this study is that there are indications of potentially regular relationships emerging between some of the variables measured, so that different types of staff responses may have predictable associations with the patterning of different types of inpatient disruptiveness over time. We conclude that these patterns are sufficiently consistent to allow detailing of questions that could be investigated in further studies. First, it would be invaluable to replicate this study but with prospective data collection, monitoring incidents and types of response over a preselected period. Second, interviews with staff could more closely examine the extent to which changing practices in relation to patients were a function of changing perceptions or levels of tolerance for some types of incident as compared with others.
Acknowledgments and disclosures
This study was funded by the English Department of Health National Forensic Mental Health Research and Development Programme (ref. MRD 12/79).
The authors report no competing interests.