Not only is schizophrenia a debilitating disease due to its associated positive and negative symptoms (
1,
2), it is also considered a risk factor for many chronic medical conditions. Observational studies have found the prevalence of diabetes to be two to three times higher for individuals with schizophrenia than for the general population (
3–
5). We previously reported a large population-based study showing that the prevalence of cardiovascular disease was significantly higher among people with schizophrenia (27%) than among a control group of people without schizophrenia (17%) (
5).
Research has demonstrated that people with severe mental illness are less likely to receive medically necessary procedures for cardiovascular disease, despite the increased cardiovascular morbidity and mortality, than are those without schizophrenia (
6–
8). For example, data from the Clinical Antipsychotic Trials of Intervention Effectiveness study recognized that people with schizophrenia were inadequately diagnosed and treated for diabetes, hypertension, and dyslipidemia (
6). In addition, Kisely and colleagues (
7) confirmed that individuals with severe mental illness were significantly less likely to receive revascularization procedures than persons without a mental illness. Last, national and international guidelines for monitoring people with severe mental illness for cardiovascular risk factors and disease are available, particularly for individuals taking atypical antipsychotic agents, but these guidelines have had little impact to date on clinical care of those with mental illness (
9–
11).
Given the increased risk of cardiovascular morbidity and mortality among people with schizophrenia, the opportunity to access care is vital for primary and secondary prevention of cardiovascular disease in this population (
9). Access to a general practitioner and specialist care, where indicated, is necessary for the monitoring and management of cardiovascular risk (
9,
12). Although a number of studies have demonstrated inequities in cardiovascular care for people with schizophrenia or severe mental illness (
6–
11), little is known about access to primary and specialist care in this population. De Hert and colleagues (
9) have suggested that people with schizophrenia have substantially limited access to primary health care. Copeland and colleagues (
13) investigated trajectories of primary care use by people over the age of 50 and found that increased use was associated with improved survival but that increased use was least common among people with schizophrenia.
People with schizophrenia thus appear to have unmet health care needs. This could be a result of not enough health care in general or a suboptimal mix of primary and non-psychiatric specialist care. Either or both situations would likely result in missed opportunities for monitoring and management of cardiovascular risk factors and disease. The first step toward addressing potential unmet health care needs would be to examine population levels of general and specialty health care use. Therefore, the purpose of this project was to evaluate health care utilization and the potential opportunities for care among people with schizophrenia compared with those without schizophrenia, with a focus on cardiovascular risk factors and established coronary artery disease. We chose to examine use of specialized cardiac care services (visits to cardiologists and internists and coronary revascularization procedures) because of previous work demonstrating that, all else equal, those with schizophrenia are older and carry a greater burden of cardiovascular disease and risk factors. Our objectives were to evaluate and compare general health care utilization, including use of general practitioner visits, emergency department encounters, and hospitalizations among people with and without schizophrenia and to compare access to specialist care for individuals with coronary artery disease (internists, cardiologists) among individuals with and without schizophrenia.
Methods
Study design
A period-prevalence study design was utilized to evaluate the study objectives. Data from the administrative databases of Alberta Health and Wellness from January 1, 1995, to December 31, 2006, were used to create the study cohort. Individuals aged 20 years and older were included in this study.
Alberta Health and Wellness databases
Alberta is a Canadian province with a population of approximately 3.3 million people in 2006 (
14). Medically necessary access to physicians and hospitals within Alberta is universally provided as a result of the Canada Health Act, although individuals or families in Alberta pay a modest needs-based health insurance premium. Health insurance premiums were partially subsidized for individuals of First Nations status, those qualifying for social assistance, and individuals receiving supports for independence. The need for, and receipt of, health care subsidies represents a robust measure of lower socioeconomic status within Alberta (
15).
Alberta Health and Wellness databases utilized in the study included the Discharge Abstract Database, Alberta Physician Claims Data, the Ambulatory Care Classification System, and Vital Statistics. These databases provide deidentified information on demographics, hospitalizations, emergency department encounters, physician encounters, diagnostic and procedural codes, and mortality (
16). Diagnostic and procedural codes were based on codes from
ICD-9-CM and
ICD-10-CA. The
ICD-10-CA is a modified version of the
ICD-10 developed by the Canadian Institute for Health Information to capture morbidity in a Canadian context (
17). Alberta Health and Wellness databases include information on all individuals within the province of Alberta eligible for Alberta Health Care coverage. Essentially all Albertans (99.5%) were covered by the Alberta Health Care Insurance Plan, according to the 2006 Canadian census data (
14,
18).
Identification of schizophrenia
Individuals with schizophrenia were identified on the basis of physician claims and hospital discharge data (
ICD-9-CM 295.x or
ICD-10-CA F20.x). Rawson and colleagues (
19) previously validated the use of
ICD-9 codes in the Saskatchewan Health databases; they found a 93.9% concordance between primary hospital and chart discharge diagnoses and a 61.8% concordance between the physician service claims and primary hospital discharge diagnoses in terms of diagnosis of schizophrenia (
ICD-9-CM 295). Individuals with prevalent schizophrenia were identified from January 1, 1995, until December 31, 2006. Persons who did not meet the criteria for schizophrenia created the cohort of people without schizophrenia and were used as the comparison group for the analysis.
General practitioner, emergency department, and hospital visits
Use of health care in general was measured by examining general practitioner visits, emergency department encounters, and hospitalizations. We considered primary, urgent, and emergent health care use and hospitalizations regardless of the reason for the encounter as a broad measure of access to general health care services. Although visits to the general practitioner, emergency department, or hospitalizations may have been for psychiatric illness among people with schizophrenia, we evaluated utilization of health care services in general to identify whether the opportunity for identification and management of cardiovascular disease exists among people with schizophrenia. In addition, we also included information regarding visits to psychiatrists for people with and without schizophrenia, separate from use of health care services in general, given that most patients with schizophrenia are referred to a psychiatrist for assessment. The following data were collected: general practitioner visits and hospitalizations from January 1, 1995, to December 31, 2006, and emergency department visits from January 1, 1998, to December 31, 2006.
Cardiac disease, revascularization, and sensitivity analysis
Prevalence of coronary artery disease was identified through
ICD-9-CM and
ICD-10-CA codes. Coronary artery disease was defined as a diagnosis of acute coronary syndrome, ischemic heart disease, past myocardial infarction, or arrhythmia and was based upon previously published criteria (
16,
20).
Access to specialist care was evaluated for people, with and without schizophrenia, with coronary artery disease by comparing their access to internists and cardiologists. General internists are consultant-based specialists within Canada that manage diabetes and cardiovascular disease specifically and were therefore included in the specialist category (
21). Reasons for referral to cardiac specialist care in Canada include the cardiac conditions described above that encompass coronary artery disease and are based on clinical circumstances of the cardiac illness (
22). Revascularization was identified using procedure codes for percutaneous coronary intervention and coronary artery bypass graft from Alberta Physician Claims Data. Prevalence of coronary artery disease and revascularization was measured with data from January 1, 1995, to December 31, 2006. [An appendix providing detailed information for identification of coronary artery disease and revascularization procedures is available in an online supplement to this article at
ps.psychiatryonline.org.]
We conducted a sensitivity analysis by evaluating a non-procedure-based specialty to distinguish access to specialist care overall versus access to those who undertake expensive procedures. We completed this analysis by comparing access to specialist care, including internists and endocrinologists, among those with diabetes. Identification of diabetes was based on the established case definition of the National Diabetes Surveillance System: having two or more physician service claims for diabetes within a two-year period or one or more hospitalizations with a diabetes code as the primary, secondary, or other diagnosis (
16,
23,
24). Using this method of identification, we calculated prevalence of diabetes in the January 1, 1995, to December 31, 2006, time span.
Data analysis
Each cohort was described in terms of age, sex, receipt of health care subsidies—a marker for socioeconomic status (
15)—and urban or rural dwelling. Urban or rural dwelling was identified using the postal code for each individual. Postal codes with a zero in the second position indicate areas that are serviced by rural route mail delivery by Canada Post (
25). Individuals with the second digit of zero in the Forward Sortation Area were classified as living in a rural dwelling (
25). All other individuals were classified as residing in an urban dwelling (
25).
General practitioner encounters, emergency department encounters, and hospitalizations were compared based on any use (yes/no) and on level of use (high/low), with a median split of the mean annual visits for the entire study group. Mean annual visits were calculated for each individual by dividing the total number of visits from January 1, 1995, through December 31, 2006, by the number of years in the cohort. Specialist access and revascularization was compared between groups as a binary variable.
Multivariate logistic regression was used to compare the cohorts of people with and without schizophrenia in terms of binary variables while adjusting for variables that could potentially influence utilization of health care, including age, sex, socioeconomic status, urban versus rural dwelling, and diabetes and coronary artery disease for the general medical access models. All analyses were completed by using SPSS, version 15.0.
Ethics approval
Permission to conduct this study was granted from the University of Alberta Health Research Ethics Board Panel B.
Results
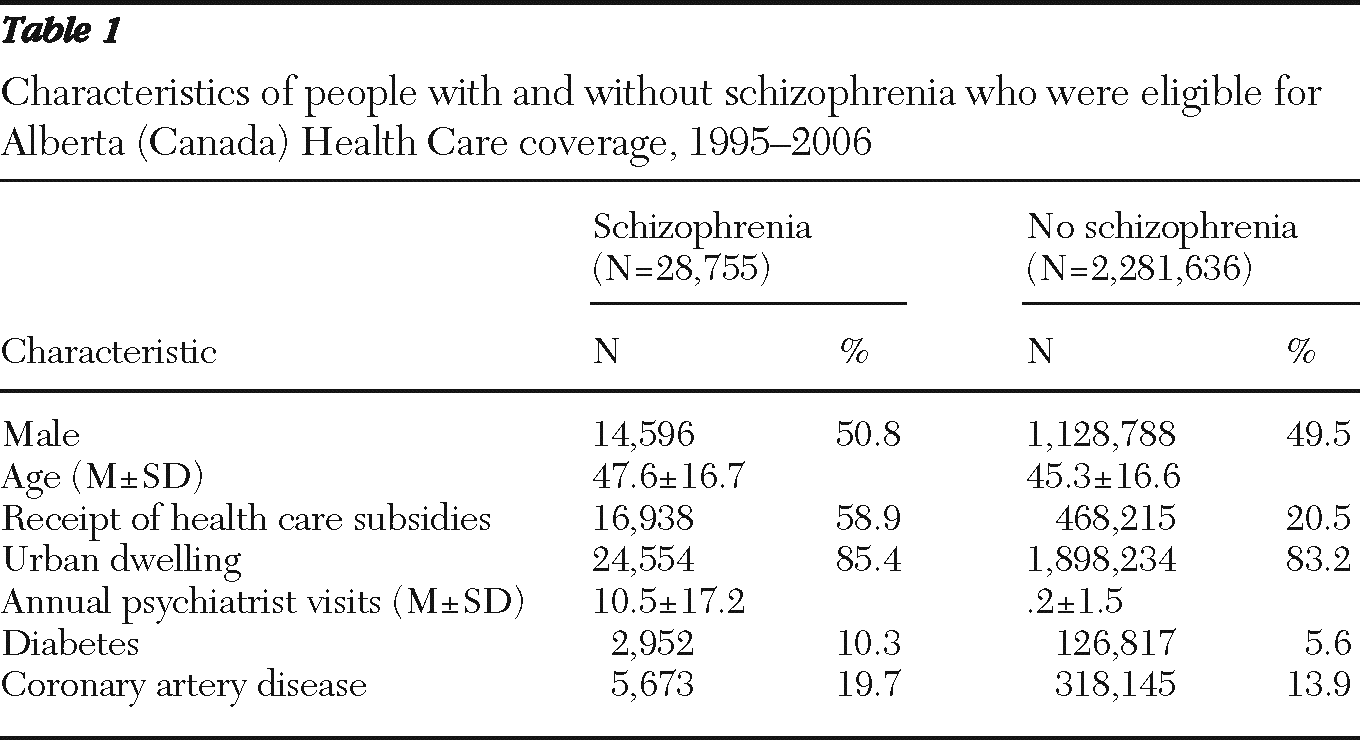
Individuals with schizophrenia (N=28,755) represented 1.2% of the sample (N=2,281,636). They were older (mean age of 48 years versus 45 years) and were more likely to have received subsidized health care funding (59% versus 21%) than individuals in the cohort without schizophrenia (
Table 1). Not surprisingly, people with schizophrenia were more likely to have visited a psychiatrist. Those with schizophrenia were more likely to have diabetes (10% versus 6%) and coronary artery disease (20% versus 14%) than those without schizophrenia.
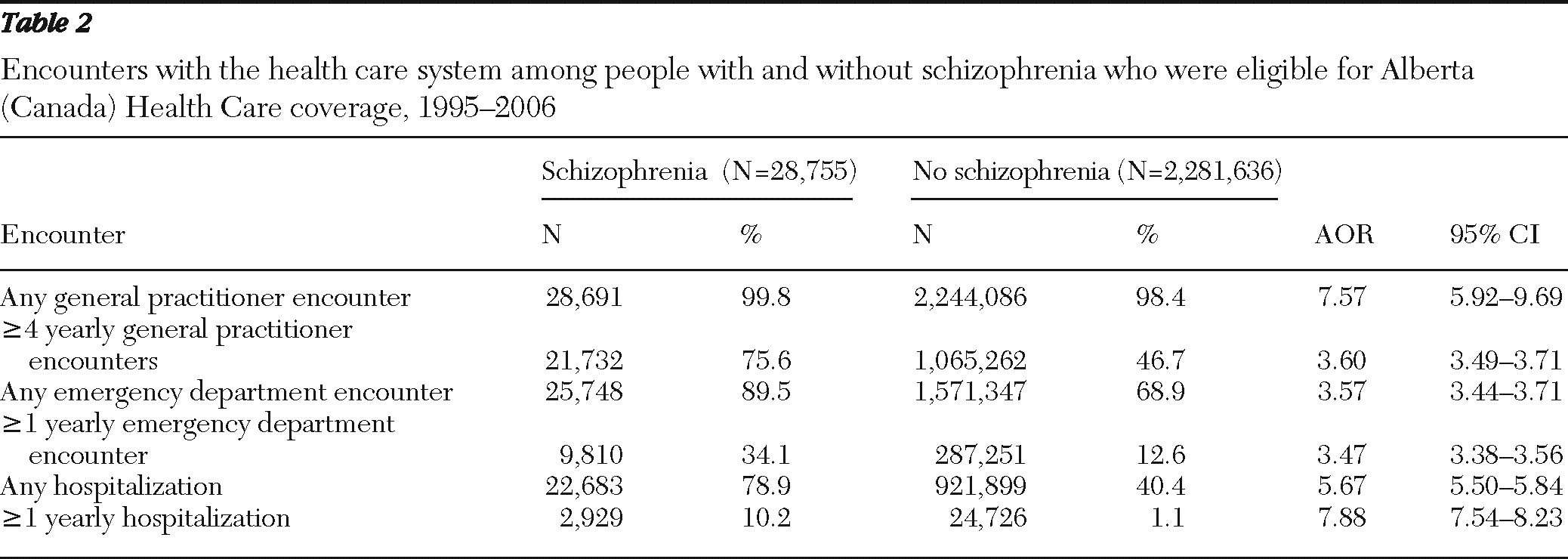
People with schizophrenia were more likely to access the health care system in general (
Table 2). Seventy-six percent of people with schizophrenia had four or more general practitioner encounters per year compared with 47% of people without schizophrenia (adjusted OR [AOR]=3.60). Likewise, people with schizophrenia were more likely to be hospitalized at least once per year (10% versus 1%; AOR=7.88) and to visit an emergency department one or more times per year (34% versus 13%; AOR=3.47) (
Table 2). Not surprisingly, people with schizophrenia were also more likely to have visited a psychiatrist than people without schizophrenia (mean±SD annual visits of 10.5±17. 2 and .2±1.5, respectively) (
Table 1).
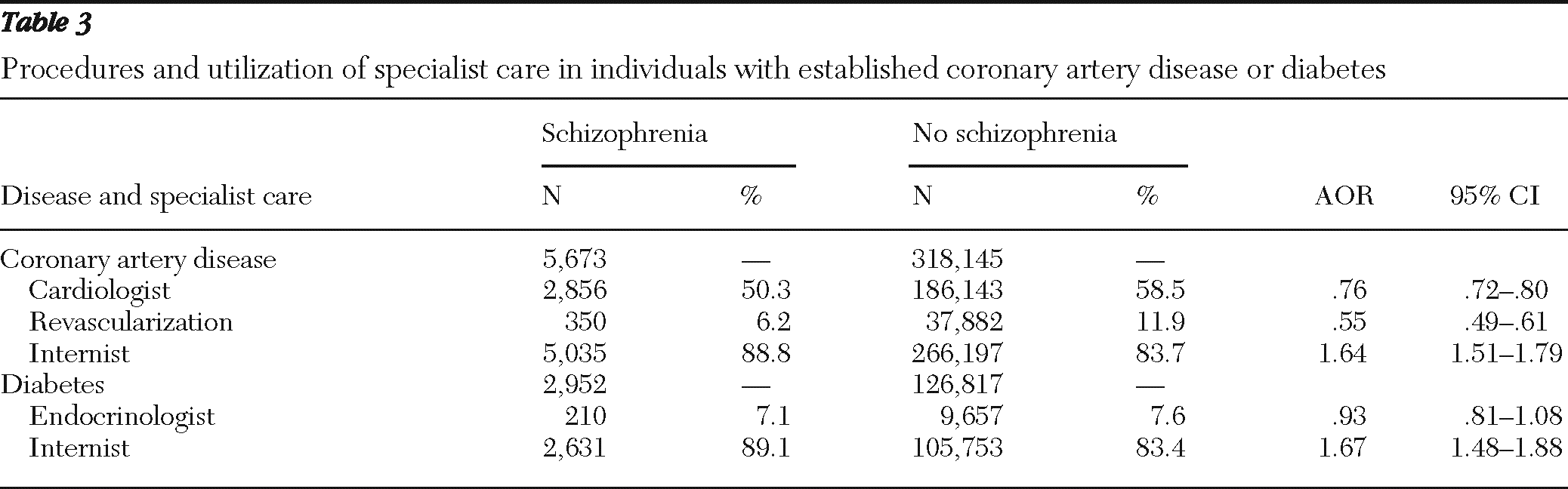
Despite having an increased prevalence of cardiovascular risk factors and coronary artery disease, individuals with schizophrenia were less likely to have received specialized cardiac care than people without schizophrenia. Cardiologist encounters (50% versus 59%; AOR=.76) and revascularization (6% versus 12%); AOR=.55) were significantly less likely among individuals with schizophrenia, whereas internist encounters were more common among people with schizophrenia (89% versus 84%; AOR=1.64) (
Table 3).
In contrast, differences were much smaller for use of less procedure-based specialty care. For individuals with diabetes, there was no difference in endocrinologist encounters (7% versus 8%; AOR=.93) compared with people without schizophrenia (
Table 3). Similar to the data found for those with coronary artery disease, people with schizophrenia and diabetes were more likely to see an internist than those without schizophrenia (89% versus 83%; AOR=1.67. [A figure comparing use of specialized care for coronary artery disease and diabetes among individuals with and without schizophrenia is available in an online appendix to this report at
ps.psychiatryonline.org.]
Discussion
Although previous research has demonstrated a discrepancy between cardiovascular care for people with schizophrenia compared with individuals without schizophrenia (
6–
11), little research has been done to evaluate why this inconsistency exists. In this large population-based study, we were able to examine access to general and specialist care among people with schizophrenia, and compare with access among people without schizophrenia, while taking into consideration important factors that may impact access to care, including socioeconomic status and urban or rural dwelling. Individuals with schizophrenia were significantly more likely than those without schizophrenia to utilize the general health care system, including general practitioner encounters, hospitalizations, and emergency department encounters. They were also significantly more likely to visit a psychiatrist more frequently than people without schizophrenia, indicating that opportunities exist for the monitoring for and management of cardiovascular abnormalities among people with schizophrenia. In addition, our results suggest that given the quantity of general care received by people with schizophrenia, the quality of care needs to be assessed to ensure appropriate management of cardiovascular risk and disease.
Despite the demonstrated use of medical care in general in this study's population, individuals with schizophrenia and coronary artery disease visited a cardiologist significantly less frequently compared with people with coronary artery disease who did not have a diagnosis of schizophrenia. Given the decreased utilization of cardiologists, our finding that prevalence of revascularization was much lower among the patients with schizophrenia and coronary artery disease is not surprising. Our results replicated similar findings by others that have demonstrated a decreased likelihood of invasive cardiac procedures among those with severe mental illness (
7,
8). In addition, it must be noted that our study was conducted in a universal health care system; thus, our results demonstrated that inequities occur in systems with universal access to health care, as has been demonstrated in previous studies in both ambulatory and hospital care (
7,
8,
26).
We did find, however, that individuals with schizophrenia and diabetes or coronary artery disease were more likely to visit an internist than were those without schizophrenia. In addition, when looking at a less procedure-based specialty, we found no difference in utilization of endocrinologists for individuals with diabetes, with or without schizophrenia. We speculate that a number of factors may be contributing to this relationship. Potentially, individuals with schizophrenia are more likely to have contraindications to revascularization that are identified at the internist level of care and are therefore not referred to cardiologists for further assessment. Alternatively, individuals with schizophrenia may be referred to cardiologists as frequently as those without schizophrenia but not attend the appointments. If this were the case, however, we would have expected to see similar results for specialist access among people with diabetes, which we did not. Last, perhaps the stigma of having a severe mental illness such as schizophrenia influences treatment decisions. Our study cannot explicitly shed light on potential mechanisms, however, and further research is needed to investigate why people with schizophrenia and coronary artery disease, in particular, are not receiving specialist cardiac care to the same extent as their counterparts without schizophrenia.
One strength of this study was the population-based approach, which includes the population of the province of Alberta aged 20 years and older. A second strength of this study was the ability to adjust for important potentially mediating variables that play a part in the relationship between schizophrenia and health care utilization, including socioeconomic status and urban or rural dwelling. Because of these strengths, the results are highly generalizable to the general population of people with schizophrenia. In addition, although some studies have evaluated receipt of revascularization among people with schizophrenia and coronary artery disease, to our knowledge very few studies have assessed access to specialist care, which is an important step in the pathway between diagnosis of coronary artery disease and receipt of revascularization procedures. Last, we conducted a sensitivity analysis to evaluate non-procedure-based specialist care among people with and without schizophrenia.
As with most studies that utilize administrative data to answer questions, our study is not without limitations. The potential for misclassification of illness existed, due to the use of physician billing codes to identify disease. In addition, although we were able to evaluate the frequency of visits to primary, urgent, and specialist care, we were unable to assess the reasons for each visit. We do not believe that this is a major limitation of this study, however, as the main purpose of this study was to evaluate whether people with schizophrenia visit the general and specialist health care system and as a result have the opportunity for monitoring and management of cardiovascular risk and disease.
Also, we were unable to evaluate the impact of lifestyle factors such as smoking status, body mass index, and blood pressure control on cardiovascular outcomes. These lifestyle factors differ between people with and without schizophrenia (
27) and may impact cardiovascular treatment decisions. In addition, although we were able to identify a discrepancy associated with cardiac care among people with schizophrenia compared with individuals without schizophrenia, we were unable to identify the reasons as to why someone with schizophrenia was less likely to visit a cardiologist. Last, we used a period-prevalence study design to examine the study objectives; therefore, the possibility of survival bias exists (
28). The potential survival bias would influence the opportunity for someone to access the health care system, particularly for illnesses such as cardiovascular disease that are associated with a high mortality rate (
29).
Conclusions
Individuals with schizophrenia and coronary artery disease were significantly less likely than their counterparts without schizophrenia to receive specialist cardiac care. Despite suggestions to the contrary, however, we found that people with schizophrenia accessed the general health care system more often than did people without schizophrenia, demonstrating that the opportunity exists to monitor and manage cardiovascular disease in this vulnerable population.
Acknowledgments and disclosures
This research was funded by a Canadian Institutes of Health Research full-time clinical fellowship and by Canadian Institutes of Health Research team grant OGT-88588.
The authors report no competing interests.