Growing literature on the effectiveness of supported housing has shown clear benefits in housing outcomes (
1–
4), but there has been little evidence of associated improvement in clinical and psychosocial outcomes. Adequate housing may be a prerequisite for psychiatric rehabilitation (
5) but may not by itself guarantee such gains. Once clients are housed, additional efforts may be needed to improve social integration, both to ensure sustained housing tenure and to enhance quality of life. One of the main tenets of the consumer and recovery movements has been to help clients live full and normal lives in spite of their symptoms (
6,
7). It can be argued that the full impact of the recovery movement has not been realized (
8) unless social integration is achieved.
Social science theories of well-being emphasize the importance of belonging to and identifying with social, political, religious, and other groups as crucial for experiencing oneself as an accepted member of society (
9). Individuals who are chronically homeless are a typically disenfranchised, socially marginalized group. Not only do many experience the stigma of being homeless or having a mental illness, or both (
10–
12), but some are migratory and not stably rooted in any location (
13–
15). One of the most common complaints of clients with severe mental illness who live by themselves, including those who were formerly homeless, is that they feel lonely, isolated, and without social support (
16–
19). Some researchers have begun to focus on how to help clients with severe mental illness become better integrated into their communities (
20).
Helping clients achieve social integration is not a new concept. Historically, community mental health centers around the United States in the postinstitutionalization era were organized around day treatment programs (
21) designed to help clients rehabilitate and reintegrate into their communities (
22,
23). More recently, there have been novel efforts, such as “citizenship” interventions, to help homeless adults with mental illness engage in community life and take more active roles in community activities (
24). Supported socialization programs also have been developed both for adults with severe mental illness (
25) and for adults who are homeless (
26). However, there has been little empirical examination of the social integration of chronically homeless adults after they are housed.
For this study, we defined social integration as a multidimensional construct, including domains of housing, work, social support, community participation, civic activity, and religious faith. Although social integration can ultimately be a highly subjective experience, we sought to examine social integration at a basic level to understand the social and community activities of a large sample of chronically homeless adults who were enrolled in a multisite supported housing initiative over a one-year period.
Methods
Program description
From 2004 to 2009, the U.S. Interagency Council on Homelessness developed a federal initiative called the Collaborative Initiative to Help End Chronic Homelessness (CICH) to provide adults who were chronically homeless with permanent housing and supportive primary health care and mental health services at 11 sites (
27). Details about CICH have been presented elsewhere (
28). Each site developed a comprehensive plan to link supports with housing, increase the use of mainstream health and mental health services, integrate systems and services, and ensure the sustainability of these efforts. None had a specific focus on social integration.
Sample
A total of 756 participants gave informed consent to participate in the evaluation of CICH. The mean number of participants at each site was 69, ranging from 52 to 98. Homeless adults were recruited by clinical and research staff at each site through a variety of methods, including community outreach and contacts with shelters and mental health agencies. Among clients who consented to participate in the evaluation, 550 (73%) had data at all three time points: baseline, six months, and 12 months. The study reported here focused on these 550 participants during their first year of program participation.
Measures
Background characteristics.
Information on sociodemographic characteristics, diagnoses, and housing history was collected from participants by CICH staff through a structured form. Three types of disabling conditions—mental health, substance abuse, or general medical—were identified at screening. The evaluation staff confirmed the conditions by clarifying the conditions noted at screening with program intake staff and by asking clients during baseline assessment interviews.
Clinical status.
The Medical Outcomes Study Short Form-12 (SF-12) (
29) consists of 12 items that generate standardized mental health and physical health subscales. A score of 50 represents the average level of functioning in the general population, and each 10-point interval represents one standard deviation. Higher scores indicate better health.
Three subscales of the Brief Symptom Inventory (BSI) (
30) were selected to measure psychoticism, depression, and anxiety. Respondents rate a list of 16 symptom items, from 0, never experience symptom, to 4, very often experience symptom. In this study, the BSI showed excellent internal consistency, with Cronbach's alpha of .92. The BSI score presented is the mean value for the three subscales.
The Addiction Severity Index (ASI) (
31), which has a six-item alcohol subscale and a 13-item drug subscale, was used to document alcohol and drug use in the past month. Each subscale combines items in a standard comparable score ranging from 0 to 1, with higher scores reflecting more serious substance use.
Housing.
The number of nights participants spent in the past three months in various settings was derived from participant self-report and categorized as nights living in own place, nights living in institution, and nights homeless. Nights living in own place was defined as nights that participants spent living in their own apartment, room, or house. Nights living in institution was defined as the number of nights in a halfway house, transitional housing, hospital, or jail. Nights homeless was defined as nights in shelters, outdoors, in vehicles, or in abandoned buildings.
Work and income.
Participants were asked whether they worked for pay and whether they did any volunteer work in the past month. They were also asked the average number of hours per week for work of each type.
Social support.
Social support was assessed by asking participants the number of types of persons they could “have counted on” (for example, friend, spouse, and clergy) in the previous three months for a short-term loan of $100, a ride to an appointment, or assistance if they felt suicidal (
32). The total mean number of types of persons was calculated for a total score ranging from 0 to 10.
Community participation.
To evaluate the extent to which individuals participated in community activities, they were asked whether they participated in each of 16 common activities (for example, going to a restaurant) during the past two weeks (
33). The total number of activities was summed, and possible scores ranged from 0 to 16, with higher scores indicating greater participation in community activities.
Civic activity.
Items on civic activity were adapted from a previous study (
34). Participants were asked whether they voted in the last local election. They were also asked whether they planned to vote in the next presidential election or in the next local election. Responses were coded as yes or no and summed for a total score ranging from 0 to 3, with higher scores indicating greater civic activity (
34).
Religious faith.
The importance of religious faith was assessed with two items adapted from a previous study (
35) that asked participants to rate how important their religious belief or faith has been in their life and how helpful their religious belief or faith has been in helping them deal with personal problems in the previous three months. Ratings were on a 4-point scale ranging from 0, not at all, to 3, extremely. The mean response was calculated for a total religious faith score.
Frequency of attendance at religious services was assessed with a separate item that asked participants to rate how frequently they attended a church, synagogue, mosque, temple, or other religious service in the previous three months. Ratings were on a 4-point scale ranging from 0, not at all, to 3, once a week or more.
Data analysis
Independent t tests and chi square tests were used to compare sociodemographic characteristics of participants with complete data and of others assessed at baseline. Levene's test for equality of variances was used, and appropriate corrections were made when assumptions were violated.
To analyze social integration over time, repeated-measures analysis of variance was used to evaluate changes in continuous dependent variables over the three time points. Mauchly's sphericity test was used to test the equality of the variances of dependent variables. Violations of assumptions of sphericity were corrected with the Greenhouse-Geisser correction. Effect sizes for significant findings were calculated with the partial eta-squared statistic (η2p). To separate the influence of clinical symptoms on social integration, these analyses were repeated with controls for baseline clinical status and change in clinical status over time.
To test differences over time on categorical dependent variables, Cochran's Q test was used. Cochran's Q is a nonparametric test specifically used for binominal dependent variables to test whether proportions are the same across repeated measures.
To examine the interrelationships between the various domains of social integration, partial correlations were examined between aggregated measures of social integration with data over one year and with controls for baseline clinical status. Partial correlations were also examined between change scores in these domains; change scores were created by subtracting 12-month values from baseline values and testing their intercorrelations. To reduce type I error, the level of significance for all tests described above was set at .01.
Results
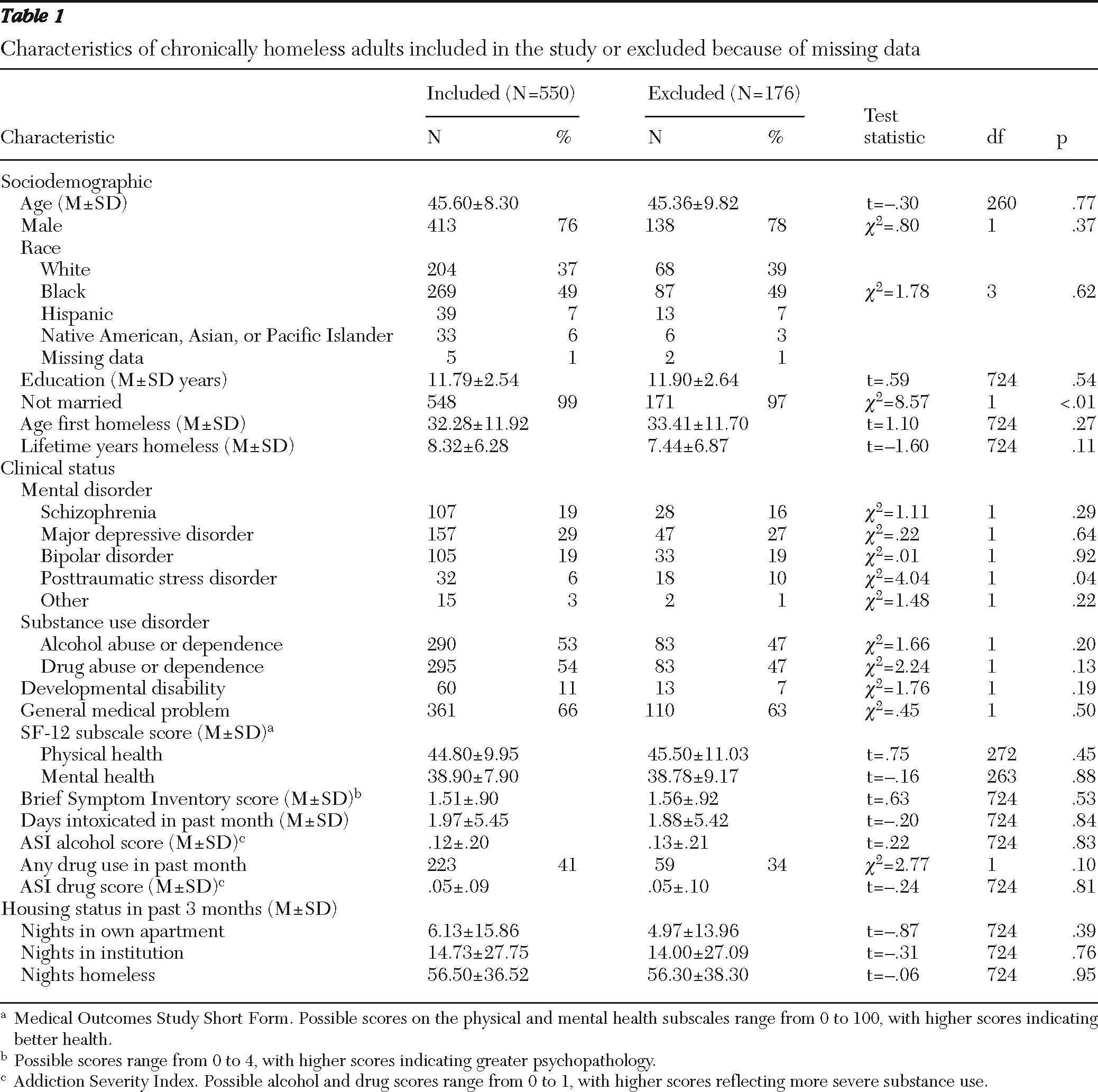
With one exception, the demographic characteristics of study participants and of the 176 individuals who were excluded because they lacked complete data did not differ significantly. The exception was that study participants were more likely to be married (
Table 1). The study sample was generally comparable to samples in previous studies of chronically homeless adults (
36–
39), although this sample appeared to have a slightly lower rate of reported substance use disorders and longer reported homeless histories. The results presented below are from analyses of the 550 participants who provided complete data at all three time points—baseline, six months, and 12 months.
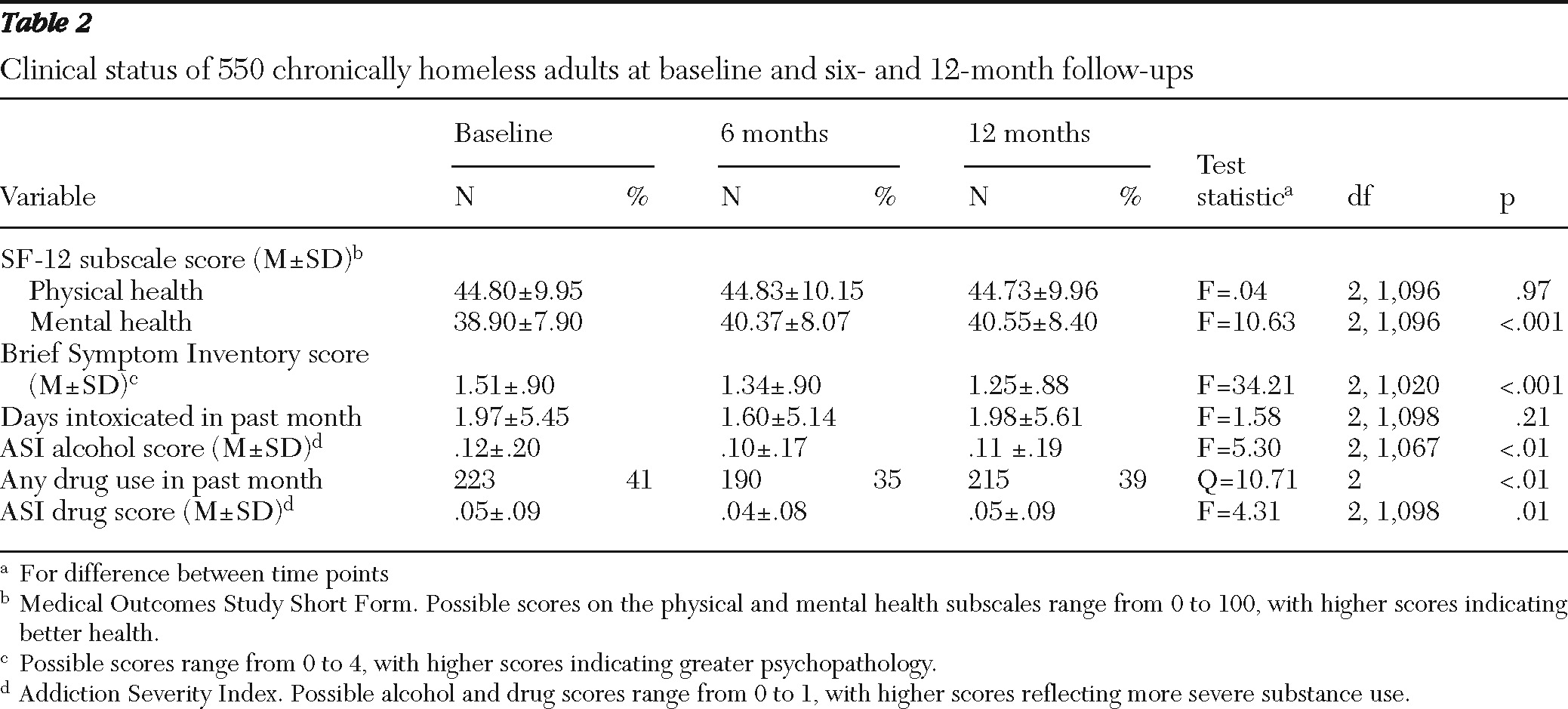
Small but statistically significant increases were observed on the SF-12 mental health subscale (
η2p=.02), indicating slight improvements in overall mental health (
Table 2). Scores decreased on the BSI (
η2p=.06) and on the ASI alcohol subscale (
η2p=.02), and the proportion of participants who reported drug use (p<.01) also decreased compared with baseline; these changes indicated significant but small improvements in clinical status.
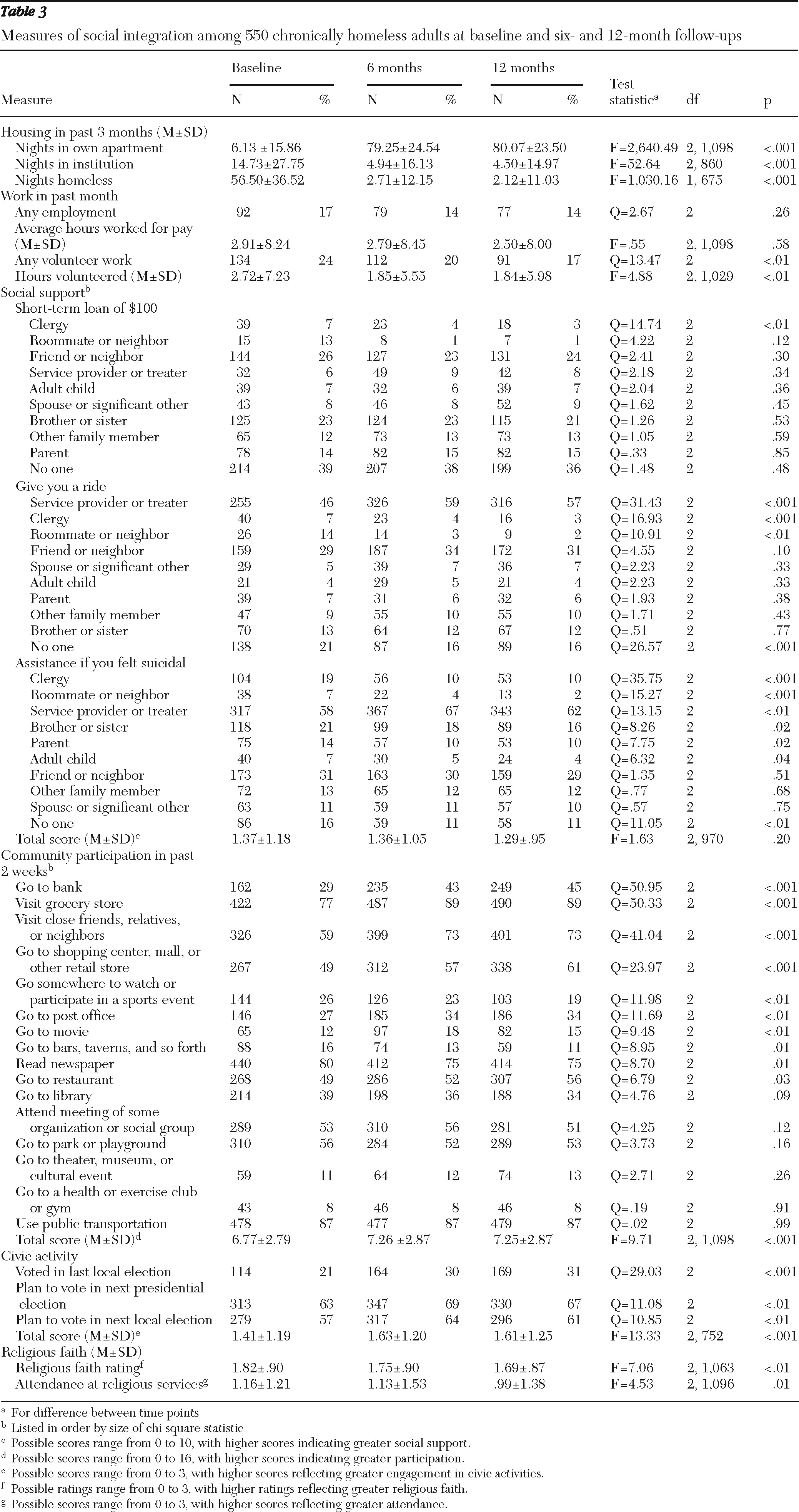
Table 3 summarizes measures of the six domains of social integration over time. After housing placement, participants spent many more nights in their own apartment (
η2p=.83) and fewer nights in institutions (
η2p=.09) or homeless (
η2p=.65). The number of participants who did volunteer work and the average number of hours volunteered declined over time (
η2p=.01). Social support total scores did not significantly change with time. However, a few significant changes were observed on individual items. Most notably, the number of participants who listed clergy as a source of social support decreased across all three scenarios (that is, for a short-term loan of $100, a ride to an appointment, or assistance if they felt suicidal). In terms of giving support for a ride or if they felt suicidal, a greater proportion of participants listed service providers compared with the proportions listing roommates or neighbors.
Participants also showed a small but statistically significant increase in their community participation over time (
η2p=.02) (
Table 3). The largest increases were in the number of participants who went to a bank; visited a grocery store; visited close friends, relatives, or neighbors; and went to a shopping center, mall, or other retail store. However, for nine of the 18 activities (50%), there was no significant change. Across time points, participants reported they engaged in an average of seven of the 16 (44%) community activities.
Participants also showed a small but significant increase in civic activity (η2p=.03). The number of participants who voted in the last local election increased, as did the number who reported that they planned to vote in the next local and presidential elections. Participants also showed a significant decrease in how important they rated their religious faith (η2p=.02); however, no significant change was observed in the frequency of attendance at religious services.
When analyses of social integration were repeated controlling for measures of baseline clinical status and change in clinical symptoms over time, all significant changes in social integration were no longer significant except for those in the housing domain (that is, the increase in nights in own apartment and the decrease in nights homeless).
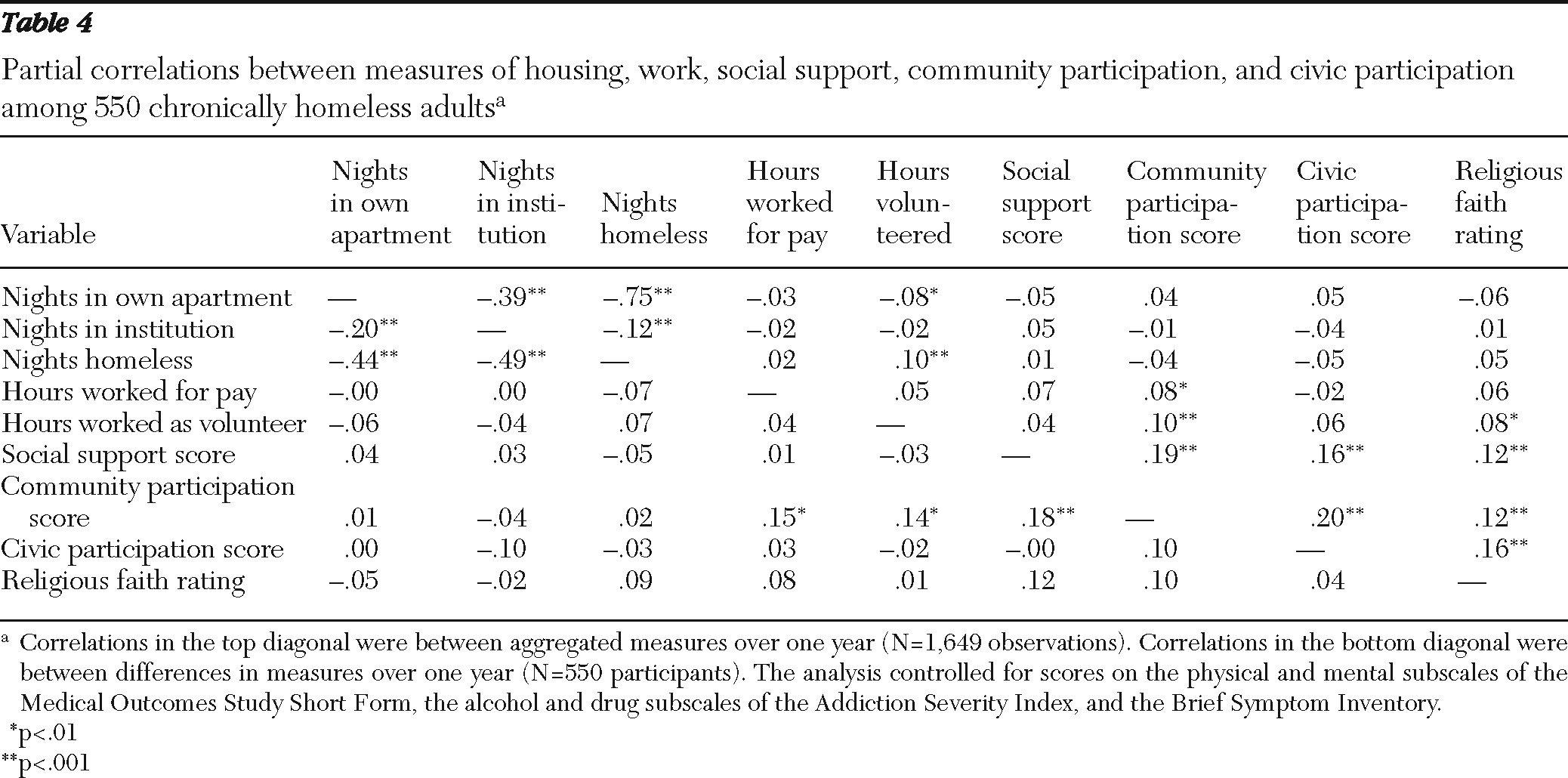
Table 4 shows partial correlations between the various domains of social integration. The upper diagonal shows the correlations between aggregated measures with controls for baseline clinical status. The strongest correlation was the link between the mutually exclusive measures of nights housed and fewer nights homeless and fewer nights living in an institution. Other notable but far more modest correlations indicated that higher community participation scores were associated with higher civic activity scores, more social support, and more hours of paid work.
The lower diagonal shows correlations between differences in measures of social integration over a one-year period with controls for differences in clinical status. These results were generally consistent in showing modest intercorrelations between measures of social integration. Again, clients who reported increased community participation also reported more social support and worked an increased number of hours for pay. In addition, an increase in community participation was positively associated with increased hours of volunteer work.
Discussion
This study described changes in social integration of a large sample of chronically homeless adults after they entered a supported housing program for one year. Although improvement in housing was dramatic, changes in other domains of social integration were minimal. Only a small increase (2%–3% of variance explained) was found in community participation, civic activity, and religious faith, and no significant improvement was found in work or social support. Furthermore, when adjustment was made for change in clinical symptoms, no significant increase was found in any domain of social integration except housing, suggesting that social integration may be partly mediated by symptom changes.
Thus, despite the clear success of CICH and other supported housing programs in the housing domain (
1–
3,
27) and the widespread appreciation of the recovery concept in recent years (
6,
7), social integration remains an area in which chronically homeless adults, even when housed, show little improvement. From baseline to one-year follow-up, on average, clients could not identify more than two types of people they could count on for social support and reported that they engaged in less than half (44%) of a list of common community activities. These results empirically show that formerly homeless individuals are often socially marginalized and isolated, which confirms previous observations (
11,
12,
16,
19). In addition, although CICH aimed to include plans to integrate systems and services, services to improve social integration were either not included in those plans or were not adequately implemented.
Not surprisingly, several of the domains of social integration were interrelated, albeit weakly. These findings recapitulate those of Strauss and Carpenter (
40) in showing that functioning consists of several semi-independent processes. In this study, community participation was positively associated with social support and employment—that is, clients who reported engaging in more community activities also identified more individuals who could provide them with social support and reported working more paid hours. However, there were many domains that were not significantly correlated, suggesting that social integration may be a heterogeneous construct. Further research is needed on which domains are causally related to each other and which are most amenable to intervention.
Several other results were of interest. Although no significant difference was found in overall social support over time, participants reported decreased support from clergy and roommates and neighbors after they obtained housing. Although it is fairly obvious why clients would report less support from roommates and neighbors after they moved into their own apartments, we can only speculate why there would be less support from clergy. Faith-based organizations have long been involved in providing social services, food, and shelter for homeless populations (
41,
42). As clients enter supported housing, they may rely less on these resources and have less contact with staff members of faith-based organizations, including clergy. We also found that as participants entered supported housing programs, there was a decrease in volunteer work. It is not clear why this occurred, but one possibility is that participants became increasingly occupied with tasks related to obtaining and maintaining their new housing.
This study was observational in nature, and we cannot rule out the possible influence of unmeasured variables on outcome measures. We did not collect data on some client characteristics, such as lifetime hospitalization history and substance abuse history, which have been found to predict outcomes (
43). The data were mostly derived from participant self-report, which is susceptible to various biases and has its limitations.
Of note, we may have used narrowly defined measures of social integration. Although we defined six domains of social integration, we did not gather data on how clients themselves wanted to be integrated and in what domains. Some proponents of the recovery movement could argue that we are imposing our standards of social integration and health, which may be the case; we acknowledge that our measures of social integration may be at variance with what clients want. Social integration may be a subjective experience that cannot be adequately measured with objective indicators, such as participation in community activities, or it may need to be measured on different levels (
20). Furthermore, the measures we used could have benefited from more thorough assessments; for example, we asked participants about voting but not about whether they were eligible to vote, and we asked about religious activities but not about nonreligious activities of atheists.
Thus further research is needed to further our understanding of whether and how clients want to become more socially integrated. Our measures of social integration did not address client experiences of choice or empowerment, which are important concepts that may be related to recovery (
8). Studies designed to replicate our findings and to specifically to test the null hypothesis should be conducted. A better understanding is needed of social integration and of the development of specific interventions to improve social integration for individuals who were formerly chronically homeless.
Conclusions
Supported housing had little effect on the social integration of chronically homeless adults. As supported housing programs continue to show success in the housing domain, clients may benefit from interventions that focus on their social integration after housing is obtained.
Acknowledgments and disclosures
The CICH Funder's Group, representing the U.S. Department of Housing and Urban Development, the U.S. Department of Health and Human Services, and the Department of Veterans Affairs, provided essential support and guidance to this evaluation. This material is also based on work supported by the Office of Research and Development, Veterans Health Administration. The views presented here are those of the authors and do not represent the position of any federal agency or of the United States government.
The authors report no competing interests.