Worldwide, suicide is among the leading causes of death and years of life lost (
1,
2). Although efforts to mitigate this burden through prevention and treatment strategies have been implemented, population-level suicide estimates remain stable (
1,
3,
4). This is one reason that suicide is still projected to be a leading cause of death in 2030 (
2). Additional research on suicide, nonfatal suicide attempts, and suicidal ideation is needed to more accurately guide large-scale interventions that could reverse these projections.
Prior research on suicidal thoughts and nonfatal attempts has been conducted in the general population in large epidemiological studies (
1,
4). Correlates of suicidal ideation found with National Comorbidity Survey Replication data include having a psychiatric condition or substance use disorder, as well as being unemployed, female, previously married, less educated, and younger (
4). Data from large populations also suggest that approximately 64% of individuals with suicidal ideation, and 79% of those who attempt suicide, seek any form of general medical or specialty treatment during the year before assessment, whereas only 44% of ideators and 61% of attempters seek specialty mental health treatment (
4). This is a particularly challenging public health problem because many of those at greatest risk of attempting suicide do not appear to seek out specialty mental health care.
Understanding factors associated with suicidal thoughts and behaviors in the general population is essential because it is often recommended that targeted prevention and treatment strategies focus on the populations at the highest risk who also may be more likely to participate in the treatment setting (
3). Nonetheless, the predictors of treatment receipt and nonreceipt in high-risk groups are not well understood. More broadly, outside a few large surveys using data from the early 2000s, there is a lack of data to describe the correlates of recent suicidal thoughts and nonfatal attempts. The main aim of the study reported here was to investigate correlates and patterns of nonreceipt of specialty psychiatric treatment (including substance abuse treatment and mental health treatment) among individuals with past-year suicidal thoughts and attempts.
Methods
Data were from the National Survey on Drug Use and Health (NSDUH) conducted in 2008 and 2009 (
5,
6). The NSDUH is a cross-sectional sample survey conducted each year throughout the United States that allows borrowing of data across multiple survey years, as demonstrated in other research (
7). This survey's main focus is on alcohol, tobacco, and drug use, but it also queries for mental health status and treatment utilization. In 2008, the NSDUH was expanded to include additional questions on mental health and suicidal thoughts and attempts (
5). The NSDUH has not yet been tapped for data on suicidal ideation or behavior and correlates of specialty treatment seeking.
The NSDUH 2008 and 2009 study populations were representative of the U.S. population. Each year the weighted screening rate for the NSDUH is near 90% and the weighted interview response rate is around 75% (
8). Individuals who are selected for the study and who agree to participate take part in an audio computer-assisted self-interview. The study protocols were reviewed and approved by the appropriate institutional review boards for the protection of human subjects in research. The total, combined sample size for the 2008 and 2009 NSDUH was 111,511 (2008, N=55,739; 2009, N=55,772). We used data from 75,690 individuals, age 18 and over, who were asked and responded to the same set of questions related to suicidal thoughts and suicide attempts.
Suicidal thoughts and suicide attempts were measured during the 12-month period before assessment with single-item yes-no response questions. Treatment utilization to address alcohol and drug use as well as for mental health specialty treatment was queried via a battery of standardized questions. Individuals who answered yes to having received either alcohol or drug abuse specialty treatment or mental health specialty treatment were considered to have received any specialty psychiatric treatment in the past 12 months.
Participants were also asked a core set of questions regarding their drug use, psychological distress, and depression during the 12-month period before assessment. First, the survey asked about use of each drug or drug category via separate single-item questions for each drug. Lifetime and past-year major depression were derived from a nine-item question series, and past-year psychological distress was determined with the psychological distress scale embedded within the NSDUH (
8). Additional demographic variables included age (18–25, 26–34, and ≥35), sex (male or female), race and ethnicity (white and non-Hispanic, black and non-Hispanic, Hispanic, Asian or Pacific Islander, and other), marital status (married, previously married, or never married), education (less than high school, high school, some college, or college graduate), health insurance (yes-no), and overall health (excellent, very good, good, and fair or poor).
Analyses involved a multistage process. First, descriptive analyses were used to generate the weighted percentage of suicidal thoughts and suicide attempts by sociodemographic variables of interest and treatment participation. Logistic regressions were then used to investigate odds of nonreceipt of specialty psychiatric treatment among those who had suicidal thoughts or attempts. All analyses were weighted to account for the complex survey sampling design. Stata version 11 was used for all statistical analyses presented (
9).
Results
In total, 3.7% of all participants experienced thoughts of suicide, whereas 1.0% made a suicide plan and .5% attempted suicide during the 12 months before assessment. Approximately 52% of those with suicidal thoughts, 64% who made a suicide plan, and 66% who attempted suicide sought any psychiatric services (mental health or alcohol or drug treatment) in the year before assessment. [Additional details on sample characteristics and specialty treatment utilization are provided in an appendix available as an online supplement to this report at
ps.psychiatryonline.org.]
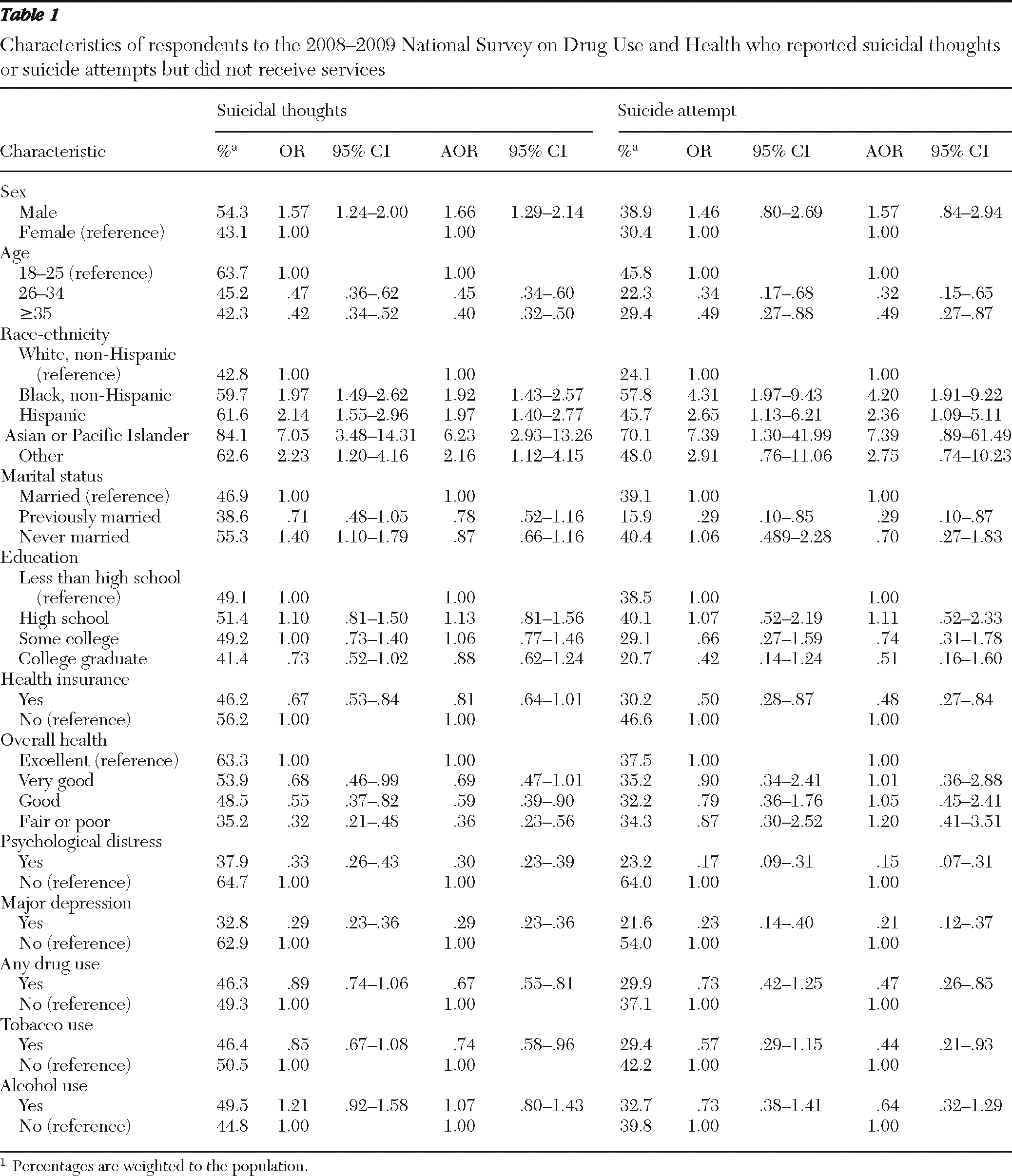
Characteristics of treatment nonreceipt were investigated among only individuals who experienced suicidal thoughts or who made attempts during the year before assessment. Individuals who were male, younger, of a racial or ethnic background other than white and non-Hispanic, and uninsured and those who had higher levels of overall health, were not depressed, and did not experience psychological distress were less likely to seek specialty treatment services. There were no differences on the basis of past-year alcohol, tobacco, or drug use in unadjusted models between those who did or did not seek services; however, when analyses adjusted for age and sex, we found that persons who used tobacco or any drug, but not alcohol, were more likely to seek services (
Table 1). In the unadjusted model, among individuals with suicidal thoughts but not suicidal attempts, those who were married sought services more often than those who were never married. Overall, there were no differences by education between those who did or did not seek services.
Discussion
The results of this study show that over 3.5% of the general population experienced suicidal thoughts, with one in 200 people attempting suicide in the past year. This finding is broadly consistent with the limited literature available from other findings with large populations (
4). Nonreceipt of specialty psychiatric treatment was common among individuals who thought about or attempted suicide. Less than two-thirds of all people who attempted suicide received any specialty mental health treatment. This finding is also consistent with earlier data reported by Kessler and colleagues (
4).
This study was the first to use the new NSDUH 2008–2009 mental health items to investigate treatment utilization patterns among those who experienced suicidal thoughts and who attempted suicide. It is not surprising that individuals who were depressed, experienced psychological distress, or used drugs were more likely to seek specialty psychiatric services. Nonetheless, it is interesting that among those with suicidal thoughts or who made attempts, the study showed that men, persons from racial-ethnic minority groups, 18- to 25-year-olds, and individuals without insurance were less likely to seek services. Typically, men are more likely to end up in treatment services for alcohol or drug use but women receive mental health services more often (
10). These results confirm other research suggesting that lack of health insurance is a barrier to psychiatric treatment utilization (
11).
This study had several important implications. The results provide essential information for health care reform and mental health parity efforts, such that mental health insurance access is one prevention strategy that may affect suicidal thoughts and attempts by altering the affordability of, and access to, treatment (
12). If individuals are able to access specialty treatment, professionals can intervene and hopefully mitigate suicidal thoughts and attempts. Also, although some programs within health care settings have shown initial success in reducing suicide among treatment seekers (
13), suicide rates within large populations have not dropped accordingly. One reason may be the large unmet need for mental health and addiction services in the United States (
14). Receipt of services may be able to help prevent suicidal thoughts before they occur, by addressing the underlying disease condition.
Another issue may be the need for better identification of persons who are at risk of suicide. Improved suicide screening in general medical settings may be able to catch individuals who fear seeking specialty mental health or addiction services. Efforts along these lines are certainly possible but may not be pursued for a number of reasons. Alcohol and drug use disorders are often missed entirely in the general health care setting—another missed opportunity to identify, and intervene with, persons at risk of suicide.
This study must be considered in the context of limitations. First, the cross-sectional, large-population survey used for this study allows the investigation of rare events (suicide behaviors), but it is difficult to determine causality and temporality of suicidal thoughts and attempts and receipt of services. Second, subgroup differences, such as by race and ethnicity, may exist in the interpretation of, and response to, each survey question related to suicide, mental health, and drug use. Third, psychiatric questions are often sensitive and stigmatizing, which may result in underestimation of the constructs. Fourth, single-item questions are not always the best measure of a construct. Nonetheless, suicidal thinking and behavior are frequently measured via a one-item question, which may be a reasonable option.
Conclusions
Despite these limitations, it remains important to assess factors that are associated with nonreceipt of specialty treatment. For instance, identification, prevention, and treatment efforts should especially target males, younger age groups, and persons from racial-ethnic minority groups, all of whom are less likely than others to appear for specialty treatment. In addition, these findings may assist health care workers to engage in outreach efforts that can target those at risk of suicide. These efforts should also increase access to services and mitigate obstacles that pose a threat to treatment engagement. In total, suicide is a major public health, family, and individual issue that affects society on all levels. Overall, more research is needed to identify the best strategies to target individuals with suicide problems who do and do not seek treatment.
Acknowledgments and disclosures
The NSDUH is funded by the Substance Abuse and Mental Health Services Administration (SAMHSA). Data analysis and writing of this article were supported by grants AA019575 and DA027832 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA). NIAAA, NIDA, and SAMHSA did not have a role in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
The authors report no competing interests.