Depression affects approximately 18% of pregnant women and 19% of women in the first three months postpartum (
1). Depression during pregnancy is associated with poor neonatal outcomes, including preterm birth and low birth weight (
2–
4). Postpartum depression is associated with impaired mother-infant interactions, poor parenting, unsafe practices (
5), and less mother-infant attachment (
6).
Among children, perinatal depression manifests itself as difficult infant temperament (
7,
8), impaired child development (
9,
10), and a higher risk for behavior problems and externalizing disorders (
11). Although the risk for postpartum depression increases with poverty—38% of women with annual incomes of less than $20,000 reported clinically significant levels of depressive symptoms (
12)—poverty itself is a barrier to receiving treatment.
To address the problem, the U.S. Health Resources and Services Administration (HRSA) initiated maternal-depression screening by Healthy Start (
13). In 2001, all 104 sites in the Healthy Start program were required to add maternal-depression screening and referral to their home visiting services. Healthy Start provides home visiting services to families living in areas with high infant mortality to achieve the goal of reducing infant mortality and morbidity. In addition, the program aims to foster development of local health systems serving these families.
In the three published evaluations of this screening initiative, two implementation models emerged (
14–
16). In the integrated model, screening and treatment were provided on site by Healthy Start staff. For example, in Tampa, Florida, home-visiting community nurses screened clients, a certified nurse-midwife conducted subsequent assessments, and a clinical social worker provided on-site treatment (
14). In contrast, in the collaborative model of screening used, for example, by the Pittsburgh and New Haven programs, home visitors screened at-risk women. Those identified as needing treatment were referred to collaborating community mental health professionals (
15,
16).
Evaluations of these three programs addressed a variety of outcomes. For example, the Florida program reported high screening rates—over a six-month period, registered nurses screened 180 of their 219 clients (82%) (
14). The proportion of women who accepted a referral for further evaluation was similar in the Florida (51%) and Pittsburgh (55%) programs (
14,
15). In Pittsburgh, however, where treatment was provided by collaborating mental health professionals, only eight of 29 (28%) women who were identified as possibly depressed accepted treatment (
15). With regard to depression outcome, two evaluations garnered contradictory data (
15,
16). In the Pittsburgh program, depression severity decreased among the eight women who received treatment, and participants reported high levels of satisfaction (
15). In contrast, the New Haven Healthy Start program evaluation reported negative depression outcome results. Notably, it was the only evaluation based on quasi-experimental data, given that women's outcomes were independently assessed and control group comparisons were included (
16).
These prior evaluations were, however, limited. Only three programs were evaluated, each assessed diverse outcomes, and only one directly assessed the primary implementation outcome—compliance with the mandate to screen (
14). Moreover, assessment of outcomes occurred almost immediately after screening was initiated and continued for only a short period of time. The short assessment period raises questions about the results because in large-scale interventions, implementation levels often improve over time (
17).
This article describes the implementation and evaluates the results of maternal-depression screening by the Des Moines Healthy Start Project. The Des Moines Healthy Start Project is a voluntary program that aims to reduce infant mortality and morbidity in families living in areas of high infant mortality. Case management services include linking families to appropriate health and mental health care providers and child development services; educating clients about nutrition, newborn care, child development, and positive parenting practices; referring clients to community resources; and providing screening services, such as child development and maternal-depression screening. Upon entry into the Healthy Start program, case managers visit weekly and then gradually decrease the number of visits to once per month as goals are met. Visits stop when the youngest child turns two years of age.
The Des Moines Healthy Start Project initially adopted a collaborative model of maternal-depression screening and referral but gradually incorporated the provision of mental health services; thus the program represents a hybrid implementation strategy. The evaluation of the program should extend the generalizability of the accumulating evidence about outcomes of the maternal-depression screening initiative. It is the first longitudinal and comprehensive evaluation that assesses compliance by a Healthy Start program with the screening mandate, as well as the rates of referral acceptance and use of treatment by program participants and their depression outcomes.
Methods
Procedures
Implementation of depression screening.
Prompted by the HRSA mandate, the Des Moines Healthy Start Project director and the second author obtained funding for four years of consultation by the first and second authors, who have expertise in perinatal depression. Together, this consultation team developed a depression screening protocol, educated the case managers who made home visits about perinatal depression, and developed treatment resources.
Depression screening protocol.
The Edinburgh Postnatal Depression Scale (EPDS) was selected as the screening tool. The EPDS is a ten-item instrument that has been validated for use with pregnant and postpartum women as well as with women with toddlers and has been translated into the many different languages spoken by Des Moines Healthy Start Project clients (
18). Possible scores range from 0 to 30. The original validation study used the Research Diagnostic Criteria for depressive illness (
19), which set the optimal cutoff score at 13 or higher, with a sensitivity of .86 and a specificity of .78 (
18). Nevertheless, to increase the sensitivity of the tool (
20) the Des Moines Healthy Start Project adopted a cutoff score of ≥12 to indicate possible depression and the need for further assessment or a treatment referral.
In line with the frequent home visits provided by case managers and the high risk for depression among low-income women (
12), the following screening schedule was adopted: patients were screened at enrollment, during their first and second trimesters, immediately after delivery, and six weeks, three months, 12 months, 18 months, and 24 months after delivery as well as at discharge from the program. Home visitors also were encouraged to screen on the basis of their clinical judgment of significant deteriorating mood. Not all women enrolled before delivery or participated until their children were two years of age. Rather, program enrollment occurred on a rolling admission and discharge basis, with women entering and leaving the program anytime during pregnancy and the first two years of their child's life.
The screening procedure included giving the EPDS to the woman to complete and then immediately reviewing the responses with her. Home visitors discussed an elevated score and offered a referral to further evaluation or treatment. If a woman with an elevated score declined the referral, the home visitor continued to monitor her mood, screening and referring according to the standard screening protocol described above.
Perinatal depression education workshops.
During the first two years of implementation, the consultation team provided monthly educational workshops about perinatal depression to the Healthy Start home visitors. In the latter two years, these workshops were provided to the other staff of the local social service agencies through which the home visitors provided Healthy Start services as well to local physicians, nurses, and social workers.
Treatment resources.
Early in the consultation, two psychologists were contracted to further evaluate women and provide them with counseling services. Mental health services were later expanded by the Healthy Start Project's director to include a community-based psychiatrist who provided evaluation and consultation as well as a full-time mental health counselor who provided individual therapy and directed postpartum depression support groups. The director also implemented “listening visits” by home visitors as part of an ongoing clinical trial (
21). To remove barriers and encourage attendance, Healthy Start provided child care, transportation, and interpretation services.
Evaluation
Because the Des Moines Healthy Start Project depression screening initiative was implemented as a clinical services program, not as a clinical trial, the evaluation relied on data available in the Des Moines Healthy Start Project database. For each Healthy Start participant enrolled between 2002 and 2009, the database included demographic characteristics, the number of EPDS screens completed, EPDS scores, referrals, and treatment use. The data provided were deidentified, so the institutional review board of the University of Iowa did not require informed consent from individual participants.
Screening protocol compliance.
The protocol incorporated ten possible occasions for screening. Depending upon when women entered the program and how long they participated, those occasions varied. For example, a woman may have started the program during her second trimester and been discharged three months after the baby's birth, a period of enrollment that would have presented six possible screening occasions—intake, second trimester, birth, six weeks and three months postpartum, and discharge. Compliance with the screening protocol was calculated as the number of times participants were screened divided by the number of screenings required by the protocol. Notably, the discharge EPDS score was excluded from this calculation of compliance because many women did not complete the discharge interview.
Referral acceptance.
Home visitors were required to suggest treatment to women who scored ≥12 on the EPDS if they were not already in treatment. The acceptance rate represents the percentage of women who accepted referral information (a list of treatment providers) from the home visitor or worked with the home visitor to schedule an appointment.
Use of treatment.
Home visitors recorded their clients' report of treatment use, including medication only, counseling only, or a combination of both.
Predictors of referral acceptance and treatment use.
The predictors examined included the EPDS score at the time of referral, ethnicity, primary language, household income, and education.
Change in depressive symptoms.
The average change between the initial elevated EPDS score and the last available score was used to assess the impact of the screening initiative.
Results
Participants
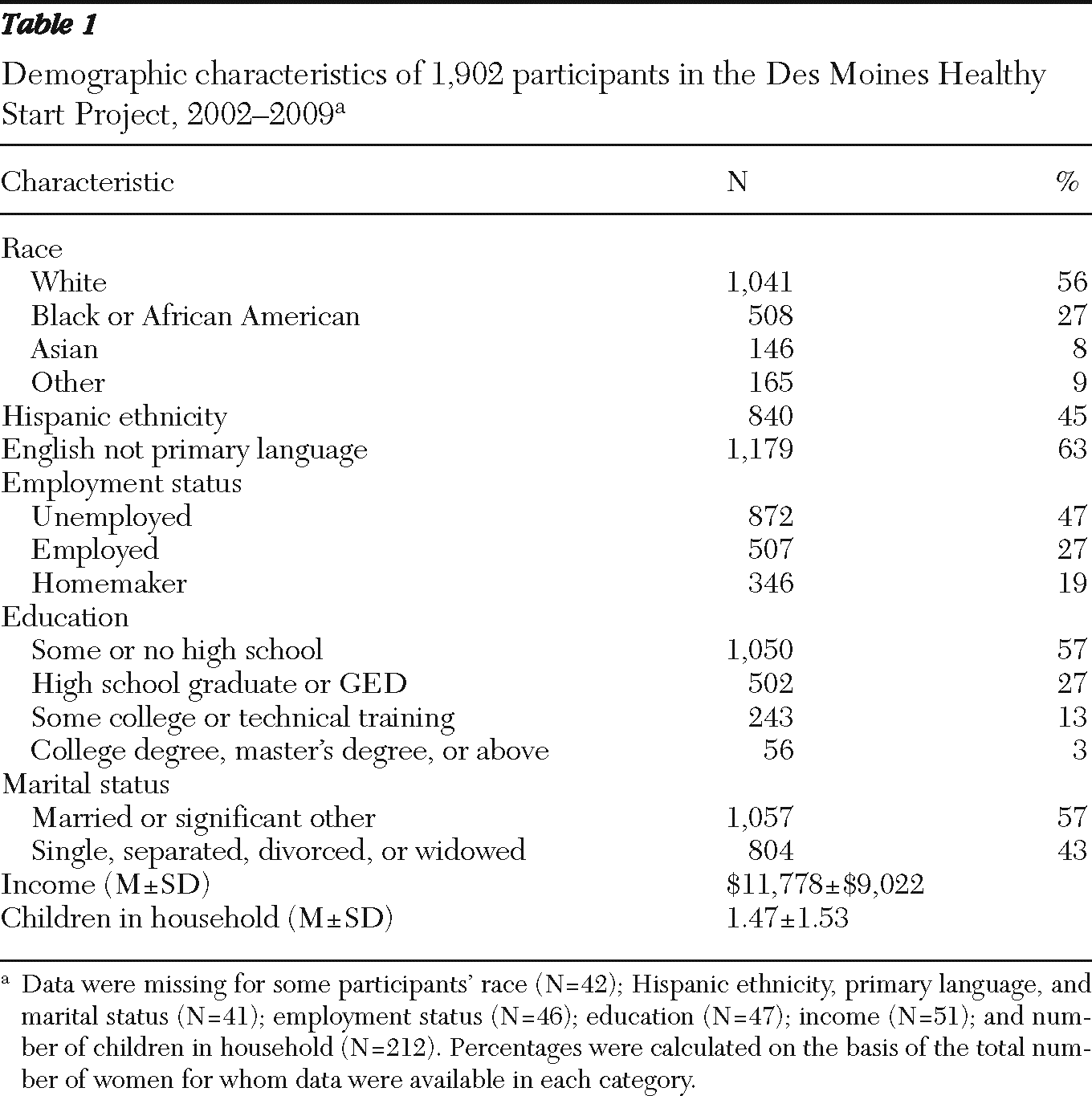
Between 2002 and 2009, a total of 1,902 women entered the Des Moines Healthy Start Project. Participants represented a racially, ethnically, and linguistically diverse group (
Table 1). The average household income was below $12,000, and 47% were unemployed. More than half were married or lived with a partner. On average, participants had 1.5 children; their ages ranged from newborn to 13).
Screening protocol compliance
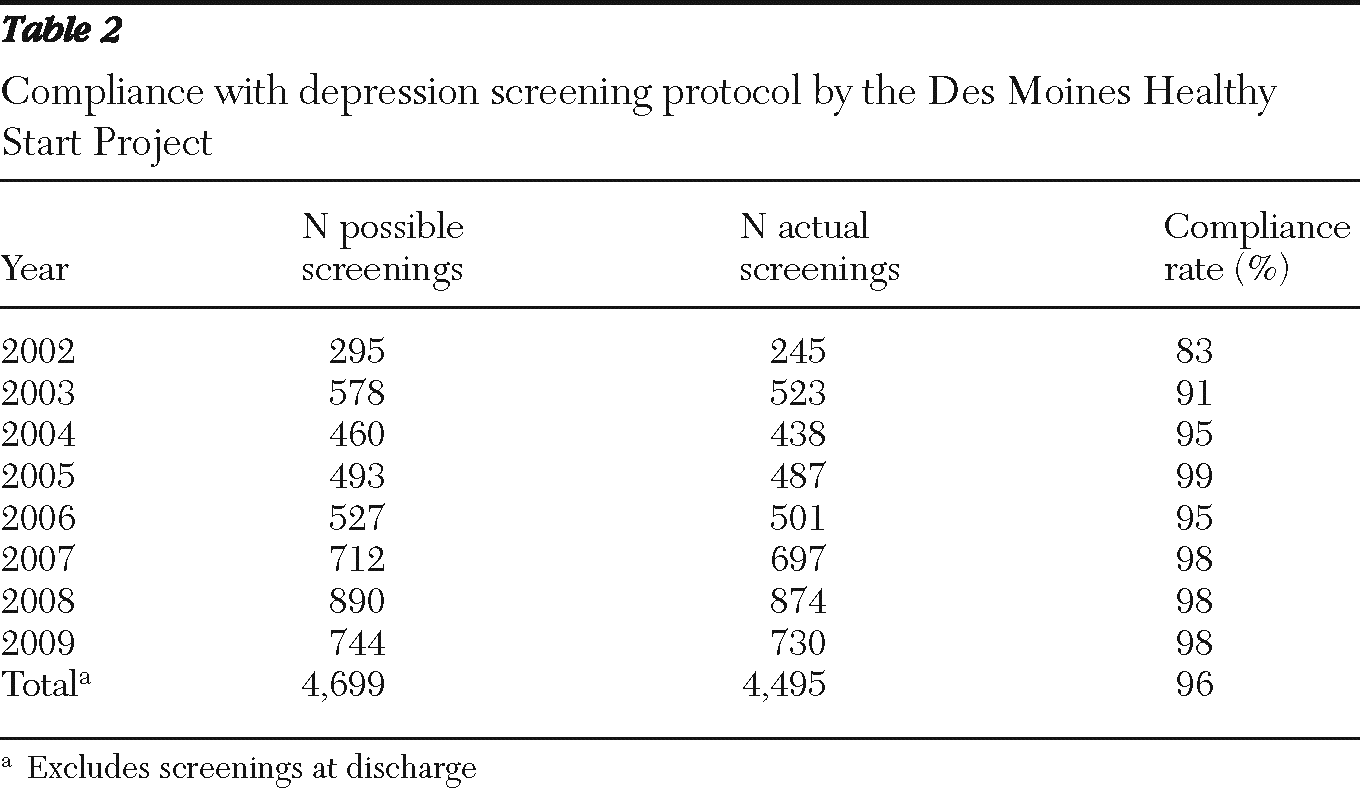
Over the eight years, compliance with the screening protocol increased (
Table 2). The compliance rate was significantly greater in 2009 than in 2002 (98% versus 83%; z=8.97, p<.05).
Referral acceptance
Of the 1,800 women screened, 581 (32%) had scores of 12 or higher at least once. Eight (1%) of these women were not offered referrals because they were already receiving treatment. Of the 573 eligible women offered referral, 370 (65%) accepted and 203 (35%) declined. [A flowchart of screening outcomes for women in the Healthy Start program is available online as a data supplement to this report.]
Use of treatment
Of the 370 women who accepted the referral, 219 sought treatment. Another 52 women who were offered a referral but who did not accept it later sought treatment. Together, 271 (47%) of women offered a referral sought treatment. Of the 258 women who provided specific information about the nature of their treatment, 149 (58%) received counseling alone, 12 (5%) received medication alone, and 97 (38%) received counseling and medication.
Predictors of referral acceptance and treatment use
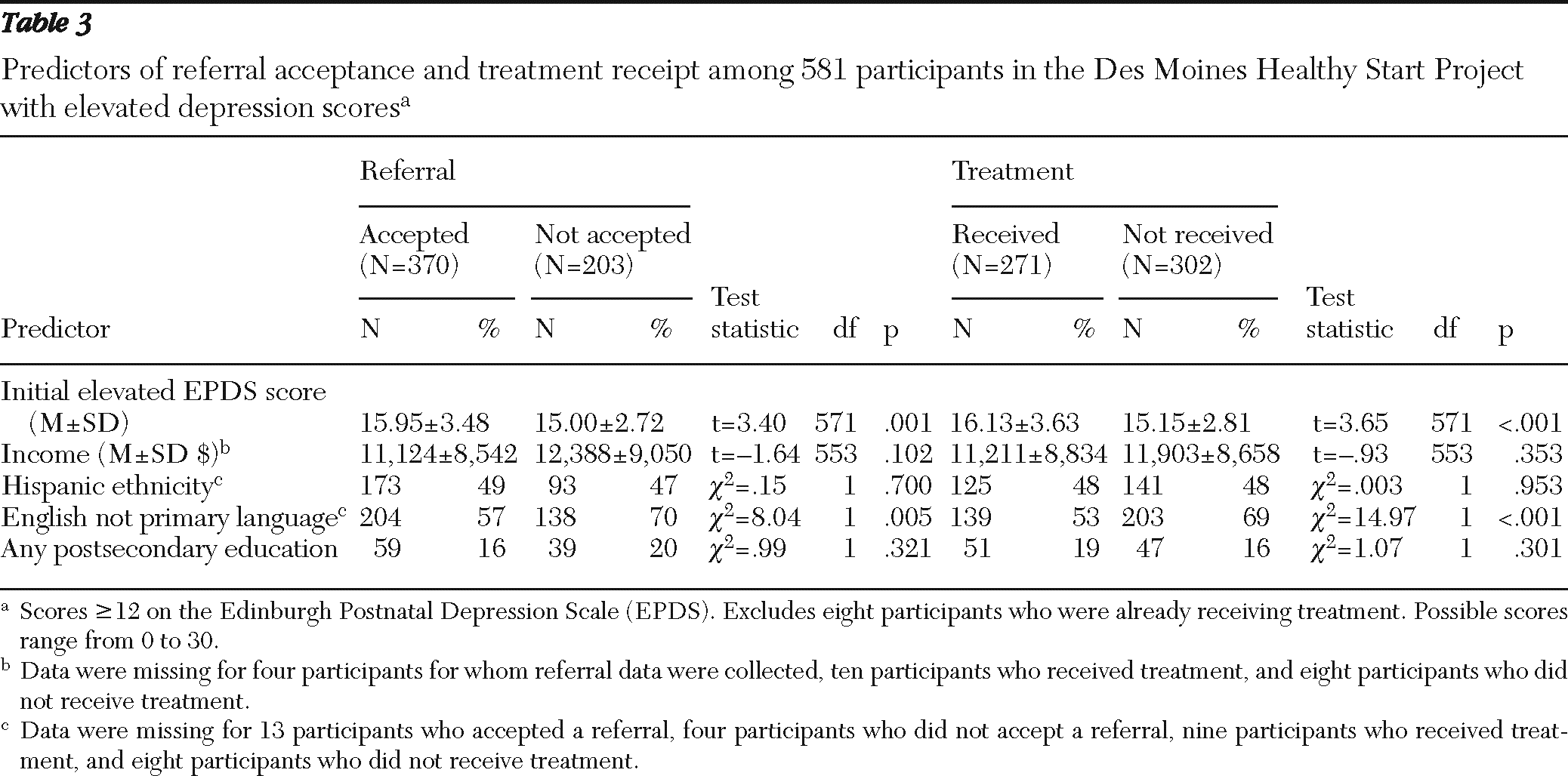
A higher EPDS score and speaking English as one's primary language predicted both acceptance of referral and treatment use (
Table 3). Ethnicity, income, and education were not significant predictors of either outcome.
Changes in depressive symptoms
The Healthy Start database contained the first elevated score and the last available score for 216 of the 271 women who received treatment. Notably, the time frame between their scores varied. On average, treatment recipients experienced a decline in depressive symptoms between their first elevated EPDS score and their last available EPDS score (16.12±3.62 versus 10.50±5.73; t=14.26, df=215, p<.001). Most (N=137, 63%) experienced at least a 4-point improvement in EPDS score, and more than half (N=125, 58%) scored <12 by the final assessment.
Discussion
Data linking maternal depression to poor infant outcome prompted HRSA to require all Healthy Start programs to incorporate depression screening and referral into their home-visiting services. This evaluation of the Des Moines Healthy Start Project is the first longitudinal and comprehensive evaluation of the federal screening initiative to assess compliance, referral acceptance, use of treatment, and depression outcome.
The results showed that the staff effectively incorporated this new practice into home-visiting services. Compliance with an intensive screening schedule—which was immediately high (83% in 2002) and increased to near perfect by 2009 (98%)—indicated that the Des Moines Healthy Start Project successfully established nearly universal screening. This positive outcome was consistent with results from the evaluation of the Tampa, Florida, program: in a six-month period, registered nurses there screened 82% of their clients. Collectively, these high screening rates support the feasibility of incorporating universal, maternal-depression screening into home visiting programs.
It is especially strategic to incorporate depression screening into home visiting programs that have regular contact with at-risk, low-income perinatal women (
12), because there is little evidence of systematic, maternal-depression screening in primary care. Screening alone, however, cannot improve maternal mental health. Accordingly, the U.S. Preventive Services Task Force recommends depression screening for adults in clinical settings to ensure accurate diagnosis, effective treatment, and follow-up (
22).
Data from the Des Moines Healthy Start Project database allowed us to draw some preliminary conclusions about the clients' experience. First, depression was not detected among two-thirds of the Healthy Start clients screened (N=1,219, 68%); this rate was consistent with an epidemiological study that included low-income women (
12) and suggested that depression is not an inevitable consequence of poverty. Second, it is notable that of the 581 women with positive screens, very few (N=8, 1%) were already receiving treatment. This result was somewhat consistent with other reports. For example, in the New Haven Healthy Start program, seven of 56 (13%) participants with elevated EPDS scores were already receiving treatment (
16). In contrast, a study of five Ontario hospitals showed that 4% to 15% of women were experiencing significant depressive symptoms, but none were receiving treatment (
23). Collectively, these results suggest that the majority of women experiencing significant depressive symptoms might not seek treatment on their own. Therefore, systematic maternal-depression screening creates a means to both increase awareness and explore the potential need for treatment.
This study examined a group of women who typically do not receive mental health services; yet the odds were high that if these women were identified as possibly depressed, they would accept referral and treatment. Of the 573 women with an elevated depression score who were not already receiving treatment, 370 (65%) accepted a treatment referral. Treatment rates were moderately high; about half (47%) of women identified as depressed indicated that they had accepted some form of treatment. The rate of treatment might have been relatively high because ultimately the Des Moines Healthy Start offered on-site depression treatment. In contrast, only 28% of women were treated in the Pittsburgh program, which implemented a collaborative model of care (
15).
Nevertheless, the treatment rates from both programs were particularly impressive compared with the low treatment rates reported by a screening program based in an obstetrics setting (
24). In that study, 689 women were identified as depressed and were provided referrals, but only 95 (14%) received treatment (
24). The comparatively high rates of treatment use determined by this and other evaluations of the Healthy Start depression screening initiative (
15) suggest that home visitors have leverage in providing this service.
Finally, among women who received treatment, depression scores significantly decreased, with over half reporting nonsymptomatic levels of depression at the final assessment. This improvement was consistent with the evaluation of the Pittsburgh Healthy Start program, in which the average EPDS score of screened, referred, and treated participants declined (
15). In contrast, in the New Haven Healthy Start program, rates of depressive symptoms after universal screening and referral were not reduced compared with rates for a Healthy Start cohort assessed before the start of maternal screening or for a group of non-Healthy Start participants (
16). This discrepancy in depression outcome might be attributable to program differences or, alternatively, may reflect differences in evaluation methodology. For example, the positive outcomes reported by the Des Moines and Pittsburgh programs may reflect the lack of a control group comparison, which was available for the New Haven Healthy Start evaluation.
A lack of control group comparisons is one of several limitations of this evaluation. First, the assessment of both depressive symptoms and treatment use was limited to self-report. Furthermore, the data available reflected only whether a woman went to treatment but did not provide information about the number of sessions she attended. This second point is important because studies have indicated that of those who seek counseling, less than half attend more than four sessions (
25); thus the high treatment rates reported here may not reflect optimal treatment use. Finally, the evaluation did not assess the impact of treatment on offspring. Nevertheless, this study is important because it is the first longitudinal assessment of the screening initiative that also assessed multiple outcomes.
In summary, the results of the Des Moines Healthy Start Project depression screening initiative were positive: depression screening was nearly universal, and rates of referral acceptance and treatment use were moderately high in a group whose depression would likely otherwise go untreated. The limited evidence available also suggested improved depression outcomes for these women.
Conclusions
With strong leadership from the federal government, maternal-depression screening has been implemented in 104 Healthy Start sites nationwide and evaluated at four of these programs. The collective findings of the four evaluations indicate two definitive, positive outcomes. First, programs have been compliant with the mandate, as evidenced by high screening rates. Indeed this initiative identified many women as having significant depressive symptoms. Second, women who were otherwise unlikely to obtain services were effectively linked to mental health professionals, although the evidence regarding outcomes for these women is still unclear. Finally, although the ultimate goal of Healthy Start is to reduce child morbidity, none of the evaluations assessed the programmatic impact on outcomes for children. Further assessment of these outcomes is therefore an important direction for future evaluations of this public health initiative.
Acknowledgments and disclosures
This research was supported by grant 1H78 MC 00025-01 from the Health Resources and Services Administration and grant K23 MH075964 from the National Institute of Mental Health.
The authors report no competing interests.