Up to one-third of adults who begin psychotherapy do not return for a second visit (
1–
3). Early dropout from therapy has been associated with younger age, lower income or educational attainment, less social support, and substance use disorders (
4–
8).
Surprisingly few data regarding outcomes of people who attend a single psychotherapy visit are available. We have reported that adults who dropped out after a first visit had milder symptoms at the time of telephone triage (
2), but no data regarding treatment outcomes were available. Among patients continuing treatment, many experience sustained improvement after a single visit (
9,
10). However, findings about patients who continue treatment may not apply to patients who do not return. We are not aware of any published data regarding outcomes of patients in community practice who discontinue psychotherapy after one visit.
This study used surveys routinely collected by a prepaid health system to examine outcomes of health plan members who did or did not return after an initial psychotherapy visit.
Methods
The Group Health Cooperative is a not-for-profit, mixed-model, prepaid health system serving approximately 650,000 members in Washington and Idaho. Members are demographically similar to the area's population and are enrolled through a mixture of employer-sponsored coverage, individual insurance, and publicly funded programs. Group Health provides specialty mental health care at seven group model mental health clinics serving members in or near the cities of Bellevue, Bremerton, Olympia, Seattle, Spokane, and Tacoma. Approximately 300 fee-for-service providers under contract with Group Health provides services to members who live elsewhere.
Group Health members may directly request specialty mental health care without referral or authorization. Members call a centralized screening program and complete a brief structured assessment of the primary problem, recent mental health treatment, perceived urgency, and risk of harm to self or others; the assessment includes screening for substance use disorders. In 2008, the most common presenting problems were depression (34%), adjustment or interpersonal problems (19%), anxiety (14%), and attention-deficit hyperactivity disorder (7%). Members are offered an appointment with a therapist at a clinic or with a participating provider.
Group Health's behavioral health service routinely mails satisfaction surveys to a random sample of patients who have visited a mental health provider (
11). Every month, health plan billing records are used to select up to ten visits by different patients for each mental health provider in the service. The patient is mailed a two-page survey about the visit that assesses satisfaction with the care of the individual provider, the facility, and the mental health department. Although only approximately 40% of surveys are completed, our previous research found no significant evidence of response bias (
11). In March of 2008, the satisfaction survey was expanded to assess patients' ratings of therapeutic alliance and improvement since starting treatment. Overall satisfaction with treatment is rated from 0 to 10, with 0 indicating the “worst possible” and 10 indicating the “best possible” mental health care (
12). A single item measuring improvement since starting treatment is rated from 1, much worse, to 5, much improved. Three items from the patient-rated version of Horvath and Luborsky's (
13) Working Alliance Inventory, a standard measure of therapeutic alliance, were selected—one from the bond subscale (“I feel my therapist appreciates me”), one from the goal subscale (“We collaborate on setting goals”), and one from the task subscale (“The way we are working with my problem is correct”). Each is rated on a 5-point scale, from 1, seldom, to 5, always.
We selected all surveys regarding initial psychotherapy visits that occurred between March 10, 2008, and September 30, 2010. Survey results were linked to computerized records regarding prior treatment, diagnosis at the index visit, and return visits to the same provider. Analyses compared survey responses of patients who did or did not return for a second visit by using chi square statistics for unadjusted comparisons and logistic regression to adjust for potential confounders. The Group Health Human Subjects Review Committee approved a waiver of consent for use of the deidentified data.
Results
A total of 2,666 patient surveys satisfied the inclusion criteria (2,030 surveys about visits to staff therapists and 636 surveys about visits to contracted network therapists). The patients' mean±SD age was 48±15 years, and 71% (N=1,893) were female. The primary diagnoses were depressive disorder (N=1,493, 56%), anxiety disorder (N=693, 26%), substance use disorder (N=107, 4%), bipolar disorder (N=107, 4%), schizophrenia or other psychotic disorder (N=52, 2%), and other conditions (N=214, 8%). For 906 (34%) of the episodes, there was no return visit to the same therapist within 45 days of the initial visit.
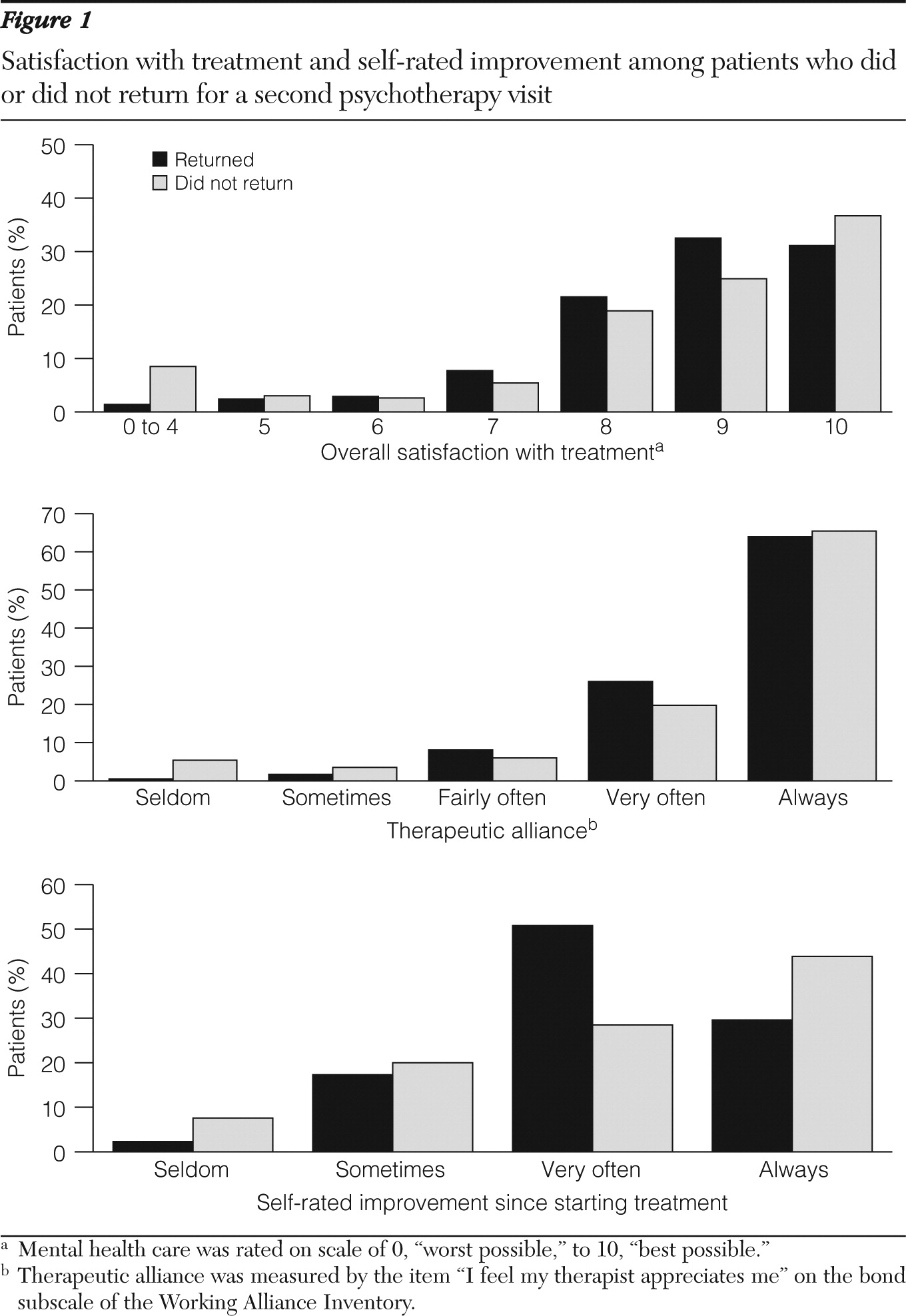
Mean scores for overall satisfaction (8.67±1.41 versus 8.28±2.45), the Working Alliance Inventory bond subscale (4.62±.70 versus 4.50±.96) and global improvement (4.07±.74 versus 4.17±.91) were roughly the same among patients who did and did not return for a second visit. The distributions of these ratings, however, differed significantly between the two groups. As shown in
Figure 1, members who did not return were more likely than those who did return to report satisfaction ratings of 0 through 4, the lowest possible (8% versus <1%), and to report a satisfaction rating of 10, the highest possible (37% versus 31%). This difference in distribution far exceeded that expected by chance (
χ2=98.6, df=6, p<.001). Similarly, the distribution of ratings of improvement (
χ2=89.5, df=3, p<.001) and scores on the Working Alliance Inventory bond subscale (
χ2=44.6, df=4, p<.001) among returning and nonreturning members differed significantly. As shown in
Figure 1, patients who did not return were more likely to report both the lowest level (8% versus 2%) and the highest level (44% versus 30%) of improvement and the lowest level of therapeutic alliance (5% versus <1%). The results for Working Alliance Inventory goal and task subscales, available online as a data supplement to this article, showed the identical pattern.
Because the associations between various predictors (satisfaction, therapeutic alliance, self-rated improvement) and returning for a second visit might be confounded by other patient characteristics, logistic regression models were used to examine the association between each predictor and likelihood of return. Given the nonlinear relationships between returning for a second visit and results of the self-rating instruments, as seen in
Figure 1, each predictor was represented by a series of indicator variables (three indicator variables to represent four levels of self-rated improvement). In each model, adjustment for potential confounding variables (patient's age and sex, primary diagnosis at the index visit, staff versus external therapist, and duration of enrollment in the health plan) had no meaningful effect on the patterns of association shown in
Figure 1. [The data are available online as a data supplement to this article.]
Discussion
One-third of adult members of a health plan who attended a psychotherapy visit did not return for a second visit. Those who did not return were more likely to report care experiences at the positive (high satisfaction, strong therapeutic alliance, and large clinical improvement) and negative extremes (low satisfaction, poor therapeutic alliance, and clinical worsening). Comparison of mean scores obscured the significant differences in the distributions of scores. The differences were not explained by patients' pretreatment characteristics.
The primary limitations of these findings included the low response rate for mailed satisfaction surveys and the brief assessments of self-rated improvement and therapeutic alliance. Our previous research (
11) found that response to satisfaction surveys was associated with female sex, older age, and longer health plan enrollment, but none of these predictors of response led to bias in assessment of satisfaction with providers. We cannot determine, however, if the findings of this study would have differed among patients who did not return satisfaction surveys. The survey included only one item that assessed clinical outcome and only three items adapted from the 48-item Working Alliance Inventory. Self-ratings of improvement may not necessarily agree with the clinical assessment of professional therapists, but they are probably more relevant to patients' decisions about continuing treatment.
Conclusions
Our findings indicated that dropout after a first therapy visit can sometimes reflect satisfying treatment and a good clinical outcome. Among patients who did not return for a second visit, approximately one-third gave the highest possible satisfaction rating, over 60% gave the highest rating for therapeutic alliance, and over 40% reported that symptoms or problems were much better since starting treatment. Fifteen percent of patients who did not return gave the highest possible ratings on all three measures. Although these outcomes may represent spontaneous recovery rather than true treatment effects, outreach to promote engagement in additional therapy would seem unnecessary for this group.
These findings, however, also supported the need for routine monitoring of outcomes. Failure to return after a first visit was also associated with the most unfavorable experience of care, and over 25% of patients who did not return reported that the symptoms or problems were unimproved or worse. For this group, outreach to promote reengagement in treatment might help to prevent unfavorable outcomes.
This pattern is similar to that seen in previous studies of dropout from antidepressant pharmacotherapy (
14). Patients who did not refill an initial antidepressant prescription included sizable groups with both favorable and unfavorable outcomes. Successful interventions to improve antidepressant pharmacotherapy were built around systematic outreach to assess outcomes and intensify services according to need (
15). Our findings point toward a similar approach to address early dropout from psychotherapy.
Acknowledgments and disclosures
The study was supported by grants P20MH068572 and R01MH081112 from the National Institute of Mental Health.
The authors report no competing interests.