Length of hospitalization among persons with serious mental illness has declined (
1–
4). In an analysis of data from the National Hospital Discharge Survey, Mechanic and colleagues (
5) found that the average length of psychiatric hospitalization declined from 12.1 to 9.6 days between 1988 and 1994. Among persons with serious mental illness, the average length of hospitalization declined from 12.8 to 9.7 days between 1995 and 2002 (
6).
Shorter hospital stays can be attributed mainly to economic factors (
7,
8). Because psychiatric hospitalization is the most expensive modality of care for people with serious mental illness, insurers have used a combination of gatekeeping and utilization review techniques to shorten hospital stays. Under some managed care plans, a case-based reimbursement mechanism has generated incentives for hospitals to shorten stays.
Sociodemographic and clinical characteristics of patients (for example, diagnosis) appear to have little effect on length of stay (
9–
14). McCrone and Phelan (
15) found that psychiatric diagnosis predicted only 3% of the variation in length of psychiatric hospitalization. Other studies have also shown that psychiatric diagnoses appear to have little value in predicting length of stay (
8,
14–
17). Previous psychiatric hospitalization (
18,
19), suicidal ideation (
20), and level of psychopathology (
17,
20) are also poor predictors, as are race, marital status, education, occupation, employment status, and living situation (
7,
14,
21,
22).
On the other hand, hospital characteristics have been found to be strong predictors of the length of hospital stays and other health service use among children, adolescents, and women with breast cancer (
9,
23). Using Medicaid claims data from 1996 to 2001, Gifford and Foster (
10) found that hospital type explained 51% of variation in length of hospitalization among youths with mental or substance use disorders. Regional characteristics have also been found to predict length of hospitalization among populations without serious mental illness (
24–
26). Ashton and colleagues (
25) found geographic differences in length of hospital stays among veterans with general medical disorders. Nguyen-Huynh and Johnston (
24) also found regional variation in length of hospitalization for stroke among Asians and Pacific Islanders in the United States. However, little is known about the effects of hospital and regional characteristics on length of hospital stays among people with serious mental illness.
Moreover, few empirical studies have used statistical models that account for the multilevel nature of length of stay (that is, hospitals are nested within regions that differ in the availability of alternative resources). Most empirical studies explaining inpatient length of stay have used ordinary least squares (OLS) regression models (
13–
15). The exception is Gifford and Foster's 2008 study (
10); however, their study was limited by the use of a single variable for hospital type (psychiatric hospital or general medical hospital), which did not account for a host of other hospital characteristics that may have an impact on length of stay.
This study examined the effects of hospital characteristics and county mental health funding characteristics on length of psychiatric hospitalization among persons with serious mental illness. The nature of our data allowed us to apply a multilevel modeling strategy to examine the extent to which contextual factors (for example, community mental health program funding) and hospital characteristics were associated with length of hospitalization among individuals with serious mental illness.
Methods
Pennsylvania inpatient discharge records and 2006 data from the American Hospital Association (
27) were used to identify psychiatric hospitalizations and hospital characteristics. Pennsylvania inpatient discharge data, collected from Uniform Bill-Patient Summary forms, were obtained from the Pennsylvania Health Care Cost Containment Council. Data from the 2000 U.S. Census were used to obtain county characteristics (
28).
The sample consisted of 106 hospitals in 42 county mental health administrative regions in Pennsylvania. Hospital discharge records from 45,497 adults with serious mental illness—a diagnosis of schizophrenia or major affective disorder (ICD-9 code 295 or 296)—from these regions were used to construct hospital-level measures. Hospitals classified as nonpsychiatric (for example, specialty substance abuse services) and hospitals in which the mean length of stay was greater than 60 days (for example, rehabilitative facilities) were excluded from the model.
To account for the structure of the data, whereby individuals are nested within hospitals and hospitals are nested within regions, we tested a three-level model in our preliminary analysis that included patients, hospitals, and regions. However, the model did not support the rationale for multilevel modeling; for example, we found no significant difference between groups. After finding that patient characteristics had little impact on length of hospitalization, we aggregated patient characteristics from each hospital to create a hospital unit of observation (that is, the percentage of patients with serious mental illness) and used a two-level model. The two-level model showed a significant difference between groups—that is, intraclass correlation coefficients (ICCs) ≥.05 (
29). This study has been approved by the University of Pennsylvania Institutional Review Board.
Study variables
Study variables were based on the extended version of Andersen's behavioral model of health care utilization (
30–
32) that was adapted to vulnerable populations (
33–
36). The conceptual framework specifies the role of predisposing factors (such as age and gender), enabling factors (such as income and insurance status), and need factors (such as perceived health status and diagnosis) as individual determinants of access and health care utilization. Just as important, however, are variables related to the mental health delivery system, such as resources (for example, geographical distribution of hospitals) and organizational features (for example, system structure) (
37) that may mediate the length of hospitalization. Although these contextual variables have been employed extensively to explain health care use (
38–
42), they have been largely neglected in studies of use of psychiatric care.
Two sets of variables were constructed: level 1 variables included hospital characteristics based on patient case mix and organizational factors, and level 2 variables included regional and county mental health program characteristics.
Level 1: case mix.
Patient characteristics at the facility level included age, gender, race, diagnosis, admission type, insurance status, readmission rate, and percentage of patients with a serious mental illness. All categorical patient characteristics were made into dummy variables on the basis of the discharge record and aggregated to the hospital level with percentages (for example, the percentage of females). For continuous data (for example, age), an average value by hospital was calculated. Three dummy variables (white, black, and Latino) were created for race. A dichotomous variable was created indicating emergency versus nonemergency admission by aggregating admission type as emergency or urgent and admission source as either emergency department or transfer from another hospital emergency department. Four dummy variables were created for insurance status—Medicaid, Medicare, private insurance, and uninsured—on the basis of the primary payer type. The readmission rate was created on the basis of the percentage of patients who had more than one discharge record at the same hospital during the study period. The percentage of patients with serious mental illness was calculated as the ratio of psychiatric patients with serious mental illness over all psychiatric patients discharged from the hospital.
Level 1: organization.
Organizational characteristics included hospital type, hospital size defined as total bed count, psychiatric bed count, psychiatric discharges, staffing levels, contract status with a health maintenance organization (HMO), psychiatric occupancy rate, and daily reimbursement. Hospital type was defined as general acute care hospital or specialty psychiatric hospital. Patients discharged from state hospitals, U.S. Department of Veterans Affairs hospitals, or long-term care hospitals were excluded. All hospitals reported whether they had a formal written contract with an HMO. The psychiatric occupancy rate was the percentage of psychiatric beds used by adults with psychiatric disorders. Daily reimbursement was constructed as the total charge divided by the length of hospitalization. Full-time total staff was defined as the number of staff members working full-time at the hospital, including psychiatrists, nurses, social workers, and other professional staff. Log transformations were done for hospital bed counts, psychiatric bed counts, psychiatric discharges, daily reimbursement, and full-time hospital staff because of large variations in these variables.
Level 2: regional and county program characteristics.
Since public mental health services in Pennsylvania are funded and administered by county program authorities, we constructed variables at the level of county mental health programs to capture relevant organizational and financial characteristics as a regional construct that might be associated with psychiatric length of stay at the hospital level. Although Pennsylvania has 67 counties, there are 44 mental health administrative programs because some counties combine their program administration for efficiency. Two programs were dropped because they had no inpatient hospital with psychiatric discharges. Thus 42 mental health programs were included in the study.
Regional and county program characteristics included community mental health expenditures (dollar expenditures per 10,000 population), which represented the total amount of outpatient funds provided to the county mental health program by Medicaid and the state office of mental health in 2006; percentage of the county mental health budget used for residential care; poverty rate, which was the percentage of residents in the county who were living below the federal poverty level; and county size, which was operationalized as the total county population. Log transformations for community mental health expenditures and total population were conducted because of the large variation by county program.
Length of hospitalization
Length of hospitalization, the dependent variable, refers to the average length of psychiatric hospitalization of patients who were hospitalized at the same hospital. Log transformation for length of hospitalization was conducted to account for positive skewness.
Statistical analysis
Descriptive statistics were conducted to analyze patient, hospital, and county mental health program characteristics. To account for the multilevel structure of the data, in which hospitals (level 1) are nested within mental health program units (level 2), hierarchical linear modeling (HLM) was employed (
43).
Our analytic strategy used an unconditional model, which included a level-1 random intercept, without any independent variables. This allowed us to see the variability in hospital and program units by calculating ICCs, which represent the proportion of variance in the outcome between groups (
43). We then created conditional models by adding patient case mix characteristics, hospital characteristics, and program-level characteristics separately in different models. To identify predictors of length of hospitalization, fixed effects using the conditional models were employed. Considering the relatively small observed missing values on the patient level, listwise deletion was conducted. HLM Software 6.08 was used to conduct multilevel analyses.
Results
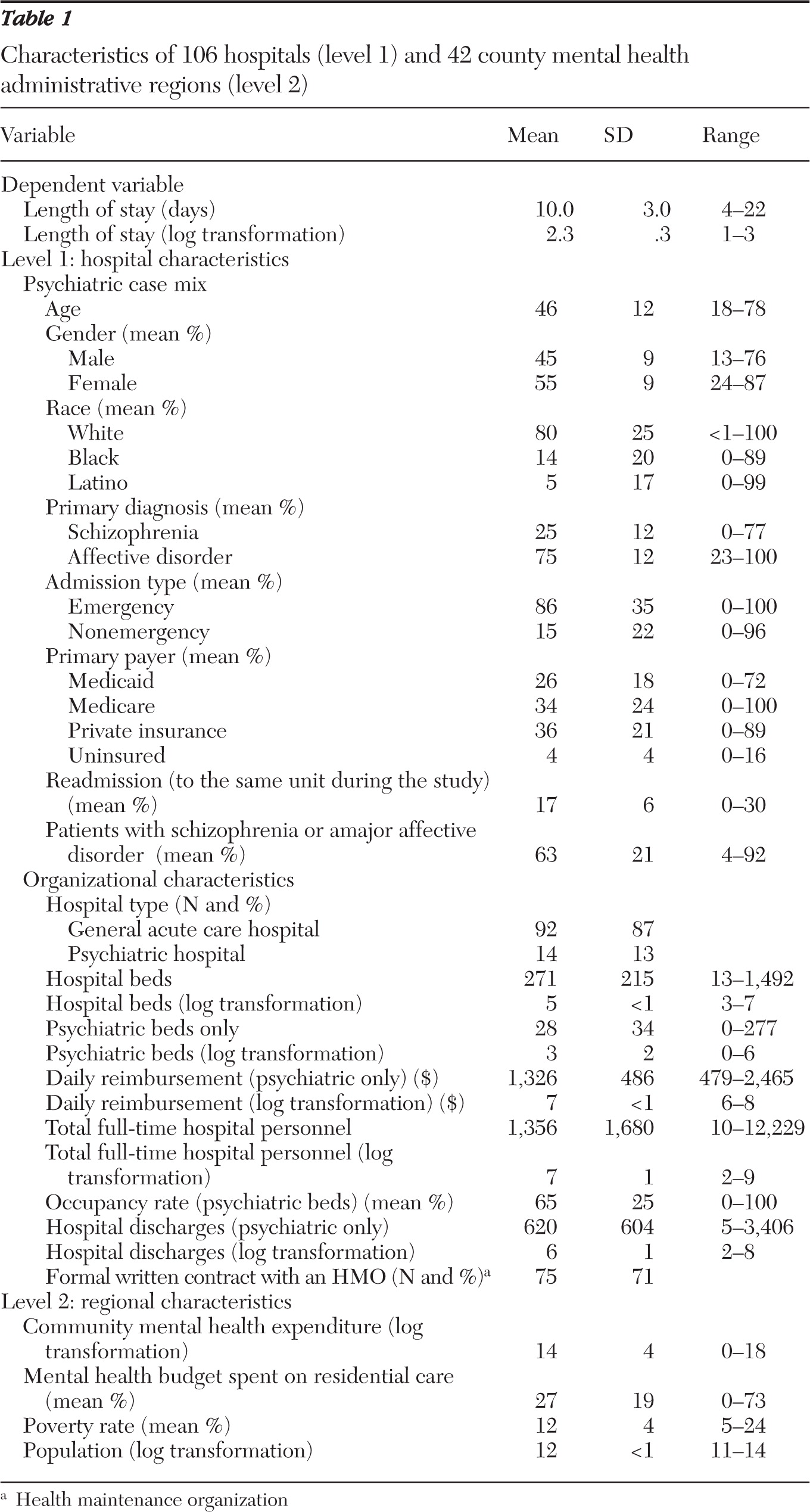
Table 1 presents hospital and county mental health program characteristics. The mean length of psychiatric hospitalization was 10.0 days. The mean age of patients was 45.5 years. The 106 hospitals reported a mean percentage of female patients of 55%. Other reported means were as follows: white patients, 80%; patients with affective disorders, 75%; and admissions through the emergency department, 86%. In terms of primary payer type, the percentage of patients with private insurance was the highest (36%), followed by Medicare (34%) and Medicaid (26%). About 17% of patients were hospitalized at the same hospital more than once during the study period.
In terms of hospital organizational characteristics, most were general acute care hospitals (87%), and most had a formal written contract with an HMO (71%). The overall psychiatric occupancy rate was 65%. In terms of regional characteristics, the percentage of the county mental health budget used for residential care was 27%, and the average percentage of persons living below the federal poverty level was 12%.
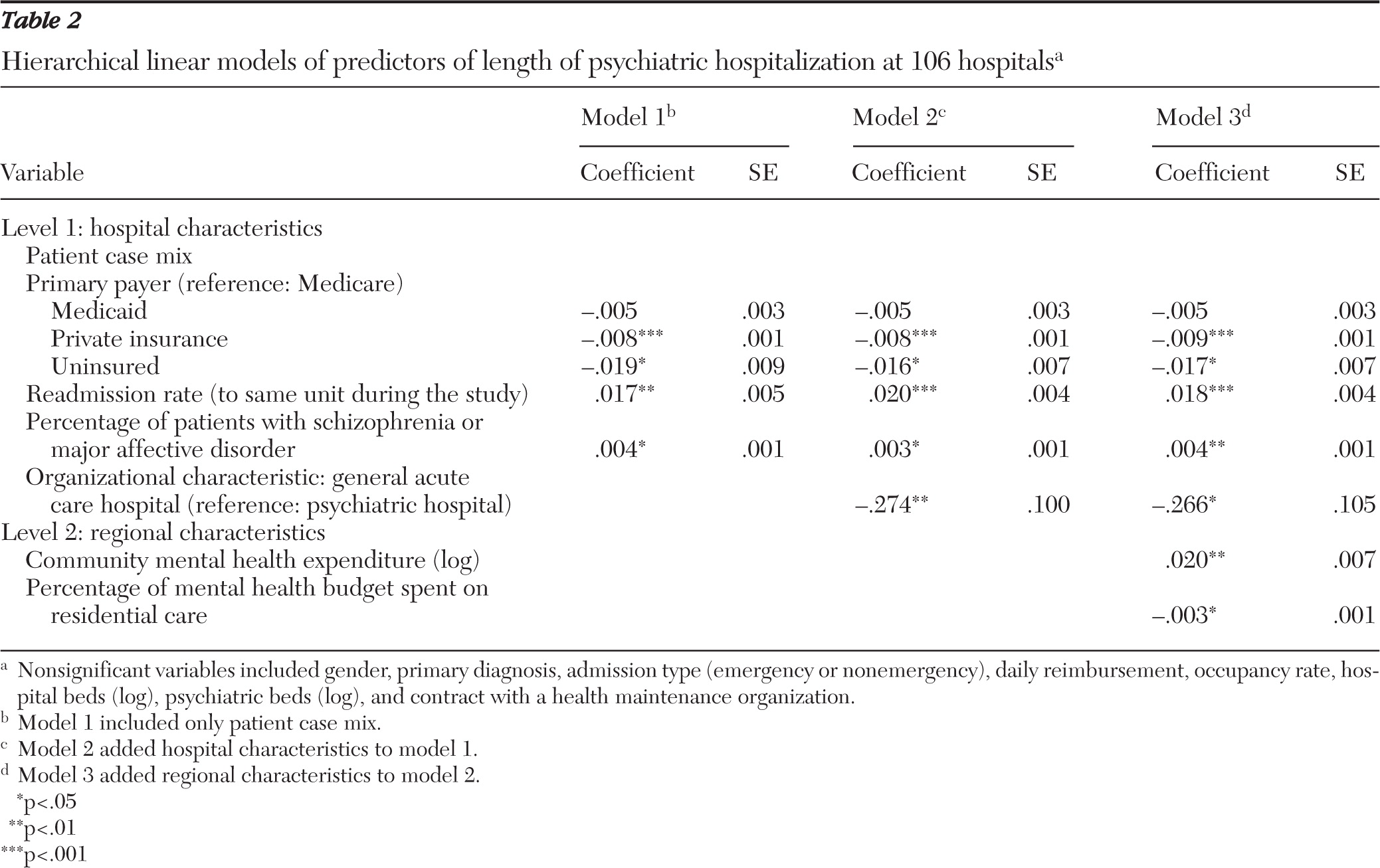
Table 2 shows predictors of length of psychiatric hospitalization from HLM models. The variables of age, race, total number of psychiatric discharges, total number of full-time personnel, and total population of the region were excluded in the model because of multicollinearity, whereas other variables that were more amenable to the policy-relevant issue of psychiatric hospitalization remained in the model. Because of the large number of variables in the study, only variables that were statistically significant predictors are presented. All random effects were statistically significant (p<.05), indicating that there was significant variability in length of hospitalization between hospitals across county mental health programs. The proportion of variance explained in length of hospitalization that was attributable to hospital characteristics was 84%, and the proportion of variance that was attributable to county mental health program characteristics was 16%.
Among hospital-level patient characteristics, insurance status, percentage of patients readmitted to the same hospital, and percentage of patients with serious mental illness were statistically significant predictors of length of stay when the analysis did not control for hospital characteristics and county mental health program characteristics (model 1). Stays were longer at hospitals with a higher percentage of Medicare patients than at hospitals with a higher percentage of patients with private insurance and uninsured patients. Stays were also longer at hospitals with a higher percentage of patients with serious mental illness as a proportion of all psychiatric discharges and at hospitals with a higher readmission rate. Regarding hospital-level organizational characteristics (model 2), stays at psychiatric hospitals were longer than stays at general acute care hospitals (p<.01).
In model 3, after the analysis controlled for hospital characteristics, stays were longer in hospitals that were located in counties where the county mental health program received a larger percentage of the state's mental health budget and where a smaller share of the budget was used for residential care. Other significant predictors found in model 2 (primary payer, type of hospital, readmission rate, and percentage of patients with serious mental illness) remained as significant predictors in model 3 with the same directions.
Discussion
Examining factors related to variation in length of hospitalization is particularly relevant for health care policy makers because the number of hospital days attributed to psychiatric conditions is greater than that attributed to any other medical disorder (
44). In our multilevel model, we found that hospital stays were longer at psychiatric hospitals, at facilities with a greater proportion of patients with serious mental illness (need factor), and at facilities with a higher percentage of reimbursement from Medicare (enabling factor). In addition, at a county level, hospital stays were longer in areas where fewer public mental health dollars were allocated to residential care as a percentage of overall mental health funding (contextual factor).
Although we found longer stays at hospitals with a larger percentage of patients with serious mental illness, we cannot conclude that the severity of symptoms is greater for inpatients with serious mental illness than for inpatients with other mental disorders. Psychiatric patients who are admitted to a hospital likely have similar levels of symptom severity in order to meet insurance criteria for admission. An alternative explanation is that patients with serious mental illness have high rates of comorbid mental and general medical conditions, which may complicate their treatment and lengthen their stay.
The finding that stays were longer at psychiatric hospitals may be associated with practice patterns that go beyond crisis stabilization. However, we cannot draw firm conclusions because the data set that we used limits our ability to determine whether the psychiatric hospitals had treatment philosophies that were different from those of the other hospitals. Before policy recommendations can be made, further investigation is required using chart reviews and specific data collection efforts focusing on practice patterns.
An unexpected finding was that hospitals with longer stays had higher rates of readmission. Previous studies on the relationship between hospital readmission and length of stay have been inconclusive, with some studies showing higher rates of readmission to be associated with shorter stays (
45–
47) and others finding no relationship (
48). Our finding may suggest that seriously ill patients with longer stays return to the hospital after discharge because a suitable placement is lacking. Further research on hospital practice patterns related to discharge planning and available residential community resources is warranted to validate this explanation.
For psychiatric hospitalizations, Medicare reimbursement rates are generally higher than Medicaid reimbursement rates or compensation for uninsured patients. Also, patients with psychiatric disorders who are Medicare enrollees are often seriously disabled (recipients of Social Security Disability Insurance), which may also explain why patients with Medicare as a funding source had longer stays than those with private insurance (
49,
50).
An important contribution of this study is our use of a multilevel statistical model to reflect the nested structure of hospitals within county mental health administrative programs. In many states, particularly Pennsylvania, which has a county-level delivery system, mental health programs are involved in allocating mental health resources and managing state dollars. Our model allowed us to examine the relationship between public mental health expenditures on outpatient and residential care and psychiatric hospitalization in a hospital other than a state hospital. Greater expenditure on community outpatient care might be expected to reduce inpatient utilization, but this was not a finding of our study. The Dartmouth Atlas project yielded a similar result: researchers found that greater supply generated greater demand for both outpatient and inpatient care (
51).
However, in examining specific resource allocations, we found shorter stays in hospitals located in regions where a larger proportion of public-sector expenditures were allocated to residential care. Although the finding has face validity, no conclusions about causality can be drawn because we do not know whether the hospitalized patients were the ones who used the residential services. A study that links hospital discharges with admission to residential facilities would be needed. Furthermore, a comprehensive picture of residential resources, including supported housing programs subsidized by federal funds, housing programs run by local religious organizations, and housing units supported by foundations and charitable organizations, is needed to establish a more accurate relationship between residential resources and length of hospitalization.
An analytic limitation in this study is the relatively small group size (for example, the average number of hospitals per county mental health program was 2.5). Recent empirical research by Clarke (
52) found that two-level models, unlike OLS models, generated unbiased estimates of the fixed effects and standard errors with one exception—a model with a very small group size (≤2). Clarke (
52) demonstrated that a multilevel model with an average of five observations per group might be more reliable. Thus further studies are recommended utilizing a multilevel model with a larger group size.
Conclusions
Using a hierarchical methodology and administrative data, this study identified significant hospital and contextual features, such as hospital type and community mental health expenditures, that were related to length of hospitalization for persons with serious mental illness. Further studies should investigate differences on hospital admission of symptom levels by diagnosis to determine whether reimbursement policies should risk-adjust for individuals with serious mental illness. Also, the extent of variation in treatment philosophy between general hospitals and specialty hospitals requires examination. Finally, the extent to which supportive and supported housing is a substitute for hospital care requires more comprehensive study.
Acknowledgments and disclosures
The authors are grateful to Aidan Altenor, Ph.D., for his help in data acquisition and Joan Erney, J.D., for her support of the study.
The authors report no competing interests.