Work is an integral component of recovery from psychiatric disorders (
1), providing financial resources as well as social support and social identity, self-esteem, and a sense of purpose (
2,
3). This study focused on how treating posttraumatic stress disorder (PTSD) affects work-related quality of life. PTSD is a serious and prevalent psychiatric disorder. Among U.S. adults, the lifetime prevalence is 6.8% (
4). Prevalence is elevated in populations with high exposure to traumatic events, such as military veterans. For example, an estimated one in seven veterans returning from the conflicts in Iraq and Afghanistan has PTSD (
5).
PTSD is associated with decrements in all domains of quality of life (
6,
7). According to the multicomponent model of quality of life (
8), work-related problems linked to PTSD can be characterized in terms of social-material conditions such as employment status, functioning, and subjective well-being and satisfaction. PTSD is associated with increased likelihood of unemployment and failure to return to work after a traumatic event (
9–
12), lower hourly wages, increased absenteeism, and difficulty with work-related demands (
13–
20). Findings about PTSD and work satisfaction are mixed. Some studies have found associations between PTSD and lower satisfaction with work (
21–
23), but others have failed to find an association (
24,
25).
Symptom reduction is the primary outcome in most clinical trials of treatment for psychiatric disorders. However, symptom reduction is also related to positive effects on work-related quality of life (
26,
27). Placebo-controlled trials have found improved occupational functioning following treatment with selective serotonin reuptake inhibitors (
28–
31). Although they are fewer in number, studies that have addressed the effect of psychotherapy for PTSD on occupational outcomes have found generally positive results (
19,
32–
34). For example, female participants in a randomized trial of prolonged exposure with or without cognitive restructuring had lower posttreatment occupational impairment relative to persons in a wait-list control group (
33).
This study examined work-related quality of life in a sample of female military veterans and soldiers who had sought treatment for PTSD. Lifetime prevalence of PTSD is higher among women than men (9.7% versus 3.6%, respectively) (
35). Among veterans who were treated in the Department of Veterans Affairs (VA) in 2011, 11.6% of women and 8.7% of men had a diagnosis of PTSD (
36). Studies have found PTSD to have comparable effects on work-related quality of life among female veterans and men (
37–
40). Analyses of the sample described in this article found that PTSD severity before treatment was associated with higher occupational impairment and lower satisfaction with employment but was not associated with employment status (
41).
The sample of women in this study were part of a randomized controlled trial comparing the effects of prolonged exposure (
42) with a present-centered treatment that controlled for nonspecific benefits of therapy (
43). The original trial found that prolonged exposure was more effective than present-centered therapy for treatment of PTSD symptoms and somewhat more effective for treatment of depression. We examined whether prolonged exposure would also lead to better work-related quality-of-life outcomes. Our secondary aim was to further understanding of the relationship between PTSD symptoms and quality of life by examining how clinically meaningful change during treatment relates to change in work-related outcomes.
Measures of individual improvement are important indicators of a treatment’s benefits, especially because average symptom change may not accurately reflect the likely change among individuals (
44). By extension, understanding how individual improvement maps onto changes in quality of life can enhance knowledge of what patients need to help them achieve recovery. Prior findings had shown that to experience improved sexual functioning, individuals must no longer meet PTSD diagnostic criteria (
45). Likewise, we expected that participants who experienced clinically significant change would also enjoy greater improvements in work-related quality of life.
We also explored whether current depression and employment status moderated the effects of treatment and of clinically meaningful change on work-related outcomes. We expected that depression could attenuate any effects of treatment or change, given findings that initial depression severity predicts change in PTSD symptoms after treatment (
46–
48). It was more difficult to make predictions about employment status. Although severity of PTSD after treatment was unrelated to employment status (
41), prior studies found that individuals with PTSD had an increased likelihood of unemployment (
9,
10). However, it seems most plausible that individuals who are able to work—even at a reduced capacity—would show the greatest benefit in work-related outcomes after receiving prolonged exposure or after experiencing a clinically meaningful reduction in PTSD symptoms.
Methods
Details about the original study have been published elsewhere (
43,
49). An institutional review board at each site approved the research protocol. Participants provided written informed consent after they had been given a complete description of the study. Data were collected between August 2002 and October 2005.
Participants
Participants were 218 women (214 veterans and four active-duty soldiers) drawn from a randomized clinical trial of PTSD treatment (
43). Inclusion criteria were current PTSD according to the “one, two” rule (frequency greater than or equal to once or twice in the past month and moderate or greater intensity) and a score of ≥45 on the Clinician-Administered PTSD Scale (CAPS) (
50); a gap of three or more months since experiencing trauma; a clear memory of the trauma that caused PTSD; an agreement to not receive other psychotherapy for PTSD during study treatment; and for those on psychoactive medication, a stable medication regimen for the prior two months. Exclusion criteria were current psychotic symptoms, mania, or bipolar disorder; current substance dependence; prominent current suicidal or homicidal ideation; cognitive impairment; current involvement in a violent relationship; and self-mutilation within the past six months.
Because work-related quality of life was the outcome of interest, retired members (N=31) of the original sample of 284 participants were excluded. On average, the retired participants were 11.50 years older than the working or unemployed participants (t=6.91, df=282, p<.001), but the two groups did not differ on PTSD symptoms, occupational impairment, or occupational satisfaction before treatment. We excluded an additional 35 women who did not participate in any posttreatment assessments. Their pretreatment PTSD symptoms, occupational impairment, or occupational satisfaction did not differ from participants who partook in posttreatment assessment.
Measures
We measured PTSD symptoms by using the CAPS (
50), a structured interview that rates the frequency and intensity of the 17
DSM-IV PTSD symptoms (
51) on a 5-point scale. Total scores range from 0 to 136, with scores of 60 to 80 indicating severe PTSD (
50). Current depression diagnosis was measured by using the Structured Clinical Interview for DSM-IV (SCID) (
52). Interrater reliability was high for both interview measures (
43).
Clinicians rated occupational impairment with the CAPS on a 5-point scale ranging from 0, none, to 4, extreme. Interrater reliability was high (intraclass correlation coefficient=81). Self-rated impairment was measured by an item from the Beck Depression Inventory (
53). Possible scores range from 0, “I can work about as well as before,” to 3, “I can’t do any work at all.” Occupational satisfaction was assessed by the work satisfaction item in the Quality of Life Inventory (QOLI) (
54). Possible scores on the 6-point scale range from –3, very dissatisfied, to 3, very satisfied, and the scale has no midpoint. The QOLI instructs unemployed individuals to rate how satisfied they feel about not working. Employment at study entry was coded as 1, full- or part-time, or 0, unemployed or other.
Procedures
Information about potential participants was provided to study staff by referring clinicians. Study staff met with potential participants to explain the study and obtain informed consent. A master’s- or doctoral-level clinician who was blind to the participants’ treatment assignment performed assessments at study entry, after completion of treatment, and at three- and six-month follow-ups.
Eligible women were assigned at random to receive ten weekly sessions of prolonged exposure (
42) or present-centered therapy (
49). Therapists were 52 female master’s- or doctoral-level clinicians who were assigned at random to deliver one of the two treatments. All received specialized training in the assigned treatment. Sessions were videotaped and reviewed by an expert supervisor, who provided telephone supervision. Therapist adherence and competence, rated by an independent fidelity monitor, were excellent and equivalent across treatments (
43).
Data analysis
Data from participants who provided at least one outcome assessment, including those who discontinued treatment, were analyzed with SAS PROC MIXED to account for missing data and clustering of participants within therapists. For each outcome, the analysis consisted of a longitudinal model that included the baseline score, group (treatment type and loss of or continued PTSD diagnosis), site, time of assessment, and the group × time interaction. The models that examined loss of diagnosis included treatment type as a fixed effect. Therapist nested within treatment was included as a random cluster effect in all models. The Kenward-Roger approximation was used to estimate the denominator degrees of freedom (
55,
56). Pre- to posttreatment effect sizes were computed as Cohen’s d, or the standardized mean difference (
57).
We tested additional models to determine whether the effect of treatment type or loss of diagnosis was moderated by current major depression or work status before treatment. Interactions between current major depression and current work status with treatment type or loss-of-diagnosis group were tested separately for each outcome. We also explored whether including a dichotomous indicator (yes or no) of service-connected disability status resulting from PTSD and removing the four active-duty soldiers affected the results. Because neither analysis changed any of the findings, the results do not include service-connected disability status as a covariate and are based on the entire sample of 218 women.
Results
The characteristics of the sample are summarized in
Table 1. On average, participants were in their mid-forties (range 22–66 years). Almost all had postsecondary education, one-third were married or cohabitating, and just less than half were members of a nonwhite minority group or were currently employed. About half of participants had a service-connected disability approved by the VA. Participants had experienced multiple types of traumatic events. Sexual trauma was most frequent, and over 70% (N=156) reported experiencing at least one sexual trauma during military service. One-quarter of participants had experienced exposure to a war zone. Almost 80% had a current comorbid axis I disorder; about half had major depression.
Before treatment, the average score for PTSD symptoms was in the severe range. Clinician ratings of occupational impairment fell between moderate and severe; almost 50% (N=107) of participants had severe or extreme impairment. About 88% (N=191) of participants reported some degree of occupational impairment. About half of participants expressed some degree of occupational dissatisfaction (51%, N=110).
Effects of treatment
Pre-post effect sizes are shown in
Table 2. There were small, statistically significant reductions in both measures of occupational impairment in both treatment groups. The effect sizes of the two treatments did not differ for either outcome. For occupational satisfaction, no significant changes were found in pre-post effect sizes for treatment type or for differences between treatments.
Least-squares means for each work outcome in the longitudinal analyses are also presented in
Table 2. There was no effect of treatment type on any of the work outcomes, nor were there any interactions with time. There was an effect of time on self-rated impairment (F=5.88, df=2 and 397, p=003). Post hoc comparisons showed that from posttreatment to three-month follow-up, impairment increased (t=–3.43, df=384, p<.001), but it did not change further between three and six months.
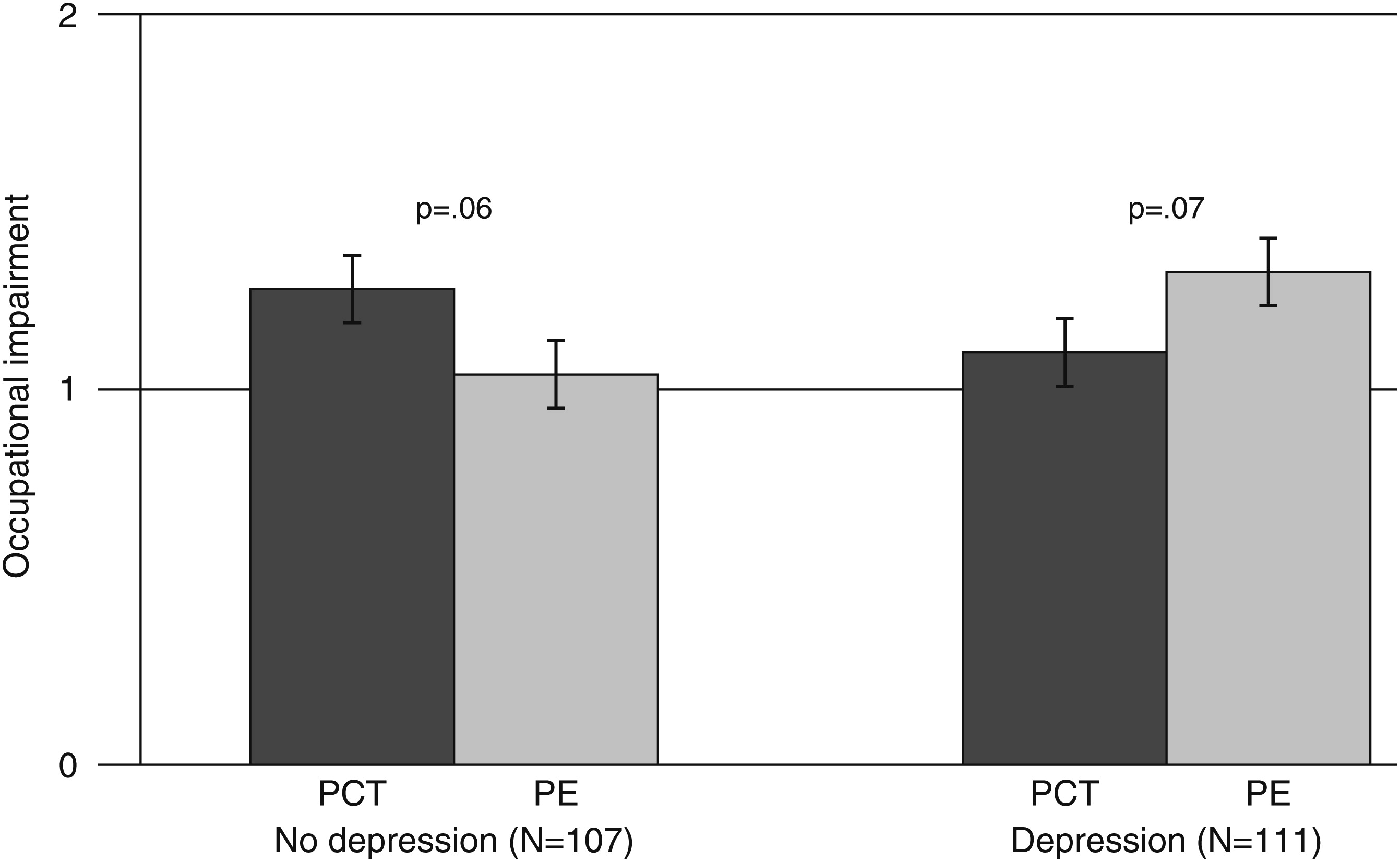
We examined whether current depression and pretreatment work status moderated the effect of treatment. There was an interaction between depression and treatment type for self-rated occupational impairment (F=7.32, df=1 and 212, p=007). Examination of the least-squares means of self-rated occupational impairment by treatment type and depression diagnosis (
Figure 1) suggested that prolonged exposure was more effective in reducing impairment among participants without current depression and that present-centered therapy was more effective in reducing impairment among participants who were depressed. However, the simple effect of treatment type was not statistically significant in either group.
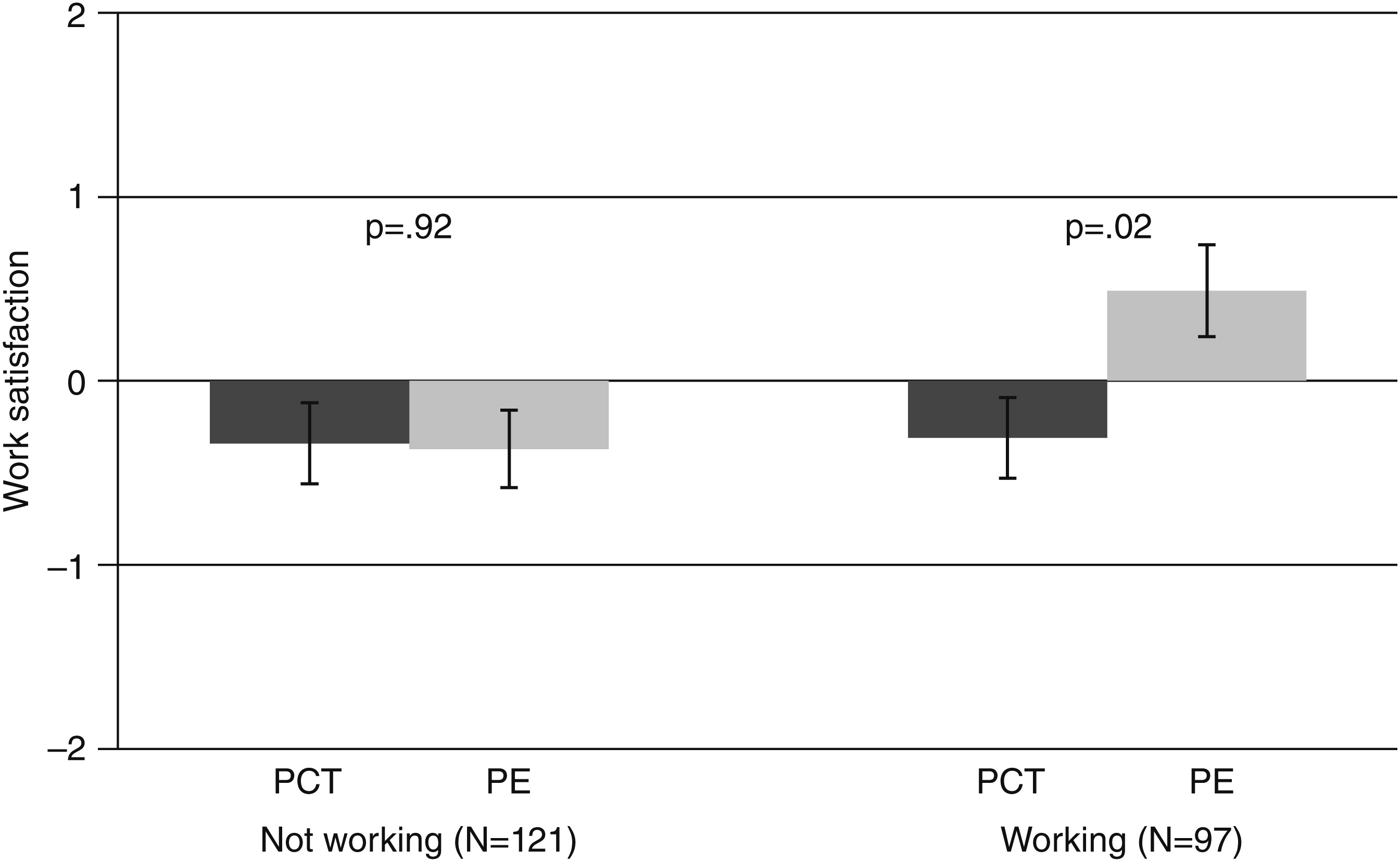
There also was an interaction between work status and treatment type related to work satisfaction (F=4.72, df=1 and 220, p=03) (
Figure 2). Prolonged exposure was more effective than present-centered therapy among employed participants (t=–2.59, df=74.3, p=012) but not among the unemployed.
Effects of loss of diagnosis
Immediately following treatment, 60 participants (29%) no longer met diagnostic criteria for PTSD. (Ten participants were missing at least one posttreatment assessment.) For those who lost their PTSD diagnosis, CAPS scores declined by an average of 45.90 points (range 14–80). Clinician-rated and self-rated impairment improved only among participants who lost their diagnosis (
Table 3). Pre-post effect sizes for clinician-rated and self-rated impairment in this group were large and were significantly greater than pre-post effect sizes among participants who still had PTSD (t=4.94, df=194, p<.001 and t=6.93, df=193, p<.001, respectively). There was no pre-post change in the occupational satisfaction of either group, and the groups did not differ in the degree of pre-post change.
However, in the longitudinal analyses, participants who no longer had PTSD at the end of treatment had greater improvements on all three outcomes compared with those who still met diagnostic criteria. There was a significant effect of loss of diagnosis on clinician-rated impairment (F=50.40, df=1 and 201, p<.001), self-rated impairment (F=35.97, df=1 and 214, p<.001), and occupational satisfaction (F=14.92, df=1 and 211, p<.001). For self-rated impairment, there was a significant time effect (F=9.07, df=2 and 394, p<.001). Self-rated impairment was lower at posttreatment follow-up than at three-month follow-up (t=–4.19, df=375, p<.001) but was not different at the three- and six-month follow-ups. There was an interaction between loss of diagnosis and time of assessment for clinician-rated impairment (F=9.01, df=2 and 384, p<.001) and self-rated impairment (F=4.48, df=2 and 394, p=012). Although the loss-of-diagnosis group had significantly lower impairment at all three follow-ups, the size of the effect decreased over time. Neither work status nor current depression moderated the effect of loss of diagnosis on any outcome.
Discussion
We performed secondary analyses of data from a randomized clinical trial of prolonged-exposure therapy to investigate whether treatment for PTSD also improves work-related quality of life. During the course of treatment, clinician ratings and self-ratings of occupational impairment improved, but there was no change in occupational satisfaction. However, the effects of prolonged exposure and present-centered therapy on work-related outcomes did not differ, even though prolonged exposure led to greater improvements in PTSD symptoms in the original trial (
43). These findings are inconsistent with results of other studies showing that treatment for depression (
26,
27) and for PTSD (
19,
28) was associated with improved work-related quality of life.
There are several possible explanations for the difference between the findings for PTSD symptoms and for work-related quality of life. First, before treatment, all participants had substantial PTSD symptoms but not necessarily reduced work-related quality of life; the effects of PTSD treatment on work outcomes may be more difficult to detect among individuals with varying degrees of work-related problems. Second, statistical power to detect treatment differences may have been reduced because we excluded retired participants.
Another explanation of why prolonged exposure did not have an impact on work-related quality of life is that the modest, although statistically significant, improvements in PTSD symptoms that were observed in the original trial (
43) were not large enough. Symptom reduction may have an effect on work-related quality of life only when an individual has experienced a clinically meaningful amount of improvement. This hypothesis is supported by the association between no longer meeting diagnostic criteria for PTSD after treatment and large improvements in clinician-rated and self-rated occupational impairment. This finding is consistent with prior findings about this sample that associated loss of diagnosis, but not treatment, with improvement in sexual functioning (
45).
Nevertheless, our results suggest that even meaningful symptom improvement did not completely restore work-related quality of life. In the group that no longer met PTSD diagnostic criteria, there was at least mild to moderate occupational impairment, and occupational satisfaction was rated only slightly positive. Our findings are comparable to the results of studies showing that although treatment for psychiatric disorders is associated with improved occupational outcomes (
58–
60), patients continue to experience some degree of impairment compared with individuals without a history of a psychiatric disorder (
61,
62). Our findings also raise questions about the durability of the effects on symptom improvement on work-related quality of life. Compared with participants who still had PTSD, those who no longer met diagnostic criteria after treatment had less clinician-rated and self-rated work-related impairment at all follow-ups, but the effect declined over time.
We found that despite the absence of overall treatment effects, depression moderated the effect of treatment on self-rated impairment. There was a trend for prolonged exposure to be more effective than present-centered therapy among participants who were not depressed before treatment and a trend for present-centered therapy to be more effective than prolonged exposure among those who were depressed. We are unaware of either a theory or prior findings that explain this response pattern. Furthermore, depression did not predict differences in treatment response by this sample (unpublished data, Foa EB, Powers MB, Gillihan SJ, et al, 2011) nor in a study that examined predictors of response to prolonged exposure and cognitive processing therapy (
48). Our findings require replication to determine whether the marginally significant findings are more than statistical artifact.
We also found that employment status moderated the effect of treatment on occupational satisfaction. For employed participants, prolonged exposure was more effective than present-centered therapy, but the effect of treatment did not differ among those who were unemployed. Improvement in PTSD may lead to improved occupational satisfaction only if a person is working. By extension, reemployment may be necessary to make gains in occupational satisfaction following treatment. It is plausible that reemployment could enhance the effects of symptom improvement on occupational functioning as well.
Although women who no longer met diagnostic criteria for PTSD had greater improvement on all outcomes, there was no pre-post change in occupational satisfaction for the groups with and without PTSD. However, at all follow-up intervals, the groups differed, and women who no longer had PTSD reported higher satisfaction. An intervention to enhance job satisfaction may be required to achieve more meaningful gains (
63). Also, if PTSD has impaired an individual’s ability to be employed in an appropriate job, a change of job may be required to increase satisfaction substantially. Future research should employ multidimensional measures of work satisfaction to assess whether different components of job-related satisfaction may change as symptoms improve.
It is important to consider when interpreting our findings that the original study was not designed to specifically assess the effect of treatment on work-related quality of life. We did not have longitudinal assessments of key variables such as employment status and had only single-item measures of self-reported impairment and satisfaction. Research on this topic should be conducted with a fuller assessment battery that is repeated over time. The use of measures such as the Work Limitations Questionnaire (
64) would allow examination of how different domains of work-related quality of life, for example, mental or time management demands, change over time as a function of treatment. The effect of disability compensation and demographic factors such as gender, race, and socioeconomic status should be explored more fully as well.
Because the sample consisted almost entirely of female veterans with severe PTSD, our findings may not generalize to women who are on active duty, who are not veterans, or who have less severe PTSD symptoms. Given that the effects of employment on quality of life for men and women may differ, our findings also may not generalize to male veterans or to men in general (
65,
66). Furthermore, the heterogeneity of trauma types, coupled with the multiple types of exposure, prevented us from performing analyses to determine whether the effects would vary as a function of trauma exposure.
Conclusions
Although our study was exploratory, an important implication of the results is that the burden of PTSD can be reduced—even for patients with severe and chronic PTSD. Meaningful improvement in PTSD following psychotherapeutic treatment can translate into improved work-related quality of life. However, research studies typically employ treatment protocols that constrain the number of sessions in an attempt to standardize treatment delivery. A consequence of such methodological rigor is that some participants may not achieve or sustain the gains that might be possible with more treatment. The benefits for occupational impairment associated with loss of diagnosis of PTSD suggest that it may be necessary for treatment to continue until clinically meaningful change has been attained. However, this hypothesis should be tested in studies explicitly designed to determine how to optimally enhance quality-of-life outcomes.
Acknowledgments and disclosures
This study was conducted with grant CSP 494 from the VA Cooperative Studies Program with support from the U.S. Department of Defense (DOD). The views expressed in this article are those of the authors and do not necessarily represent the views of the VA, the DOD, or any federal agency.
The authors report no competing interests.