Suicide ranks tenth among causes of death in the United States, accounting for 38,000 deaths in 2010 (
1). Nonfatal suicide attempts cause approximately 600,000 emergency department visits (
2) and 200,000 hospitalizations (
3) annually. Early intervention to reduce this morbidity and mortality would require both accurate screening tests and effective interventions for persons found to be at risk of suicide. Although some behavioral interventions have shown promise for preventing suicidal behavior among high-risk patients (
4,
5), we have no evidence that any screening test accurately identifies people in the general population at risk of suicide attempt or suicide death (
6,
7). Consequently, the U.S. Preventive Services Task Force (
6) and others (
8,
9) do not recommend screening for risk of suicidal behavior.
Nevertheless, increasing use of standard depression outcome questionnaires (
10–
14) means that clinicians treating depression will frequently encounter patients who report thoughts of death or self-harm. For example, up to 10% of outpatients completing the nine-item Patient Health Questionnaire (PHQ-9) for depression respond to item 9—“thoughts that you would be better off dead, or of hurting yourself in some way”—with a frequency of “more than half the days” or “nearly every day” (
14,
15). At this time, we cannot offer clinicians any clear guidance regarding immediate or long-term risk for those patients. Cross-sectional research has demonstrated that reporting thoughts of death or self-harm on self-report depression questionnaires agrees with clinician assessments of suicidal ideation (
16). Longitudinal research has found that more detailed assessments that focus on suicide risk can predict subsequent suicidal behavior (
17,
18), but no previous research has examined whether item 9 of the PHQ-9 (or any other brief depression outcome questionnaire) predicts subsequent suicide attempt or suicide death.
This study used electronic medical records data from a large integrated health care system to address three questions of practical interest to clinicians: Among outpatients receiving depression treatment, do responses to item 9 accurately identify people at risk of subsequent suicide attempt or death? Does response to item 9 add information after accounting for overall severity of depression and other risk factors? What is the immediate risk of suicide attempt and suicide death among outpatients endorsing item 9 of the PHQ-9?
Methods
The Group Health Cooperative is an integrated health care system serving approximately 650,000 members in Washington State and Idaho. Group Health provides care through an internal group practice and a network of external providers available on contract. Members are enrolled through employer-sponsored insurance, individual insurance plans, Medicare, Medicaid, and other subsidized low-income insurance programs. The Group Health Human Subjects Review Committee served as the institutional review board for this study and granted a waiver of consent for use of deidentified records data for this research.
Since March 2006, all group practice primary care and mental health providers have been advised to administer the PHQ-9 depression questionnaire (
19–
22) at every visit for depression treatment. Item 9 of the questionnaire asks, “Over the last two weeks, how often have you been bothered by thoughts that you would be better off dead, or of hurting yourself in some way?” with response options of “not at all,” “several days,” “more than half the days,” or “nearly every day.” The study sample included all PHQ-9s collected between January 1, 2007, and December 31, 2011, for patients ages 13 or older. The proportion of all visits with depression diagnoses for which a PHQ-9 score was recorded increased from 5% in 2007 to 48% in 2011.
Suicide attempts were identified in electronic medical records (for services provided at Group Health Cooperative facilities) and insurance claims (for services provided by external providers or facilities). Three criteria were used to identify nonfatal suicide attempts: inpatient or outpatient encounter involving ICD-9-CM diagnosis of definite self-inflicted injury (E950–E958), inpatient or outpatient encounter involving ICD-9-CM diagnosis of acute injury considered possibly self-inflicted (E980–E988), and inpatient or outpatient encounter with ICD-9-CM diagnosis of suicidal ideation (V62.84) accompanied by ICD-9-CM diagnosis of either poisoning (960–989) or open wound (870–897).
We previously reported (
23) that validation by clinician review of full-text medical records notes found a positive predictive value of 100% for the first criterion and 80% for the second (compared with definite documentation of both self-inflicted injury and suicidal intent). Review of an additional 100 records to validate the third criterion found a positive predictive value of 86%. Given the relative frequency of these three criteria in our sample (61% definite self-inflicted injury, 31% possible self-inflicted injury, and 8% injury or poisoning plus suicidal ideation), we estimate the weighted-average positive predictive value to be 92% for all three combined. To evaluate possible undercoding of self-inflicted injury, we examined the proportion of emergency department and hospital encounters with any injury or poisoning diagnosis for which any cause-of-injury code (or E code) was not recorded. The proportion with no such code is one indicator of the proportion of medically treated suicide attempts that might be missed by reliance on E codes for identification (
24). The proportion of injury or poisoning encounters with no E code was 29% in 2010.
Suicide deaths were identified by linking membership records to state death certificate and identifying records with ICD-10-CM cause-of-death codes indicating definite self-inflicted injury (X60–X84) or possible self-inflicted injury (Y10–Y34).
Electronic medical records and claims for identification of nonfatal suicide attempts were available through December 31, 2011. Death certificate data were available through December 31, 2010. Electronic medical records and claims data were also used to assess past use of specialty mental health care and past psychiatric hospitalization.
Descriptive analyses examined the cumulative risk of any suicide attempt (fatal or nonfatal) and cumulative risk of suicide death according to response to item 9 of the PHQ-9. Analyses treated the questionnaires as the unit of analysis, so that each completed questionnaire defined a new period at risk. Each risk period was censored at the time of disenrollment from Group Health, death from causes other than suicide, or the end of the study period. In the primary analysis, time at risk was not censored at the next PHQ-9 completion. Consequently, each patient could contribute multiple overlapping risk periods, and each suicide attempt or death could be linked to multiple prior PHQ-9s from a single patient. This approach examines risk on the basis of what was known at the time of completion of the PHQ-9, regardless of subsequent assessment or treatment. It avoids informative censoring that would occur if likelihood of completing a later PHQ-9 was related to probability of observing a subsequent suicide attempt. Alternative analyses with censoring at the time of next PHQ-9 completion yielded substantially similar findings.
Partly conditional Cox proportional hazards regression was used to estimate the association between response to item 9 and risk of subsequent suicide attempt or death after accounting for other risk factors (age, sex, history of prior hospitalization or mental health specialty treatment, and response to other PHQ-9 items) (
25). These models accounted for clustering of observations per person, with standard errors estimated with the robust sandwich estimator for survival data (
26). We assessed proportional hazards assumptions examining slopes of scaled Schoenfeld residuals plotted over time and by examining standard diagnostic plots (
27).
Results
Electronic medical records contained 207,265 completed PHQ-9s for 84,418 patients, including 42,333 patients (50%) with a single questionnaire, 17,251 (20%) with two, 9,295 (11%) with three, 5,373 (6%) with four, and 10,166 (13%) with five or more. Encounters in which questionnaires were administered included 92,440 (45%) with specialty mental health providers, 112,954 (54%) with primary care providers, 1,274 (1%) with other medical or surgical specialists, and 597 (<1%) emergency department visits. Ninety-one percent (N=188,611) of patients were receiving current or recent mental health treatment (as indicated by mental health diagnosis, prescription for antidepressant medication, or use of mental health specialty care) at the time of completing the PHQ-9. With the conventional classification of PHQ-9 scores, depression was minimal (score 0–4) in 43,210 (21%) cases, mild (score 5–9) in 52,214 (25%) cases, moderate (score 10–14) in 47,261 (23%) cases, moderately severe (score 15–19) in 37,565 (18%) cases, and severe (score ≥20) in 27,015 (13%) cases. Response to item 9 regarding thoughts of death or self-harm was “not at all” in 159,234 (77%) cases, “several days” in 29,910 (14%) cases, “more than half the days” in 10,864 (5%) cases, and “nearly every day” in 7,257 (4%) cases.
The number of days of follow-up after completion of the PHQ-9 (that is, before censoring or suicide attempt) ranged from 1 to 1,703 (median=360, mean=477). Follow-up was censored because of death not due to suicide for 1,214 observations (1%), because of disenrollment from the health plan for 47,620 (23%), and because of the end of the study period for 158,431 (76%).
Death certificate data identified 46 suicide deaths, including 45 attributed to definite self-inflicted injury (death certificate diagnosis X60–X84) and one attributed to possible self-inflicted injury (Y10–Y34).
Electronic medical records and insurance claims data identified 709 instances of nonfatal suicide attempt. These included 470 diagnoses of definite self-inflicted injury (E950–E958), an additional 198 diagnoses of possible self-inflicted injury (E980–E988), and an additional 41 identified by the combination of a poisoning or wound diagnosis linked to a diagnosis of suicidal ideation (V62.84). These suicide attempts included 371 that led to hospitalization and an additional 338 that resulted in only emergency or outpatient treatment. Each individual could have more than one nonfatal suicide attempt in the study period; 37 patients had two attempts, nine patients had three, and three had four or five.
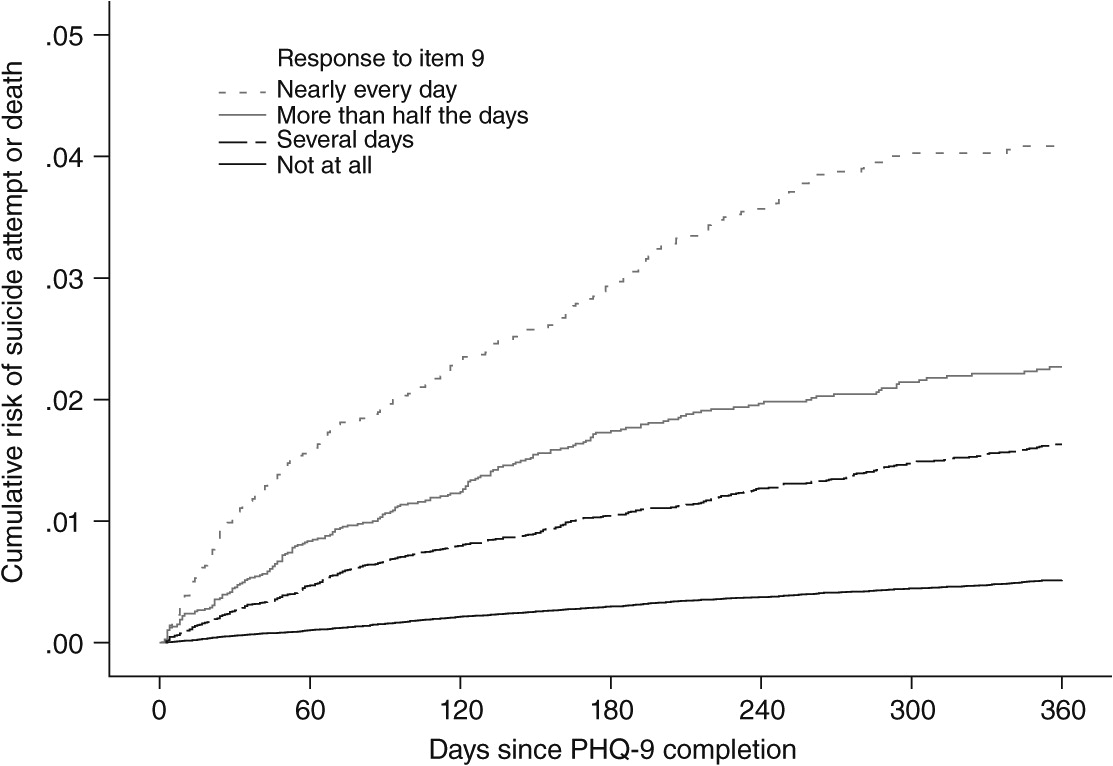
The cumulative probability of any suicide attempt (both nonfatal and fatal attempts) according to response to item 9 of the PHQ-9 is shown in
Figure 1. At one year, cumulative probability ranged from approximately .4% (1 in 250) for those responding “not at all” to approximately 4% (1 in 25) for those responding “nearly every day.” This pattern was consistent across subgroups defined by sex, age, type of visit where the questionnaire was completed, current use of antidepressant medication, or year the questionnaire was completed. [Results are available online in a
data supplement to this article.]
Results from Cox proportional hazards models predicting risk of any suicide attempt are shown in
Table 1. Without considering other risk factors (model 1), the relative hazard of any suicide attempt increased according to response to item 9 of PHQ-9, with a hazard ratio (HR) of approximately 6.4 for those responding “nearly every day” compared with “not at all.” A post hoc test for trend found a statistically significant (p<.001) linear relationship between item 9 score and risk of subsequent suicide attempt, with a 91% increase in risk (HR=1.91, 95% confidence interval [CI]=1.79–2.04) for each one-step increase in reported frequency of thoughts of death or self-harm. Risk of any suicide attempt was associated with younger age, history of specialty mental health treatment, and history of psychiatric hospitalization (model 2a). Overall depression severity (as measured by PHQ-9 items 1 through 8) was a significant predictor after accounting for demographic characteristics and treatment history (model 2b). After adjustment for all of these other risk factors, response to item 9 remained a strong predictor of any suicide attempt (model 2c).
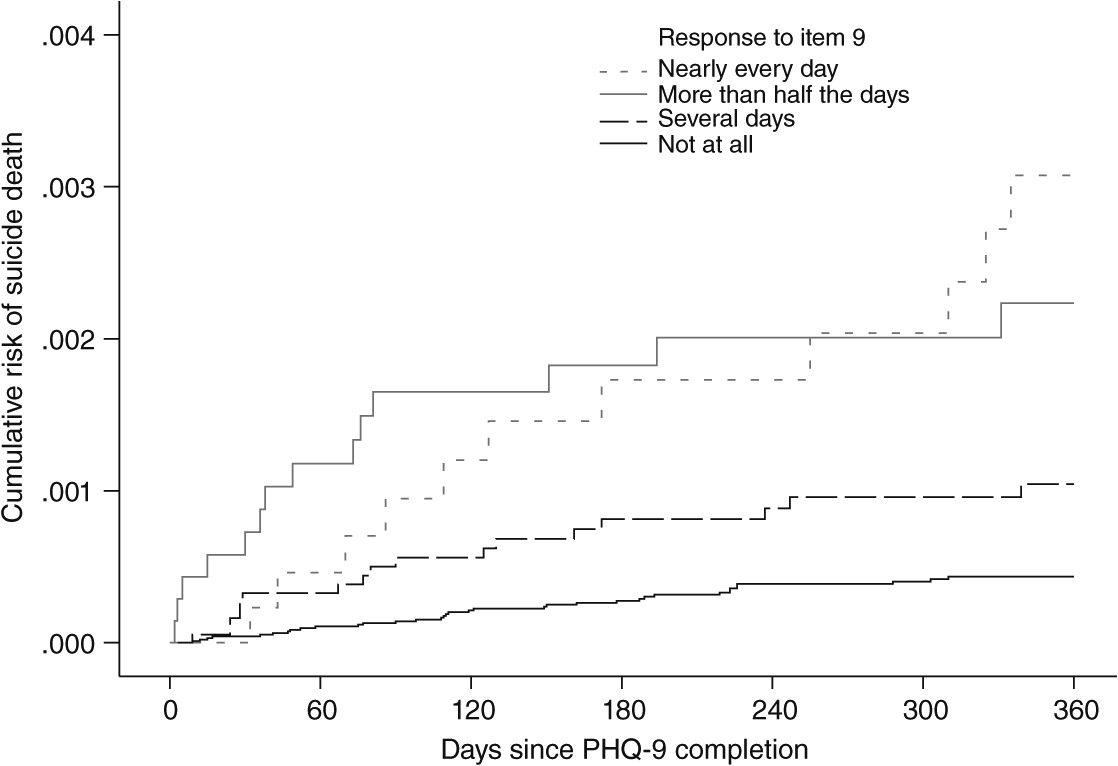
The cumulative probability of suicide death according to response to item 9 of the PHQ-9 is shown in
Figure 2. At one year, the cumulative probability of death from suicide ranged from approximately .03% (1 in 3,000) for those responding “not at all” to approximately .3% (1 in 300) for those responding “nearly every day.”
Results from Cox proportional hazards models predicting suicide death are shown in
Table 2. Without considering other risk factors (model 1), we found that the relative hazard of suicide death was significantly increased with any reported thoughts of self-harm compared with those responding “not at all.” Wide confidence limits for HRs reflect the small numbers of suicide deaths. A post hoc test for trend found a statistically significant (p<.001) linear relationship between item 9 score and risk of subsequent suicide death, with a 92% increase in risk (HR=1.92, CI=1.53–2.41) for each one-step increase in reported frequency of suicidal thoughts. Risk of suicide death was significantly higher among men. Older age, history of specialty mental health care, and history of psychiatric hospitalization were also associated with increased risk of suicide death, but these associations were not statistically significant (model 2a). After adjustment for demographic characteristics and treatment history, overall depression severity was significantly associated with increased risk of suicide death (model 2b). After accounting for all of these other predictors, response overall to item 9 remained a statistically significant predictor of suicide death (model 2c).
Table 3 displays the numbers of suicide attempts and suicide deaths during the first day, first seven days, and first 30 days after administration of the PHQ-9 according to response to item 9. The data regarding early suicide attempts (within 30 days of final PHQ-9 response) illustrate that absolute risk of attempt was low even for outpatients reporting thoughts of death or self-harm and that approximately one-quarter of suicide attempts (N=107 of 391) made soon after assessment occurred among patients responding “not at all” to item 9. The data regarding early suicide deaths also showed a low absolute risk immediately after assessment, but numbers were too small to draw conclusions regarding relationship to PHQ-9 responses.
As an additional measure of the sensitivity of item 9, each patient in the sample was classified according to her or his highest response to item 9 across all completions of the PHQ-9. Of 84,418 patients, 59,425 (70%) responded “not at all” to item 9 on every occasion. This group accounted for 144 (22%) of the 644 suicide attempts and nine (20%) of the 46 suicide attempts during the follow-up period.
Discussion
Among outpatients completing PHQ-9 depression questionnaires, response to item 9 regarding “thoughts that you would be better off dead, or of hurting yourself in some way” was a strong predictor of suicide attempt and suicide death over the following year. The 13% of patients who reported thoughts of death or self-harm “more than half the days” or “nearly every day” accounted for 53% of suicide attempts and 54% of suicide deaths (
Table 3). Even though the age and sex patterns for suicide attempts differed markedly from those for suicide death, response to PHQ item 9 predicted both outcomes. Among those reporting frequent thoughts of death or self-harm, immediate risk of suicidal behavior was low, but increased risk emerged over several days and persisted for several months.
Our findings apply to PHQ-9 depression questionnaires completed during depression treatment visits to primary care or mental health specialty providers. Our sample of questionnaires from emergency department visits was too small to specifically evaluate risk in that setting. We cannot determine whether our findings would generalize to nonclinical settings such as community screening.
The PHQ-9 was designed to measure depression severity rather than identify risk of suicidal behavior. The wording of item 9 regarding “thoughts that you would be better off dead, or of hurting yourself in some way” may falsely include some patients who are not experiencing actual suicidal ideation (
28) and falsely exclude others who are. A measure specifically focused on suicidal ideation might predict risk more accurately. This report, however, intends to provide practical guidance regarding a measure that is widely and increasingly used in everyday practice.
We should acknowledge potential misclassification of suicide attempts in both directions. Regarding false negatives, death certificate data may miss 10% to 25% of all suicide deaths (
29–
32). Given that approximately 30% of emergency department visits and hospitalizations with injury or poisoning diagnoses were not assigned a cause-of-injury code, our method for identifying nonfatal suicide attempts could miss 30% of emergency visits or hospitalizations for self-inflicted injury. In regard to false positives, review of full-text records for a sample of cases (described above) did not confirm suicide attempt in approximately 7% of cases identified with visit or hospital diagnosis data. Either type of misclassification might bias the associations we report if either error was related to prior PHQ-9 responses or to other risk factors. Random or nonspecific misclassification would lead to a conservative bias (reducing measures of association).
Denying thoughts of death or self-harm ideation on the PHQ-9 certainly does not rule out risk of subsequent suicide attempt. As shown in
Table 3, approximately one-fourth of suicide attempts that occurred within one week of patients’ completing a PHQ were by patients responding “not at all” to PHQ item 9. We could not determine whether these unexpected suicide attempts reflect imperfect sensitivity of item 9, patients’ reluctance to reveal thought of death or self-harm, or the sudden appearance of those thoughts between completion of the PHQ-9 and suicide attempt. No data were available regarding changes in suicidal ideation among patients treated in community practice or how such changes were related to suicidal behavior. Given the significant proportion of suicide attempts among patients recently denying thoughts of death or self-harm, this is a priority area for future research.
Treating clinicians were aware of PHQ-9 results, and the risks we observed reflect the consequences of any clinical response to PHQ-9 responses. While we could not directly measure how clinicians responded to the PHQ-9, we expect that clinicians typically attempted to assess immediate risk and initiate referrals, intensification of treatment, or even hospitalization. The elevated risk associated with response to PHQ item 9 was observed in spite of any such clinical responses. But providers’ immediate interventions may explain why the absolute risk in the first days after PHQ-9 completion was low, even among patients reporting frequent thoughts of death or self-harm.
If a widely used depression outcome questionnaire identifies risk of suicide attempt, this creates an opportunity for intervention and a potential liability. Concerns regarding liability led to the development of an eight-item PHQ for depression, with item 9 of PHQ-9 omitted to avoid probing for thoughts of death or self-harm (
33–
35). This reduced questionnaire is intended for use in settings where an immediate clinical response is not feasible. But use of the full questionnaire in those settings might identify a large number of people at risk of suicide attempt who would otherwise go undetected. Concerns regarding liability should not close off a potential avenue for prevention.
Although our findings showed that item 9 of the PHQ-9 accurately identifies outpatients at increased risk of suicidal behavior, this finding alone is not sufficient to justify population-based screening for secondary or selective prevention. Justification for population-based screening and prevention would require both evidence that screening predicts risk in the general population and evidence that some feasible intervention can reduce that risk (
6,
8). Some specific behavioral treatments (
4,
5) and outreach interventions (
36–
39) have been shown to reduce risk of suicidal behavior in high-risk groups, such as survivors of suicide attempt. Additional research would be needed to evaluate the effectiveness of prevention programs for at-risk outpatients identified by screening.
Our findings have implications for current practice. Systematic use of the PHQ-9 (or some other standard outcome assessment) is an essential element of effective depression treatment (
40,
41). In this sample, approximately one in ten outpatients completing the most widely used depression outcome questionnaire reported thoughts of death or self-harm “more than half the days” or “nearly every day,” and those patients experienced a markedly increased risk of subsequent suicide attempt and suicide death. For this high-risk group, additional assessment is clearly indicated. Available structured assessments include the Columbia Suicide Severity Rating Scale (
17) or the P4 screener (
42).
It is notable that excess risk of suicide attempt emerged over several days and continued to grow for several months. Clinical response to suicidal ideation typically emphasizes immediate risk and urgent interventions. These findings emphasize the need for sustained and organized follow-up care to address ongoing risk. Suicidal ideation should be viewed as an enduring vulnerability rather than simply a short-term crisis.
Conclusions
Response to item 9 of the PHQ-9 identified outpatients at increased risk of suicide attempt and suicide death. This excess risk emerged over several days and continued to grow for several months, indicating that suicidal ideation was an enduring vulnerability rather than a short-term crisis.
Acknowledgments and disclosures
This study was funded by cooperative agreement U19MH092201 from the National Institute of Mental Health.
The authors report no competing interests.