Over two million people with serious mental illness enter jails in the United States each year (
1), and the prevalence of major psychiatric disorders among incarcerated men and women—about 15% and 30%, respectively (
1)—is significantly higher than in the general population (about 5%) (
2). Although rates of incarceration in the general population have also risen (
3), the trend of increasing justice involvement among people with serious mental illness has been attributed to various legal and policy changes over the past half century, including deinstitutionalization, increasingly restrictive criteria for civil commitment, insufficient availability of community mental health services, and harsher sentencing for drug crimes (
4,
5).
Although reasons for the overrepresentation of adults with a mental illness in the justice system are complex, there are several well-established risk factors for justice involvement in this population. Some of these risk factors are shared by the general population, and others are unique. Like the general population, persons with serious mental illness are placed at greater risk of justice involvement by substance abuse; up to 80% of adults with mental illness who are involved with the justice system also have co-occurring substance use disorders (
6–
12). Persons with serious mental illness—and, perhaps, especially those with bipolar disorder (
13)—also have a modestly elevated risk of violent behavior compared with the general population (
13–
21). Studies of factors related to violent behavior have generally found co-occurring substance use disorders to have a stronger influence than most psychiatric symptoms (
13,
17,
18,
20,
21).
Gender is a significant but ambiguous correlate of committing criminal offenses among people with serious mental illness. In absolute terms, men are much more likely than women to commit criminal offenses, and that is true both in the general population (
22,
23) and among persons with mental illness (
1,
10). However, among all incarcerated individuals, serious mental illness is twice as prevalent among women than men (
1,
7–
9), and incarceration rates are rising faster for women (
24). Moreover, evidence also suggests that female inmates with serious mental illness are more likely than their male counterparts to have a co-occurring substance use disorder (
7).
Evidence also indicates that gender and co-occurring substance use disorders are associated with important variations in offending patterns by primary psychiatric diagnosis. Two of the so-called central eight criminogenic risk factors, substance abuse and antisocial personality pattern, are also not uncommon characteristics of psychiatric disorders and may occur more commonly among patients with bipolar disorder than among patients with schizophrenia. Epidemiologic research has demonstrated that antisocial personality disorder is highly prevalent among male inmates (
7,
25) and that there is a sizable overlap of clinical features of antisocial personality disorder and bipolar disorder. In a sample of adults with mental illness and co-occurring substance use disorders, those with antisocial personality disorder were more likely to have a diagnosis of bipolar disorder than of schizophrenia (52% versus 21%) (
26). A core feature shared by both disorders is impulsivity (
27–
30), a common trait among offenders with no mental disorder, so bipolar disorder may be associated with a higher risk of criminal behavior compared with schizophrenia. Evidence from a recent study of the cost of justice involvement among adults treated by the Connecticut public mental health system supports this hypothesis. Thirty-four percent of adults with bipolar disorder had some justice involvement, compared with 21% of those with schizophrenia (
10). Another recent study found that adults with bipolar disorder were at especially high risk of multiple incarcerations (
31).
This analysis aimed to identify how interactions among gender, primary psychiatric diagnosis, and co-occurring substance use disorder influenced the risk of committing criminal offenses among adults with schizophrenia spectrum disorders or bipolar disorder. We hypothesized that these three person-level characteristics interact in a multiplicative way, increasing a person’s risk of committing a criminal offense in a way that exceeds their additive effect. Thus we expected that the combination of these three characteristics—which, arguably, capture many other risk factors for offending shared with the general population—creates conditions that maximize the risk potential of each variable alone. For example, among men, the mood instability and impulsiveness associated with bipolar disorder could trigger male traits for aggression and violence that may normally be inhibited. Similarly, a combination of misuse of drugs or alcohol and the presence of other psychopathology not only may add to men’s risk of criminal behavior but may compound the risk, for example, by exaggerating impulsiveness, exacerbating threat perception and hostility, disinhibiting aggressive or antisocial behavior, creating criminal associations and opportunities, and motivating acquisition of illegal drugs (
32).
Methods
These analyses used merged administrative records from a previous study of 25,133 adults in Connecticut who were clients of the Department of Mental Health and Addiction Services (DMHAS) sometime during fiscal years 2006–2007, either for inpatient or outpatient treatment services, and had a diagnosis of schizophrenia spectrum disorder (including schizophrenia and schizoaffective disorder) or bipolar disorder (
10). Full methodologic details for these study data have been described elsewhere (
10). We used demographic and clinical diagnostic data from the DMHAS, which records this information at the client’s admission (either inpatient or outpatient) and reviews the information every six months. Arrest data for criminal offenses that resulted in convictions were obtained from the Connecticut Department of Public Safety, and jail and prison data were obtained from the Connecticut Department of Correction (DOC). All analyses using the deidentified data described above were approved by jurisdictional institutional review boards in Connecticut and at Duke University.
Measures
Dichotomous variables were coded for primary psychiatric diagnosis—schizophrenia and bipolar disorder—and for a chart diagnosis of co-occurring substance use disorder. Demographic variables included age, gender, and race-ethnicity. We created a dummy variable for any type of justice involvement during the study window, including any criminal convictions, incarceration, periods of probation or parole, participation in the state’s jail diversion program, forensic evaluations to determine competency to stand trial, and forensic hospitalizations. These different types of justice involvement vary both by proximity in time to the offense and by type, for example, diversionary, procedural, or treatment related. Because this measure captures more instances of justice involvement than just arrests or incarceration in jail, it was useful for assessing justice involvement during a brief study window of two years. For criminal convictions, we coded categorical variables for any conviction, any violent-crime conviction, any felony conviction, any drug conviction, and any minor conviction, such as trespassing, breach of peace, prostitution, and technical violations of probation or parole. We also coded a dichotomous variable for any time spent in a DOC facility during the study period.
Analysis
We conducted two sets of multivariable logistic regression analyses, one testing the main effects of gender, primary diagnosis, and co-occurring substance use disorder on the odds of each type of justice involvement and one testing whether the various combinations of those three characteristics had multiplicative effects on the odds of conviction for specific types of crime. We stratified the sample by gender, in keeping with an assumption that there could be fundamental, unmeasured differences between men and women in the pathways to offending. We then created four interaction categories for each gender to represent all possible combinations of gender, primary diagnosis, and co-occurring substance use disorder. In all regression models, the reference group was men and women, respectively, and schizophrenia with no co-occurring substance use disorder (“schizophrenia alone”). We corrected for potential type I error by applying a relatively stringent p value threshold (p<.01), rather than the more standard value (p<.05).
All covariates were modeled as dummy variables except age, which was converted to quadratic form to account for a nonlinear effect of age. Race-ethnicity covariates in the regression models controlled, at least in part, for a number of factors that are known to be important correlates of minority racial status but that we could not measure directly, including social and environmental characteristics that are associated with risk of justice involvement, such as poverty and living in a high-crime neighborhood with heightened police presence.
Results
Table 1 displays the demographic and diagnostic characteristics of the 25,133 adults with schizophrenia or bipolar disorder who were DMHAS clients during fiscal years 2006–2007. Adults with co-occurring disorders were significantly younger than their counterparts with mental illness alone (mean=38.8 versus 42.9 years old), and among those with mental illness alone, men were significantly younger than women (41.5 versus 44.1 years old). Adults with co-occurring disorders were significantly more likely than those with mental illness alone to be African American (19.0% versus 13.7%) and less likely to be from a racial-ethnic group categorized as “other” (4.7% versus 9.1%). Furthermore, among persons with co-occurring disorders, more women than men were non-Hispanic white (63.3% versus 60.4%), and among persons with mental illness alone, more men than women were African American (14.9% versus 12.7%).
Finally, compared with persons with mental illness alone, persons with co-occurring disorders were significantly more likely to have bipolar disorder (56.5% versus 47.5%). There were marked differences in distribution of primary diagnosis by co-occurring substance use disorder and gender. Among women with co-occurring disorders, 68.5% had a primary diagnosis of bipolar disorder and 31.5% had a diagnosis of schizophrenia; among men with co-occurring disorders, the distribution of primary diagnoses was much closer to equal. A similar pattern was evident among the group with mental illness alone; 61.9% of men had a primary diagnosis of schizophrenia, and 38.1% had a diagnosis of bipolar disorder.
Among those with some justice involvement during the study period (N=6,904, 27.5%), there were some statistically significant differences in prevalence of various types of justice involvement by gender and co-occurring disorder (
Table 2). Justice involvement was more common among people with co-occurring disorders than among people with mental illness alone for several categories, including any jail days (61.4% versus 50.0%), any probation days (49.3% versus 44.9%), any jail diversion days (30.3% versus 25.3%), any criminal convictions (64.3% versus 56.4%), two or more convictions (27.6% versus 19.8%), three or more convictions (11.7% versus 7.4%), and at least one felony conviction (23.9% versus 19.4%). This pattern was evident for both men and women. Notably, in most of the categories listed above, offending rates among women with co-occurring disorders surpassed those of men with mental illness alone.
Other notable results from the stratified but otherwise unadjusted analysis of convictions include a lack of statistically significant difference in the prevalence of violent-crime convictions by co-occurring substance abuse disorder. This finding indicated that unless held constant, race and age exerted effectively equal influences on the risk of violent crime among persons with and without a co-occurring substance use disorder. (However, once race and age were included as covariates in regression models, there were significant differences in risk of violent crimes by co-occurring substance use disorder.) Still, men in either group were far more likely to have a violent-crime conviction than their female counterparts. The largest differences in conviction rates among patients with or without a co-occurring disorder were for property crimes (17.8% versus 12.8%) and drug crimes (14.7% versus 10.3%). Moreover, the differences in rates of convictions for property crimes by co-occurring disorder were most notable for men. The prevalence of these convictions was 57% higher among men with co-occurring disorders than among men with mental illness alone (18.0% versus 11.5%). The converse was evident for drug crimes; women with co-occurring disorders had an 80% higher prevalence of drug crime convictions than women with mental illness alone (15.1% versus 8.4%).
The gender-stratified logistic regression models that estimated interaction effects of primary diagnosis and co-occurring substance use disorder on odds of justice involvement, or “offending,” produced very consistent patterns. For all study outcomes, and for both men and women, the risk of offending was highest among persons with a diagnosis of bipolar disorder and a co-occurring substance use disorder versus schizophrenia alone. The odds of any justice involvement, any criminal convictions, or any jail days were each seven to eight times higher for men with bipolar disorder and a substance use disorder than for men with schizophrenia alone (p<.001), who demonstrated lower risk compared with each of the other three combinations (
Table 3). Among women, the combined effect of bipolar disorder and substance use disorder was even stronger. Women with this combination had from nine to nearly 12 times higher odds of any justice involvement, any arrests, and any jail days compared with women with schizophrenia alone (p<.001). For both men and women, the odds of having any of these three main types of offending relative to persons with schizophrenia alone were incrementally lower among the subgroups without bipolar disorder and a substance use disorder, compared with the subgroup with both risk factors. The odds ratios for risk of offending with both bipolar disorder and substance use disorder did not, however, distinguish which condition contributed more to the elevated risk compared with schizophrenia alone.
Similar patterns were found in the stratified logistic regression models that estimated how combinations of characteristics served as risk factors for specific types of criminal conviction, including conviction for a violent crime, a felony, a drug crime, and a minor offense (
Table 4). Here, too, the odds of offending were highest among those with bipolar disorder and substance use disorder, especially for women. Compared with men with schizophrenia alone, men with bipolar disorder and substance use disorder had nearly six times greater odds of a felony conviction (p<.001). The odds of a drug conviction were nearly 12 times greater among women with bipolar disorder and a substance use disorder than among women with schizophrenia alone (p<.001). The combined influence of having bipolar disorder and a co-occurring substance use disorder was much more intense for women than men; for example, compared with their counterparts with schizophrenia alone, women with bipolar disorder and a substance use disorder were more likely (OR=11.78, p<.001) than men (OR=4.88, p<.001) with the same disorders to have a drug conviction. This pattern was also seen in the models of outcomes of other measures of criminal offenses (
Table 3),
For all outcomes presented here, the effect of adding substance abuse as a risk factor for offending appears to be strongest for women, especially those with schizophrenia.
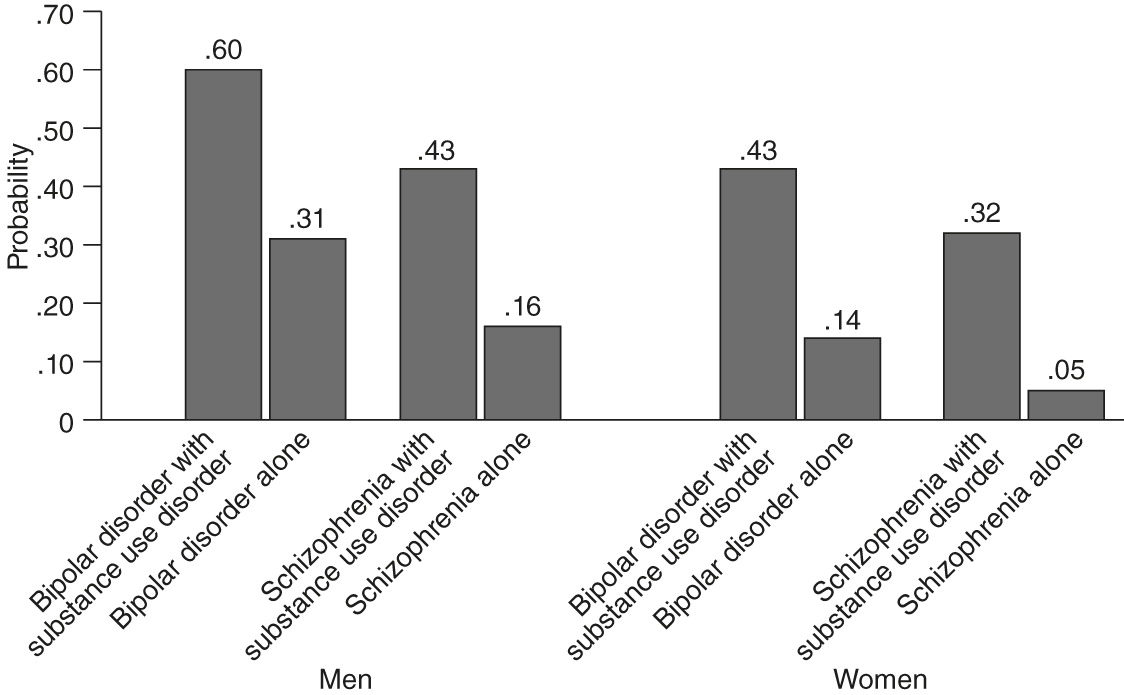
Figure 1 presents predicted probabilities from the logistic regression model for any justice involvement. The patterns shown here were evident in all the analyses across specific types of offenses as well. Among women with bipolar disorder, the predicted probability of having any justice involvement was 3.1 times higher when substance use disorder was present; 43% of women with bipolar disorder and a substance use disorder versus 14% with bipolar disorder alone had any justice involvement. Among women with schizophrenia, however, the predicted probability of having any justice involvement was 6.4 times higher when substance abuse was present; 32% of women with schizophrenia and a substance use disorder versus 5% with schizophrenia alone had any justice involvement.
Discussion
The analyses presented here add important new evidence about the way gender and diagnostic characteristics worked together among a population of adults with schizophrenia and bipolar disorder to influence their risk of justice involvement and identified subgroups of this heterogeneous population who were at relatively high risk of offending. As hypothesized, bipolar disorder in combination with substance use disorder was associated with the highest odds of offending compared with schizophrenia alone. Although men in this group had the highest absolute risk of offending, women in this group had an especially strong relative risk of offending compared with women with schizophrenia only.
For both men and women, having bipolar disorder versus schizophrenia significantly increased risk of offending, even in the absence of a comorbid substance use disorder, and it appeared to have a particularly strong influence on risk of offending among men with a substance use disorder. For women, bipolar disorder was associated with more than double the risk of offending associated with schizophrenia (except for violent crimes, where the p<.01 threshold for statistical significance was not met); however, substance abuse appeared to be, by far, the risk factor most strongly predictive of offending, especially among women with schizophrenia.
The relative risks (estimated by odds ratios) and predicted probabilities of offending were highest among men with bipolar disorder and substance use disorder—ranging from 40% to 60% probability of offending during the two-year study period. Among women, bipolar disorder and substance use disorder each, but especially in combination, appeared to have a marked effect, significantly raising risk of offending compared with schizophrenia alone. Consistently, women’s risks of offending increased the most when substance abuse was present—depending on the offense, the probability of offending among women with a co-occurring disorder was anywhere from three to nearly 12 times greater than among their counterparts with schizophrenia alone. Differences in baseline risks of offending associated with bipolar disorder and schizophrenia may explain the different contributions of substance abuse to increased risk of offending among persons with bipolar disorder compared with persons with schizophrenia. Bipolar disorder already is associated with a higher baseline risk—even without substance abuse—so the addition of substance use disorder may not have contributed as much to risk of offending as it did among individuals with schizophrenia, which is associated with a lower baseline risk of offending.
There are important limitations to these analyses. First, use of administrative data for diagnostic information has inherent shortcomings. For example, substance use disorders are often underdetected or are not documented by mental health providers (
33–
35). Thus some adults in our analytic sample who were categorized as having mental illness alone may, in fact, have had a substance use disorder, which could bias our model estimates. Also, administrative data for psychiatric diagnoses are not as valid or reliable as data from structured diagnostic interviews administered at the time of data collection. However, the DMHAS makes concerted efforts to collect and record valid diagnostic data for its clients; diagnoses are recorded at clients’ admission to the system (either inpatient or outpatient) and are reviewed at least every six months. Furthermore, we did not have any direct measures of other diagnoses, for example, antisocial personality disorder; personality traits, such as emotional reactivity and impulsivity; or social-environmental factors that are strong predictors of offending. In addition, a more precise distinction between schizophrenia and bipolar disorder is difficult to make without structured research interviews, so we cannot fully assess how well these data captured unique differences between schizophrenia and bipolar disorder. Also, to understand more about the unique contribution of substance abuse for men and women, it would have been helpful to have a comparison group of adults with only substance use disorders and no mental illness, but these data were not available. Future research should incorporate that subgroup if possible.
This work focused on the interactive effects of gender, substance use disorder, and type of major psychiatric diagnosis to understand more about differential patterns of offending within a heterogeneous population of adults with schizophrenia or bipolar disorder. Our results suggest that men who have bipolar disorder and a co-occurring substance use disorder are at especially high risk of committing all types of offenses compared with men with schizophrenia alone. We have also demonstrated in this sample of adults with mental illness that a substance use disorder appears to raise the risk of offending most dramatically for women, mostly among those with schizophrenia, whose base risk of offending is likely lower than that of women with bipolar disorder. This group may be especially good candidates for integrated treatment interventions that focus on treating mental illness and substance use disorders as a way to reduce justice involvement.
Next steps in this line of research should include testing these subgroup effects in other populations of adults with mental illness and measuring the contributing influences of other key criminogenic risks and socioenvironmental conditions. Future research should also aim to untangle the conceptual overlap between crime-relevant symptoms of bipolar disorder and antisocial traits that characterize a large majority of offenders with and without mental illness. Empirical evidence indicates that very little criminal behavior among people with mental illness is attributable to their mental illness (
36) and that other characteristics, such as criminal history and deviant lifestyle, are more predictive of offending (
37–
39). Further, it is unclear how particular symptoms of mental illness, for example, types of psychosis, may play a role, perhaps by combining with personal or situational factors, in raising risk of offending (
40). What clinicians identify as symptoms of mental illness, such as impaired mood regulation, impulsivity, hostility, lack of empathy, and excessive threat perception, may be characterized by corrections professionals as criminogenic features. Understanding the overlaps and distinctions between mental illness symptoms and criminal behavior traits would be an important step toward addressing each more effectively.
Conclusions
Once the subgroups of adults with mental illness at highest risk of justice involvement are identified more definitively, practitioners in both the criminal justice and mental health systems can identify persons with behavioral health disorders at highest risk of recidivism. This will require an integrated approach that addresses criminogenic risk and behavioral health needs and optimizes responsivity through targeted, fully integrated treatment.
Acknowledgments and disclosures
Dr. Swartz serves as a consultant to Med-IQ. The other authors report no competing interests.