Despite empirical evidence supporting its efficacy (
1–
3), psychotherapy is substantially underutilized in the United States. A minority of patients with a mental disorder engage in psychotherapy (
4,
5), with roughly one-third of psychotherapy patients receiving only one or two sessions (
6). National trends in psychotherapy use from the late 1990s through the mid-2000s suggest that the number of patients accessing psychotherapy and the number of sessions they receive may be declining as pharmacotherapy accounts for an increasing proportion of mental health services (
6,
7).
Recently, initiatives to increase access to psychotherapy have proliferated. In particular, integration of psychotherapy into primary care settings has increased psychotherapy engagement among patients who might otherwise refuse these services because of stigma or other factors (
8–
10). Similarly, psychotherapy via telephone or video teleconference (“telepsychotherapy”) has shown promising evidence of enhanced access for patients unable to travel to traditional care settings (
11,
12). Clinical practice guidelines also have highlighted the effectiveness of several evidence-based psychotherapies for specific psychiatric conditions, and, accordingly, numerous health care systems have prioritized the delivery of these treatments (
3,
13).
The Veterans Health Administration (VHA), the largest integrated health care system in the United States (
14), provides a unique opportunity to examine changes in psychotherapy utilization that may have resulted from widespread transformations in psychotherapy programming. Rates of VHA psychotherapy use mirror those of national community samples and reflect significant underutilization. Data from fiscal years (FYs) 2003 and 2004 suggest that only 22%−35% of VHA patients with depression or anxiety received any psychotherapy, and even fewer received an adequate number of sessions (
15,
16).
In 2004, the VHA released the Mental Health Strategic Plan (
17), which outlined more than 200 initiatives to improve mental health care for veterans. Between 2005 and 2011, the VHA hired more than 3,500 mental health professionals and tripled spending on mental health care (
18). Paralleling changes in the private sector, funding for the VHA’s Primary Care–Mental Health Integration Program commenced in 2007 (
8,
13), and recent VHA guidelines have encouraged the use of telepsychotherapy services to leverage technology to broaden access to mental health care (
13). The VHA has also endorsed evidence-based psychotherapies, including prolonged exposure (
19) and cognitive processing therapy (
20) for posttraumatic stress disorder (PTSD) and cognitive-behavioral therapy (
21) and acceptance and commitment therapy (
22) for depression. Nationwide rollouts of these treatments, including multiday didactic workshops and follow-up consultation for providers, are under way (
23,
24). As of August 2012, the VHA had trained more than 6,000 providers in evidence-based interventions, dramatically increasing its capacity to administer these treatments.
This study used national VHA administrative databases to conduct an unprecedented examination of psychotherapy utilization in the VHA over a seven-year period. Although VHA administrative databases do not include information on non-VA service use, they provide valuable information about VHA-specific service patterns. This study examined whether broad programmatic changes in VHA mental health care have translated into improved psychotherapy services, including receipt and amount of psychotherapy, treatment modality, and timeliness of care.
Methods
After receiving institutional review board approval, this retrospective database study used data from the VHA National Patient Care Database (NPCD) outpatient treatment files for veterans who received care during FY 2004 (October 1, 2003, to September 30, 2004), FY 2007 (October 1, 2006, to September 30, 2007), and FY 2010 (October 1, 2009, to September 30, 2010). The NPCD contains encrypted patient identifiers linked to patient and service characteristics and is available for health services research (
25).
Patient population
This study focused on patients who received a new diagnosis of depression, anxiety, or PTSD in VHA outpatient facilities during the specified years. Patients were categorized, using
ICD-9-CM codes, into three diagnostic groups: depression (codes 293.83, 296.20–296.36, 300.4, and 311), anxiety (codes 293.84, 293.89, 300.00–300.02, 300.09, 300.20–300.23, 300.29, and 300.3), and PTSD (codes 308 and 309.81). These diagnostic categories were selected because they are highly prevalent and disabling within the VHA patient population (
26), and substantial evidence supports the use of psychotherapy as a primary or secondary treatment for these diagnoses (
27). PTSD was examined separately because of its high prevalence and impact in the veteran population and because of the focus on enhancing access to PTSD-specific treatments within the VHA during the study time frame (including nationwide rollouts of two evidence-based psychotherapies).
As detailed in previous work (
15), restricting the sample to patients with new-onset diagnoses allowed the assessment of time between diagnosis and receipt of psychotherapy and provided a fair test of whether those newly identified by the system received indicated care. A new-onset condition was defined as six months without a related diagnosis before the index date (the date of first diagnosis during the study period). To avoid overlapping
ICD-9-CM coding, conditions occurring within diagnostic categories (such as major depression and dysthymia) were considered one condition. Patients with multiple new-onset conditions were classified into more than one diagnostic category (for example, patients with new-onset depression and new-onset anxiety were classified into both categories). Frequency statistics reported for the full fiscal year (FY) cohort (with diagnostic groups combined) are reported for unique patients. For diagnostic subgroup analyses, patients who were classified into multiple categories were represented in each of these diagnostic groups. We restricted the sample to patients with adequate opportunities to use outpatient psychotherapy services by excluding those with 60 or more inpatient days in the 180 days after diagnosis.
Psychotherapy, session frequency, and time to treatment
Patient use of mental health services was assessed during the 12 months after each patient’s index date. Psychotherapy use was determined on the basis of Current Procedural Terminology (CPT) codes and classified by treatment modality into individual psychotherapy (CPT codes 90804, 90806, 90808, 90810, 90812, 90814, 90845, 90875, 90876, and 96152) and group therapy (90849, 90853, 90857, and 96153). Psychotherapy exposure, defined as the number of patients receiving at least one session (any exposure to psychotherapy), four sessions (approximate length of briefer forms of psychotherapy [
28–
30]) or eight or more sessions (the minimum length of traditional, evidence-based psychotherapies for depressive and anxiety disorders [
19,
31]) was also assessed. Timeliness of psychotherapy was assessed by calculating the number of days between the patient’s index date and first psychotherapy visit.
Patient characteristics
We examined patients’ sociodemographic characteristics, including age, gender, and marital status. Patients’ residential zip codes were used to estimate income (using the average adjusted gross income for each zip code, based on 2008 Internal Revenue Service data) and distance in miles to the nearest VHA facility. Patient race was populated inconsistently in the NPCD and was therefore not reported. Because of the increased access to care provided to veterans with service-related disabilities, patients were categorized into three groups by service-related disability percentage, including 0%, 1%−49%, and ≥50%. Illness burden was assessed with a diagnosis-based, risk-adjustment methodology (
32,
33), which provides an odds ratio representing the predicted health care cost of each veteran compared with the average predicted cost (that is, the relative risk score).
Analyses
All analyses were descriptive. The proportion of patients receiving at least one, four, or eight psychotherapy sessions during the 12 months after their index date and the delay between diagnosis and psychotherapy were calculated for unique patients in each FY cohort and for specific diagnostic categories within each cohort. Subsequent analyses described treatment modality patterns (individual versus group psychotherapy) across the study time points. Effect size was calculated with odds ratios. Analyses were conducted with SAS version 9.2.
Results
Psychotherapy utilization
Table 1 lists the demographic and clinical characteristics of the cohorts from FY 2004 (N=424,428), FY 2007 (N=494,318), and FY 2010 (N=583,733); the steady growth in cohort size represents increases in the number of patients who received new-onset diagnoses of depression, anxiety, or PTSD. A minority of the sample met criteria for two diagnostic categories (FY 2004, 7.7%; FY 2007, 9.3%; and FY 2010, 10.9%). Notable changes in patient characteristics between FY 2004 and FY 2010 included a decrease in age, increased numbers of female veterans, greater medical illness burden, increased VA service-connected disability, and increases in co-occurring substance use diagnoses.
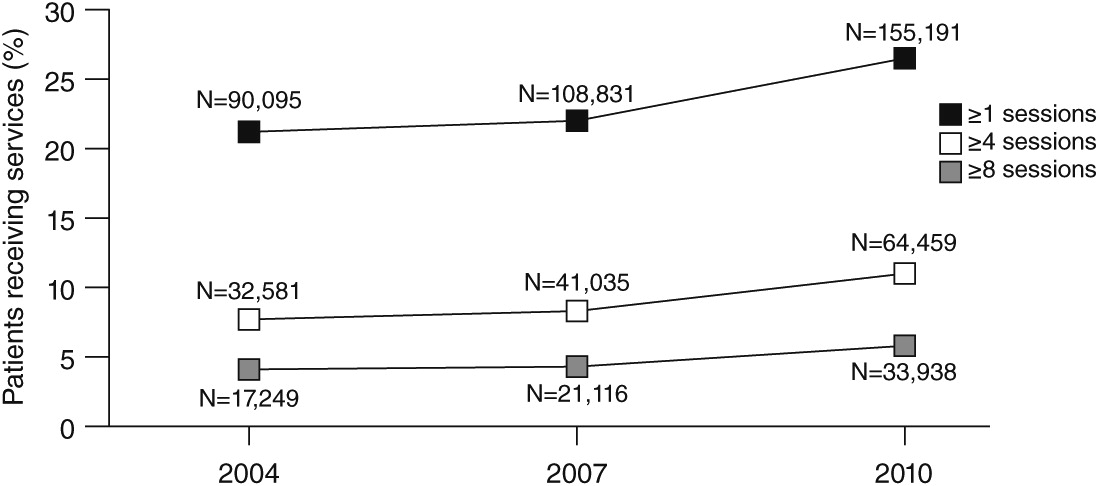
The raw number of patients receiving any psychotherapy grew by 72% between FY 2004 (N=90,095) and FY 2010 (N=155,191) (
Figure 1). The effect size, as measured by odds ratio (OR), was 1.34, which had a 95% confidence interval (CI) of 1.33–1.36. Examination of psychotherapy use from FY 2007 to FY 2010 (OR=1.28, CI=1.27–1.29) indicates greater increases in psychotherapy use during this period relative to between FYs 2004 and 2007 (OR=1.05, CI=1.04–1.06).
Amount of psychotherapy
Figure 1 presents percentages of patients who received at least one, four, or eight psychotherapy sessions. The number and proportion of patients who received each level of exposure increased across study time points. The most notable increase was in the number of patients who received at least one psychotherapy session, which grew by more than 65,000 between FYs 2004 and 2010. The number of newly diagnosed patients who received at least four sessions nearly doubled between FY 2004 (N=32,581) and FY 2010 (N=64,459), as did the number who received eight or more psychotherapy sessions (FY 2004, N=17,249; FY 2010, N=33,938). Across all levels of exposure, modest increases in psychotherapy use were observed between FY 2004 and FY 2007, with more substantial increases occurring between FY 2007 and FY 2010.
Examination of psychotherapy exposure according to diagnostic group revealed unique trends for patients with PTSD (
Table 2). Across all FY cohorts, PTSD patients demonstrated the highest rate of psychotherapy initiation and number of psychotherapy sessions. Although the proportion of PTSD patients who received psychotherapy remained relatively consistent from FY 2004 to FY 2010 (OR=.95, CI=.93–.97), rates of psychotherapy use increased among patients with depression (OR=1.40, CI=1.38–1.41) and among patients with anxiety (OR=1.59, CI=1.56–1.62), reducing disparities by diagnostic group in receipt of psychotherapy.
Descriptive analyses also revealed differences in utilization rates for group versus individual psychotherapy (
Table 3). For each cohort, patients were at least three times more likely to initiate individual psychotherapy than group psychotherapy. The proportion of each cohort that received at least one session of group psychotherapy consistently ranged from 6% to 7%. The proportion of patients receiving individual psychotherapy showed little change between FY 2004 (18%) and FY 2007 (19%) (OR=1.05, CI=1.04–1.06), with a more substantial increase between FY 2007 and FY 2010 (26%) (OR=1.33, CI=1.33–1.34). Data from all three cohorts revealed that group psychotherapy patients were more likely to receive more psychotherapy sessions. Across the full study sample, 34% of those who initiated group therapy received eight or more sessions (FY 2004, 35%; FY 2007, 32%; and FY 2010, 34%), compared with 12% of those who initiated individual psychotherapy (FY 2004, 10%; FY 2007, 11%; and FY 2010, 14%).
Timeliness
Treatment delays decreased across study time points. The median time between index diagnosis and psychotherapy dropped from 56 days (FY 2004) to 47 days (FY 2010), with the majority of change occurring from FY 2007 to FY 2010 (
Table 4). Although patients with PTSD consistently had shorter delays than patients with anxiety or depression, diagnostic disparities in time until treatment grew smaller across the study time points.
Discussion
Data from this investigation suggest that efforts to enhance the access to and quality of psychotherapy in the VHA over a seven-year span resulted in notable improvements. Across the study time points (FYs 2004, 2007, and 2010), the absolute number of patients with new diagnoses of depression, anxiety, or PTSD who received VHA psychotherapy services increased substantially. Whereas only modest growth occurred in the percentage of patients who received psychotherapy, given that the cohort of newly diagnosed patients increased by nearly 40% between 2004 and 2010, these small percentage changes reflect that the VHA provided psychotherapy to 65,096 more patients in 2010 than in 2004. These findings signify widespread increases in use of VHA psychotherapy.
Data from this study also indicate improvements related to psychotherapy exposure, with an increasing proportion of patients receiving eight or more psychotherapy sessions. This may represent a reversal in the trend identified by Rosenheck and Fontana (
34), who showed declines in the intensity of service use from 1997 to 2005. Additional studies are needed to determine whether these increases reflect improved patient outcomes.
The observed increases in psychotherapy sessions indicate growth in the number of patients who could have received a course of evidence-based psychotherapy. Previous researchers have used eight or nine sessions as the standard for a minimally adequate amount of evidence-based psychotherapy (
35–
37). Although the proportion of patients receiving eight or more sessions increased steadily across the study time points, less than 6% of each FY cohort could have completed an evidence-based protocol. However, there is increasing recognition that many patients may benefit from brief courses of psychotherapy, ranging from four to six sessions (
28–
30), and may demonstrate significant improvement after as few as four sessions of a standard-length, evidence-based protocol (
38). Even with this less conservative cutoff, only 11% of the FY 2010 cohort received at least four psychotherapy sessions, pointing to the need for continued efforts to increase engagement in evidence-based care.
Examination of psychotherapy timeliness revealed that time from diagnosis until psychotherapy decreased by nine days across the study period, with the most notable decreases for anxiety or depressive disorders. However, time between diagnosis and psychotherapy was consistently shortest for patients with PTSD. These improvements in timeliness of care are critically important, given that shorter time to treatment is a well-established treatment-enabling factor (
35). Although delays between diagnoses and psychotherapy may reflect both system-level factors (such as wait times) and patient-level factors (such as reluctance to initiate psychotherapy or preference to use medication as a first-line treatment), the median wait time of 47 days for the FY 2010 cohort suggests the need for additional efforts to enhance timeliness of VHA psychotherapy.
Consistent with previous studies (
5,
39,
15), more patients engaged in individual than group psychotherapy across all study years. Furthermore, utilization rates grew more substantially for individual psychotherapy than for group psychotherapy. This may be because several VHA-endorsed evidence-based psychotherapies for depression and PTSD are designed for individual delivery. Similar to previous studies (
15,
39), this study showed that patients who participated in group psychotherapy received more psychotherapy than those in individual psychotherapy. Reasons for this are unclear but may be partially attributable to the highly selective group therapy patient population or the structure of group psychotherapy treatments (which may be less likely to be time limited).
Factors influencing psychotherapy use
Improvements in the reach, amount, and timeliness of psychotherapy occurred during a period of dramatic increases in patient load, which likely reflects the success of several recent programmatic efforts within the VHA. Required screenings and evidence-based guidelines for assessment of mental disorders have allowed increased detection of psychiatric problems, a critical step in access to care.
Among the diagnostic categories examined in this study, rates of PTSD grew most substantially, increasing by more than twofold between 2004 and 2010. This is likely because of the VHA’s particular focus on identification and treatment of PTSD, given its substantial psychological and economic burden among veterans and the clear link between military trauma exposure and subsequent development of PTSD. Specific policy changes that may have contributed to increases in PTSD diagnosis include mandatory screening for PTSD symptoms and military sexual trauma in primary care (
40). Veterans with PTSD also had the shortest delays between diagnosis and psychotherapy and were more likely to initiate psychotherapy and receive adequate exposure than those in other diagnostic groups.
Although the VHA provided psychotherapy to many more veterans with new diagnoses of PTSD in 2010 than 2004, a majority continued to receive no exposure to VHA psychotherapy, despite numerous, ongoing PTSD-specific initiatives (such as evidence-based psychotherapy rollouts). There is a great need within the VHA for additional efforts to engage veterans in psychotherapy services.
Our study period also corresponded to a period of increased funding for VHA mental health services, expansion of mental health staff, evidence-based psychotherapy training initiatives, and the integration of psychotherapy into primary care. More substantial increases in psychotherapy reach, amount, and timeliness occurred in 2007−2010 relative to 2004–2007, which aligns with the implementation of several of these initiatives. Other recent policy changes that may have contributed to increases in both the number of newly diagnosed patients and the use of psychotherapy include cost-free VHA health care for Iraq-Afghanistan combat veterans for five years postdischarge and expanded efforts to engage rural veterans through community-based outpatient clinics and telepsychotherapy services (
41).
Limitations
This study used CPT codes to assess mental health service use. Although widely used in studies examining psychotherapy utilization, they are associated with several limitations: CPT codes do not capture the type of psychotherapy provided, and, although entered by the provider (and therefore reflective of the provider’s perspective of the care provided), the fidelity of these codes is not independently verified. The validity of provider-recorded diagnoses is similarly unknown. We defined psychotherapy amount as the number of sessions received and did not extract codes that reflect the length of each session, because these codes often represent ranges of time rather than a precise duration. We also did not examine use of non-VHA psychotherapy, and, given that many veterans are dual users of VHA and non-VHA services (
42), results likely underestimated the true rates of psychotherapy exposure within the study sample. Despite this limitation, these data are valuable in that they present a descriptive account of trends in VHA psychotherapy and reflect improvements in care that have likely resulted from efforts to transform VHA mental health services. Finally, this study did not examine medication use; evaluation of psychopharmacology for these diagnostic groups over this period would provide an even more comprehensive picture of how veterans’ mental health needs are being addressed.
Conclusions
This study examined changes in VHA psychotherapy use during a time of mounting support for the effectiveness of psychotherapy and unprecedented expansion of VHA mental health services. Findings highlight recent improvements in psychotherapy services with respect to reach, amount, and timeliness. Despite advances, results indicate that most VHA patients with new psychiatric diagnoses receive no psychotherapy or a low-intensity amount of it. Additional efforts to engage veterans in psychotherapy are needed. Future research should attempt to determine the relative impact of factors that influence psychotherapy use, including patient factors (such as concerns about stigma), provider factors (provider preferences), or system factors (including dissemination of evidence-based psychotherapies). This knowledge can guide the development of interventions to enhance psychotherapy use, thereby increasing the number of patients who receive, and ultimately benefit from, this care.
Acknowledgments and disclosures
This research was supported by the Office of Academic Affiliations VA Advanced Fellowship Program in Mental Illness Research and Treatment, the VA South Central Mental Illness Research, Education and Clinical Center, and the VA Health Services Research and Development Houston Center of Excellence (HFP90-020). The views expressed reflect those of the authors and not necessarily those of the U.S. Department of Veterans Affairs, the U.S. government, or Baylor College of Medicine. The authors thank Sonora Hudson for her thoughtful review and editing of this manuscript.
The authors report no competing interests.