Racial-Ethnic Disparities in Use of Antidepressants in Private Coverage: Implications for the Affordable Care Act
Abstract
Objective
Methods
Results
Conclusions
Methods
Results
| Private coverage(N=4,468) | Medicare(N=1,944)b | Medicaid(N=2,125) | Uninsured(N=1,679) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | N | % | N | % | N | % | N | % |
| Age (M±SEc) | 43.5±.3 | 64.1±.4 | 35.6±.6 | 41.6±.6 | ||||
| Gender | ||||||||
| Male | 1,445 | 34.1 | 652 | 33.1 | 588 | 30.1 | 652 | 43.3 |
| Female | 3,023 | 65.9 | 1,292 | 66.9 | 1,537 | 69.9 | 1,027 | 56.7 |
| Race-ethnicity | ||||||||
| Non-Hispanic white | 3,475 | 87.8 | 1,295 | 80.7 | 996 | 64.3 | 916 | 71.0 |
| Non-Hispanic black | 416 | 5.1 | 320 | 9.3 | 482 | 16.7 | 261 | 10.5 |
| Hispanic | 577 | 7.2 | 329 | 10.1 | 647 | 18.9 | 502 | 18.5 |
| Education | ||||||||
| 0–11 years | 634 | 11.2 | 741 | 30.0 | 1,197 | 50.7 | 585 | 28.2 |
| 12 years | 1,233 | 26.0 | 625 | 36.2 | 570 | 30.3 | 597 | 37.7 |
| ≥13 years | 2,578 | 62.9 | 558 | 33.9 | 343 | 19.0 | 483 | 34.1 |
| Family income (% federal poverty level) | ||||||||
| ≤124% | 359 | 5.6 | 873 | 37.5 | 1,428 | 62.5 | 726 | 36.3 |
| 125%–199% | 548 | 9.8 | 399 | 20.4 | 416 | 21.1 | 350 | 20.2 |
| 200%–399% | 1,611 | 34.1 | 450 | 26.3 | 237 | 13.8 | 430 | 28.4 |
| ≥400% | 1,950 | 50.6 | 222 | 15.8 | 44 | 2.6 | 173 | 15.1 |
| Mental health status | ||||||||
| Poor or fair | 955 | 20.8 | 822 | 40.1 | 993 | 47.2 | 601 | 35.4 |
| Good or excellent | 3,496 | 79.3 | 1,099 | 59.9 | 1,097 | 52.9 | 1,040 | 64.6 |
| General health status | ||||||||
| Poor or fair | 927 | 19.7 | 1,126 | 55.5 | 954 | 43.8 | 637 | 35.4 |
| Good or excellent | 3,525 | 80.3 | 797 | 44.5 | 1,135 | 56.2 | 1,005 | 64.6 |
| Marital status | ||||||||
| Never married | 897 | 21.5 | 283 | 14.0 | 779 | 39.0 | 458 | 28.5 |
| Married | 2,473 | 55.0 | 649 | 35.2 | 395 | 17.9 | 642 | 36.8 |
| Separated, divorced, or widowed | 913 | 20.5 | 995 | 50.8 | 629 | 31.8 | 514 | 32.3 |
| Employment status | ||||||||
| Unemployed | 1,132 | 23.3 | 1,805 | 91.5 | 1,665 | 75.7 | 860 | 45.4 |
| Employed | 3,336 | 76.7 | 139 | 8.5 | 460 | 24.3 | 819 | 54.6 |
| Activities of daily living (ADL) status | ||||||||
| No limitation | 4,386 | 98.7 | 1,655 | 88.0 | 1,981 | 95.6 | 1620 | 99.0 |
| Limited | 55 | 1.3 | 268 | 12.1 | 108 | 4.4 | 21 | 1.0 |
| Residence region | ||||||||
| No metropolitan statistical area (MSA) | 659 | 15.3 | 431 | 21.4 | 400 | 20.4 | 340 | 21.2 |
| MSA | 3,794 | 84.7 | 1,502 | 78.6 | 1,692 | 79.6 | 1305 | 78.8 |
| Chronic condition | ||||||||
| High blood pressure | 1,457 | 32.5 | 1,286 | 66.4 | 701 | 32.4 | 595 | 33.6 |
| Heart disease | 582 | 12.9 | 680 | 36.1 | 333 | 16.3 | 233 | 12.7 |
| High cholesterol | 1,614 | 37.7 | 1,146 | 61.6 | 554 | 26.0 | 441 | 25.1 |
| Diabetes | 432 | 9.7 | 573 | 28.1 | 276 | 11.4 | 175 | 8.7 |
| Joint pain | 2,380 | 54.3 | 1,495 | 77.0 | 1,111 | 56.0 | 950 | 58.4 |
| Arthritis | 1,311 | 29.4 | 1,277 | 67.0 | 692 | 33.0 | 477 | 28.3 |
| Asthma | 632 | 14.3 | 419 | 20.9 | 546 | 24.3 | 247 | 15.2 |
| Number of prescription drugs taken (M±SEc) | 3.8±.1 | 6.6±.1 | 4.1±.1 | 2.7±.1 | ||||
| Private coverage | Medicarea | Medicaid | Uninsured | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Antidepressant user | Total | Antidepressant user | Total | Antidepressant user | Total | Antidepressant user | |||||
| Race-ethnicity | N | N | % | N | N | % | N | N | % | N | N | % |
| Non-Hispanic white | 3,475 | 1,522 | 43.8 | 1,295 | 729 | 56.3 | 996 | 393 | 39.5 | 916 | 300 | 32.8 |
| Non-Hispanic black | 416 | 106 | 25.5 | 320 | 155 | 48.4 | 482 | 167 | 34.7 | 261 | 61 | 23.4 |
| Hispanic | 577 | 166 | 28.8 | 329 | 154 | 46.8 | 647 | 212 | 32.8 | 502 | 109 | 21.7 |
| Private coverage(N=4,468) | Medicarea(N=1,944) | Medicaid(N=2,125) | Uninsured(N=1,679) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | AOR | 95% CIb | p | AOR | 95% CIb | p | AOR | 95% CIb | p | AOR | 95% CIb | p |
| Race-ethnicity (reference: non-Hispanic white) | ||||||||||||
| Non-Hispanic black | .50 | .33–.66 | <.001 | .78 | .57–1.08 | .135 | .94 | .70–1.28 | .706 | .70 | .47–1.07 | .098 |
| Hispanic | .70 | .55–.89 | .003 | .81 | .58–1.12 | .204 | .92 | .70–1.21 | .560 | .87 | .61–1.23 | .422 |
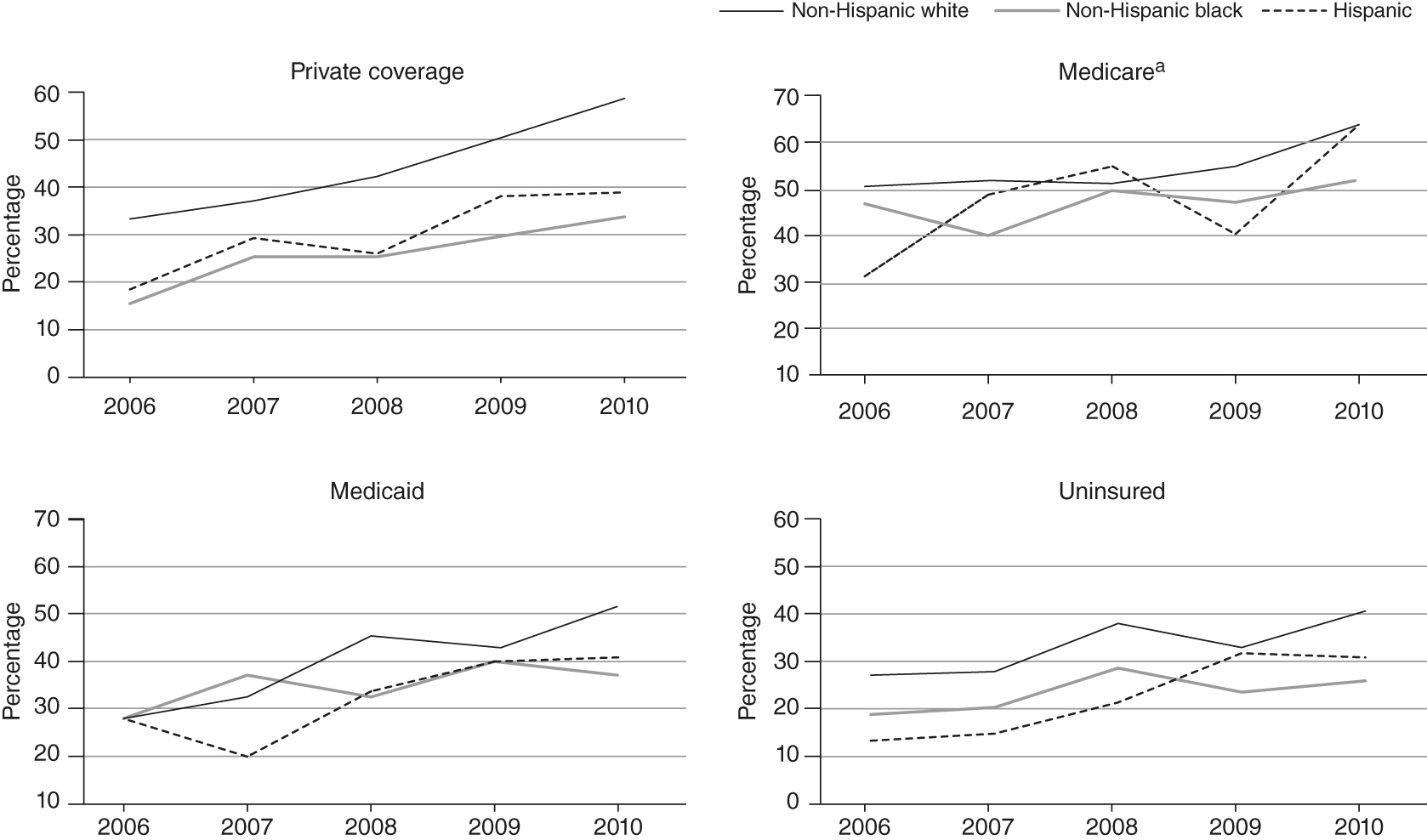
| Year (reference: 2006) | ||||||||||||
| 2007 | 1.26 | 1.05–1.51 | .011 | 1.03 | .80–1.32 | .830 | 1.11 | .83–1.48 | .475 | 1.07 | .75–1.52 | .709 |
| 2008 | 1.50 | 1.22–1.84 | <.001 | 1.06 | .77–1.46 | .731 | 1.77 | 1.30–2.43 | <.001 | 1.81 | 1.22–2.67 | .003 |
| 2009 | 2.17 | 1.78–2.64 | <.001 | 1.08 | .80–1.45 | .624 | 1.73 | 1.28–2.34 | <.001 | 1.69 | 1.15–2.47 | .007 |
| 2010 | 3.00 | 2.45–3.68 | <.001 | 1.80 | 1.34–2.43 | <.001 | 2.23 | 1.63–3.05 | <.001 | 2.12 | 1.47–3.15 | <.001 |
| Age (years) | 1.01 | 1.00–1.02 | .033 | 1.01 | .99–1.02 | .129 | 1.01 | 1.00–1.03 | .033 | 1.00 | .99–1.02 | .725 |
| Female (reference: male) | 1.06 | .90–1.25 | .506 | 1.02 | .79–1.30 | .898 | 1.17 | .89–1.52 | .259 | .91 | .67–1.22 | .515 |
| Education (reference: 0–11 years) | ||||||||||||
| 12 years | 1.06 | .82–1.38 | .641 | 1.02 | .77–1.32 | .908 | 1.15 | .87–1.51 | .340 | .91 | .64–1.29 | .586 |
| ≥13 years | 1.15 | .90–1.47 | .257 | 1.08 | .80–1.46 | .628 | 1.19 | .87–1.65 | .282 | 1.14 | .79–1.63 | .485 |
| Family income (reference: ≤124% federal poverty level ) | ||||||||||||
| 125%–199% | .98 | .72–1.34 | .905 | 1.01 | .77–1.32 | .951 | 1.03 | .80–1.34 | .802 | 1.12 | .80–1.58 | .503 |
| 200%–399% | 1.11 | .85–1.47 | .438 | 1.08 | .82–1.43 | .565 | 1.10 | .79–1.54 | .559 | 1.13 | .81–1.58 | .484 |
| ≥400% | 1.04 | .78–1.38 | .797 | 1.11 | .76–1.62 | .582 | .77 | .34–1.73 | .520 | 1.36 | .85–2.17 | .205 |
| Good or excellent mental health (reference: poor or fair) | .78 | .65–.93 | .007 | .83 | .66–1.04 | .110 | .74 | .59–.92 | .008 | .67 | .49–.89 | .006 |
| Good or excellent general health (reference: poor or fair) | 1.05 | .86–1.29 | .625 | 1.17 | .92–1.50 | .202 | 1.05 | .80–1.36 | .739 | 1.31 | .94–1.84 | .110 |
| Marital status (reference: never married) | ||||||||||||
| Married | 1.13 | .90–1.42 | .311 | 1.11 | .76–1.64 | .586 | .86 | .62–1.20 | .372 | 1.24 | .84–1.83 | .277 |
| Separated, divorced, or widowed | 1.03 | .78–1.35 | .842 | 1.15 | .79–1.66 | .460 | 1.05 | .76–1.45 | .755 | 1.26 | .83–1.91 | .287 |
| Employed (reference: unemployed) | .98 | .82–1.17 | .835 | 1.50 | .98–2.31 | .062 | .99 | .76–1.29 | .941 | .76 | .57–1.00 | .053 |
| Has limited activities of daily living (reference: no limitation) | .67 | .33–1.33 | .252 | .82 | .59–1.15 | .258 | 1.25 | .75–2.09 | .400 | .91 | .22–3.75 | .900 |
| Metropolitan statistical area (MSA) (reference: no MSA) | 1.00 | .81–1.25 | .970 | .94 | .71–1.26 | .708 | .71 | .53–.95 | .022 | 1.08 | .75–1.54 | .684 |
| Chronic condition | ||||||||||||
| High blood pressure | .99 | .82–1.20 | .945 | 1.02 | .79–1.31 | .904 | .88 | .65–1.19 | .408 | .99 | .67–1.43 | .971 |
| Heart disease | .80 | .63–1.01 | .060 | .67 | .52–.87 | .002 | .71 | .51–1.00 | .049 | .75 | .49–1.14 | .175 |
| High cholesterol | 1.08 | .90–1.28 | .411 | 1.12 | .88–1.43 | .353 | 1.16 | .85–1.58 | .350 | 1.44 | 1.04–2.01 | .030 |
| Diabetes | .76 | .57–1.01 | .061 | .72 | .55–.94 | .017 | .57 | .38–.84 | .004 | .58 | .35–.98 | .040 |
| Joint pain | .92 | .78–1.09 | .317 | 1.04 | .79–1.38 | .762 | 1.10 | .85–1.43 | .464 | .90 | .67–1.21 | .487 |
| Arthritis | 1.01 | .84–1.22 | .904 | .81 | .62–1.06 | .122 | .95 | .72–1.27 | .739 | .83 | .58–1.20 | .327 |
| Asthma | 1.02 | .82–1.26 | .877 | .78 | .58–1.05 | .099 | .94 | .72–1.21 | .612 | .57 | .38–.91 | .018 |
| Number of prescription drugs taken | 1.22 | 1.18–1.27 | <.001 | 1.22 | 1.17–1.28 | <.001 | 1.22 | 1.16–1.29 | <.001 | 1.48 | 1.36–1.60 | <.001 |
| Subgroup analysis of those at 125%–399% FPL(N=2,159)a | With cost-sharing index (overall analysis of private coverage)(N=4,468) | |||||
|---|---|---|---|---|---|---|
| Variable | AOR | 95% CIb | p | AOR | 95% CIb | p |
| Race-ethnicity (reference: non-Hispanic white) | ||||||
| Non-Hispanic black | .54 | .38–.76 | <.001 | .56 | .42–.74 | <.001 |
| Hispanic | .67 | .49–.92 | .013 | .71 | .56–.91 | .006 |
| Cost-sharing index | .82 | .64–1.06 | .126 | |||
Discussion
Main findings
Implications and future research
Limitations
Conclusions
Acknowledgments and disclosures
References
Information & Authors
Information
Published In

Cover: Girl on a Swing, by Maxfield Parrish. Drawing, oil on paper. The Metropolitan Museum of Art, bequest of Susan Vanderpoel Clark (67.155.3). Image © Metropolitan Museum of Art, New York. Image source: Art Resource. New York.
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
