Individuals who are admitted to the hospital or the emergency department for suicidal ideation or deliberate self-harm are at high risk of attempting or reattempting suicide after discharge (
1–
4). As described in the 2012 National Suicide Prevention Strategy, continuity of care and smooth transitions from an inpatient stay or emergency department visit to outpatient follow-up treatment are important ways to minimize this risk (
5). Strategies for improving care transitions include enhanced discharge planning; postdischarge contacts, such as telephone calls, crisis cards with emergency telephone numbers and safety measures, and letters of support; and postdischarge case management to promote access and adherence to recommended treatment.
Luxton and colleagues (
6) recently reviewed empirical studies of the effect of follow-up contacts on suicidal behaviors (suicide, attempts, and ideation) among patients in inpatient psychiatric or emergency departments who were being discharged to home. They identified 11 articles and eight unique studies. Seven articles reported a statistically significant reduction in at least one measure of suicidal behavior or ideation (
7–
13), three reported a trend toward improvements in the suicidal behavior or ideation outcomes that did not reach statistical significance (
14–
16), and one study found no affect (
17). They concluded that repeated follow-up contacts appear to reduce suicidal behavior, although more research is needed to determine which factors might make follow-up contact modalities more effective.
Financial support for providing postdischarge follow-up calls is limited but expanding. The Substance Abuse and Mental Health Services Administration (SAMHSA) has established 18 grants since 2008 to support delivery of follow-up calls by call centers participating in the National Suicide Prevention Lifeline (
18). Some local governments and charitable organizations have provided financial support for call centers that are collaborating with hospitals and emergency departments. Two new transitional care management procedure codes established in the 2013 Current Procedural Terminology (CPT) code book (codes 99495 and 99496) have been approved for use among Medicare beneficiaries (
19).
Of the various interventions for improving transitions of care, postdischarge follow-up calls may be particularly promising because they are a relatively inexpensive service. This study examined the business case for providing postdischarge follow-up calls to individuals who had a hospital stay or emergency department visit for suicidal ideation or deliberate self-harm by estimating the return on investment (ROI).
Methods
ROI framework
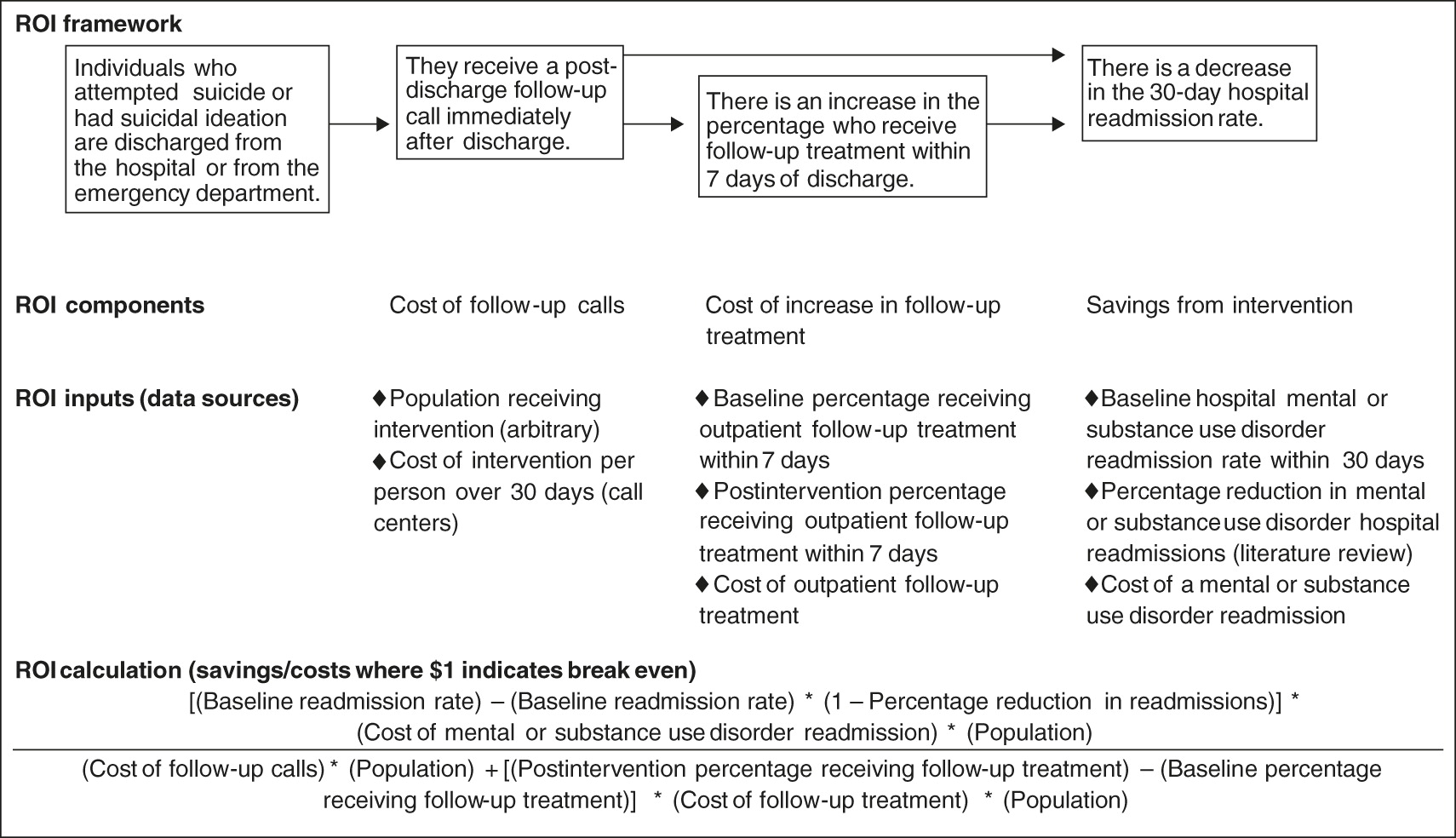
The model focused on the ROI within 30 days after discharge from a suicide-related hospitalization or emergency department visit (
Figure 1). We used a 30-day time horizon because this is the time of greatest risk for suicide and readmissions. The model was estimated from the payer’s perspective. It compared the baseline case, which consists of current costs and readmission rates, to the hypothetical case in which postdischarge follow-up calls are provided to everyone who has a suicide-related hospitalization or emergency department visit. ROI (the return that payers would gain for every $1 invested) was determined by calculating incremental savings from reduced hospital readmissions given the intervention divided by the incremental costs of the intervention (follow-up calls) and the costs of any additional treatment that might result from the follow-up calls in the 30 days after discharge. We separately estimated inputs for individuals discharged from the hospital, discharged from the emergency department, with commercial insurance, and with Medicaid coverage.
Data sources
Data sources included the Truven Health MarketScan Commercial Claims and Encounters Database and Multi-State Medicaid Database. The commercial claims database is a longitudinal database of health insurance claims that includes information from across the continuum of care from large employers and health plans in the United States. The Medicaid database is similar but consists of Medicaid claims from more than ten geographically disparate states. We examined events that occurred from January 1, 2006, to December 31, 2011. We identified individuals who had a hospital stay or emergency department visit with a diagnosis of suicidal ideation or deliberate self-harm (ICD-9-CM codes V62.84 and E950–E959). From the commercial claims database, we identified 106,948 hospital inpatient discharges and 56,374 emergency department discharges with these codes. From the Medicaid database, we identified 57,423 inpatient discharges and 32,960 emergency department discharges.
Eight call centers that currently collaborate with hospitals and emergency departments to provide postdischarge follow-up calls provided us with data on the cost of this service. Three of the call centers reported collaborating with ten or more health care facilities, and the remainder collaborated with four or fewer facilities. The call centers had different requirements for personnel providing the follow-up calls. Five centers required at least a bachelor’s or associate’s degree, and the remaining three required licensed professional social workers or counselors with master’s degrees. The call centers were located in Texas, Pennsylvania, New York, Florida, North Dakota, Ohio, and Washington.
Inputs regarding savings
The MarketScan databases were used to calculate the percentage of individuals with a suicide-related hospitalization or emergency department visit who were readmitted to the hospital with a principal mental or substance use disorder diagnosis within 30 days of discharge. We examined mental health and substance abuse readmissions rather than suicide-specific readmissions because suicide may be underdiagnosed in claims data and because individuals readmitted for a mental health or substance use condition within 30 days after an initial suicide-related event are highly likely to be at risk of suicide (
2,
20,
21). We excluded approximately 10% of individuals who were not continuously enrolled in the MarketScan databases during the 30 days after discharge, individuals with a readmission on the same day of discharge, and individuals with an admission to the hospital the day after the emergency department visit. This final group could have been transfers to hospitals (
22–
24). MarketScan was used to determine the average cost of hospital readmissions. We adjusted costs to 2011 U.S. dollars by using the medical component of the consumer price index.
Findings from randomized controlled studies identified in a comprehensive review by Luxton and colleagues (
6) were used to estimate the effect of postdischarge follow-up calls on the probability of readmissions. Specifically, we used a 45% reduction in readmissions as the upper estimate, a 0% reduction as the lower estimate, with a mean effect of 22.5% and a standard error (SE) of 11.48% (thus the 0% and 45% reductions would be 2 SEs from the mean). The range of 0%−45% is based on the two of the nine studies that examined an intervention that was purely telephone based. One study by Cedereke and colleagues (
17) that had 216 participants found no effect of follow-up calls on repeated suicide attempts, and the other study by Vaiva and colleagues (
12) that had 605 participants found a 45% reduction in repeat attempts of self-poisoning. This effect size implicitly incorporates the direct effect of follow-up contact on reducing readmissions—for example, by enhancing an individual’s social connectedness (
25)—and any indirect effect on reducing readmissions resulting from the fact that calls encourage receipt of postdischarge treatment. We did not examine these direct and indirect effects separately because, to our knowledge, there is no research that has clarified this relationship.
Cost of the intervention
The eight participating call centers reported the average time spent on follow-up calls, attempting follow-up calls, filling out call reports, and carrying out administrative work for the follow-up calls over the past 30 days. We multiplied the total time spent by the fully loaded hourly wage of the participating employees as reported by the call centers. Publicly available tax return forms of the call centers that function as nonprofit agencies (tax 990 forms) indicated that, on average, they spend 75.6% on employee costs and 24.4% on additional fixed costs. Using this information, we accounted for capital expenditures associated with the calls by inflating the total labor costs by 32%. We divided the total cost by the number of unique individuals called within 30 days to derive the average cost per person within 30 days of discharge. Because of the small sample of call centers, we also conducted a secondary analysis using the MarketScan databases to determine average payments for a similar procedure—an 11–20 minute assessment and monitoring telephone call provided by a nonphysician (CPT code 98967).
We assumed that providing postdischarge calls would increase the probability that the individual would obtain psychiatric treatment. Using the MarketScan databases, we determined the baseline percentage of patients who received follow-up treatment (that is, a nonemergency outpatient visit with a primary mental health or substance abuse diagnosis [
ICD-9-CM codes 291–293 and 295–314]) within seven days of discharge. Individuals were continuously enrolled in the databases during this time. We assumed that follow-up calls would have the greatest impact on reducing 30-day readmissions if the individuals entered treatment within seven days. In light of the sparse information on the effect of postdischarge follow-up calls on receipt of outpatient treatment, we assumed that the percentage of individuals receiving follow-up treatment in seven days as a result of the intervention could reach at least the same level as the percentage of those who, at baseline, received a mental health and substance abuse outpatient visit within 30 days of discharge. Essentially, we assumed that the effect of the follow-up call was to accelerate the time to a follow-up visit from 30 days to seven days. We assumed that payers would pay for one additional outpatient visit per discharge to help with the transition of care. This is consistent with the new transitional care management procedure codes implemented under Medicare that allow reimbursement for one face-to-face, postdischarge outpatient visit (
19). We used the MarketScan data to estimate the average amount paid for this visit.
Sensitivity analysis
To account for the uncertainty of the inputs, we conducted one-way and probabilistic sensitivity analyses. For the one-way sensitivity analysis, we varied each input and developed a tornado diagram to illustrate which inputs had the largest influence on the ROI. The ranges were set at the 95% confidence interval. We also used a probability distribution for each input and drew values randomly in a Monte Carlo simulation of 10,000 trials. For input probabilities, we used a beta distribution, which is bound between 0 and 1. For input costs, we used a gamma distribution, which is skewed right and commonly used to reflect the distribution of health care costs (
26). The probability distributions were matched to the mean and SE of the base case and hypothetical case values. The one-way sensitivity analysis, probabilistic sensitivity analysis, and all other ROI calculations were completed by using Microsoft Excel. [An Excel spreadsheet that allows users to change the values in the model and run additional sensitivity analyses is available as an online
data supplement to this article.]
Results
Inputs regarding savings
The ROI model inputs are listed in
Table 1. The 30-day mental or substance use disorder readmission rate after a suicide-related hospital stay was 9.1% for patients with commercial insurance and 10.4% for Medicaid beneficiaries. After a suicide-related emergency department visit, the readmission rate was 9.0% for those with commercial insurance and 7.4% for Medicaid beneficiaries. Commercial payers, on average, paid $7,936 for a mental or substance use disorder readmission among those with an initial suicide-related hospital stay and $7,542 among those with an initial emergency department visit; Medicaid, on average, paid $8,204 for those with an initial hospital stay and $9,176 for those with an initial emergency department visit.
Inputs regarding costs
The mean±SE cost per person to provide postdischarge follow-up calls was $56.07±$17.17 (range for the eight call centers, $11.38 to $139.64 per person). The call center that spent $139.64 per person reported that some of the services it provided over the telephone were similar to case management and, on average, the call center successfully contacted individuals five times in the first month after discharge. The other call centers averaged two calls per person in the 30 days after discharge. The services they provided included supportive listening, information and referrals, emotional support, risk assessment, safety planning, and crisis follow-up. The mean±SE length of the calls for the eight call centers was 13±2 minutes (range of means, five to 27 minutes).
The MarketScan databases indicated that the average payment for a similar procedure (CPT code 98967) was $57.26 for commercial insurance and $47.40 for Medicaid (similar to the cost of $56.07 estimated for the eight call centers).
For individuals discharged from a hospital, we found higher rates of baseline follow-up treatment among those covered by commercial insurance (52.4%) compared with those covered by Medicaid (37.7%) (
Table 1). We estimated that the postintervention follow-up treatment rates were 75.2% for those covered by commercial insurance and 61.4% for Medicaid beneficiaries. Average cost of an outpatient follow-up treatment visit was $161.29 for commercial insurance and $97.56 for Medicaid.
For individuals discharged from the emergency department, the baseline follow-up treatment rates were 38.8% for commercial insurance and 38.3% for Medicaid. The postintervention follow-up treatment rates were 61.7% for commercial insurance and 55.3% for Medicaid. The cost of an outpatient follow-up treatment visit was $149.41 for commercial insurance and $107.99 for Medicaid (
Table 1).
ROI estimate
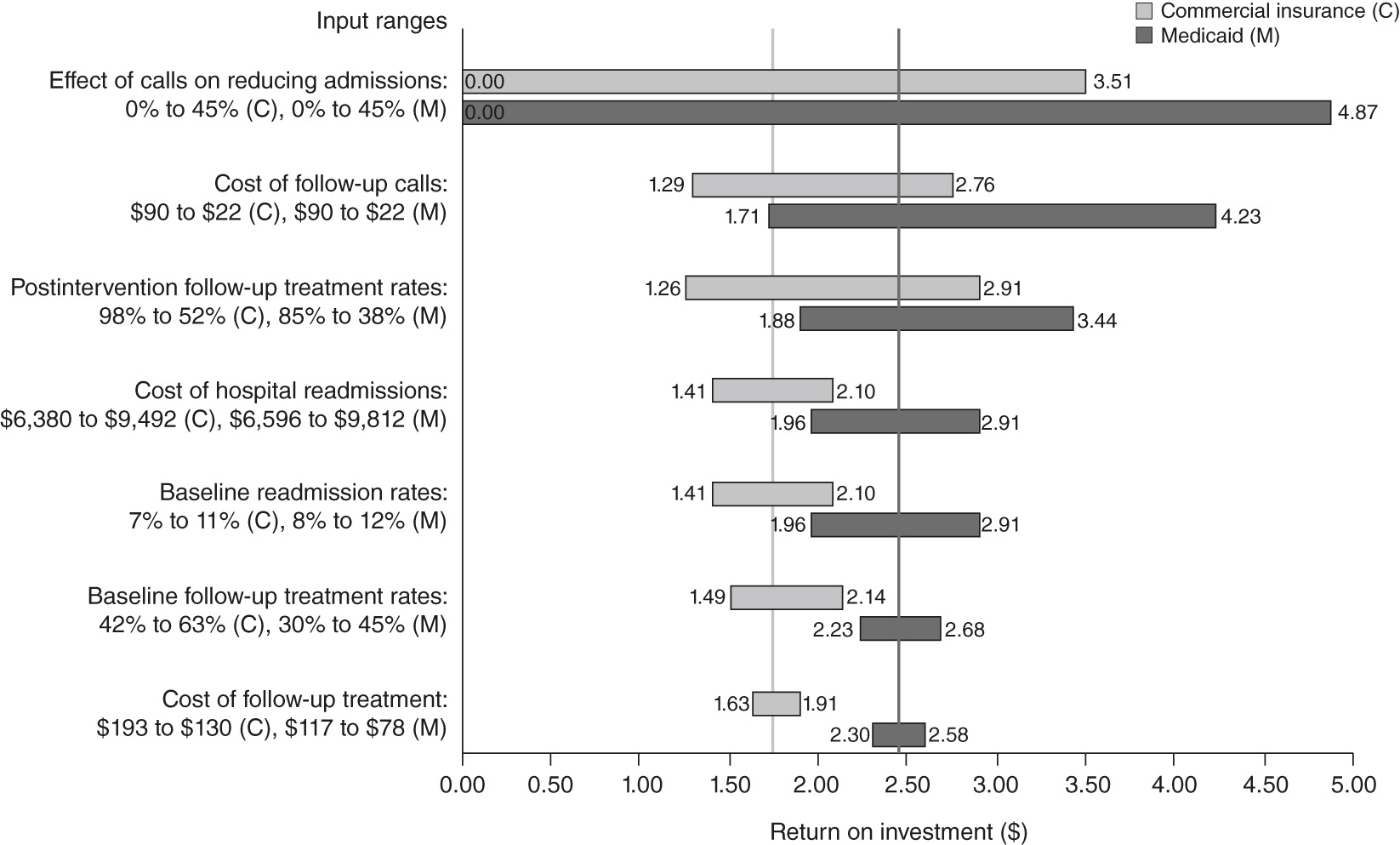
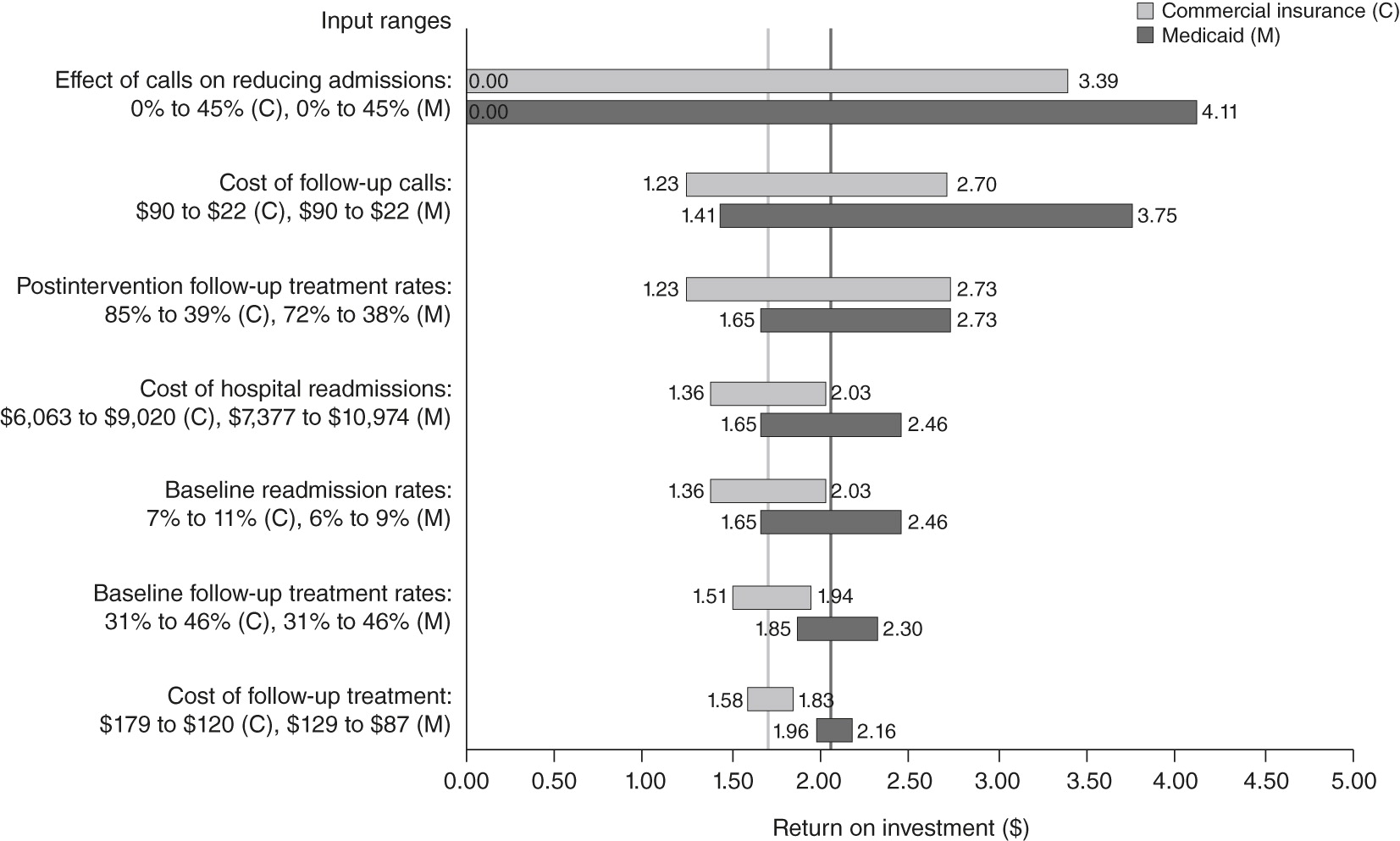
For patients discharged from a hospital, the ROI was $1.76 for commercial insurance and $2.43 for Medicaid. For those discharged from an emergency department, the ROI was $1.70 for commercial insurance and $2.05 for Medicaid. This is the return that payers would gain for every $1 invested in providing postdischarge follow-up calls to individuals who had a suicide-related hospital stay or emergency department visit (
Figure 2 and
Figure 3).
Sensitivity analysis
In the one-way sensitivity analysis, the uncertainty regarding the effect of postdischarge follow-up calls on reducing readmissions had the largest effect on the ROI (
Figure 2 and
Figure 3). For hospital discharges, the ROI varied from $0 to $3.51 for commercial insurance and $0 to $4.87 for Medicaid, depending on whether the effect of the intervention was nothing or was as large as a 45% reduction (
Figure 2). The ROI was estimated to be greater than $1 as long as the postdischarge follow-up calls could reduce the 30-day readmission rate by at least 12.9% for patients with commercial insurance and by at least 9.3% for Medicaid beneficiaries. For those discharged from emergency departments, the ROI could range from $0 to $3.39 for commercial insurance and $0 to $4.11 for Medicaid (
Figure 3). The ROI was estimated to be greater than $1 as long as the intervention could reduce readmissions by at least 13.3% for those with commercial insurance and at least 11.0% for Medicaid beneficiaries.
Variations in the cost of the intervention also had a large impact on the ROI. For example, if the cost per person of postdischarge follow-up calls was $22 (2 SEs below the mean), then the estimated ROI for patients discharged from the hospital was $2.76 for commercial insurance and $4.23 for Medicaid (
Figure 2). Increasing the intervention cost estimate to $90 per person reduced the ROI to $1.29 for commercial insurance and $1.71 for Medicaid (
Figure 2). The break-even point—where the mean ROI is $1—was when the cost of the intervention was $126 for commercial insurance and $169 for Medicaid for patients discharged from a hospital and $117 for commercial insurance and $134 for Medicaid for those discharged from an emergency department.
The percentage of people who received postdischarge treatment as a result of the intervention had the third greatest impact on the ROI. The ROI would be largest if postdischarge calls could reduce readmissions as efficiently as assumed, solely because of the effect of the postdischarge contact and with no change in treatment rates from baseline. For patients discharged from a hospital, the estimated ROI under this condition would be $2.91 for commercial insurance and $3.44 for Medicaid (
Figure 2). For those discharged an emergency department, the ROI would be $2.73 for commercial insurance and $2.73 for Medicaid (
Figure 3).
On the basis of the results of the probabilistic sensitivity analysis, we estimated that for hospital discharges there was a 77% probability that the ROI was greater than $1 for commercial insurance and an 88% probability that the ROI was greater than $1 for Medicaid. For emergency department discharges, we estimated that there was a 74% probability that the ROI was greater than $1 for commercial insurance and an 82% probability for Medicaid.
Discussion
The positive ROI found in this analysis supports a business case for providing postdischarge follow-up calls and for sustainable financing of this service. One method for providing these calls is through call centers. Large payers may establish their own call centers (similar to OptumHealth in San Diego), or they may support local call centers in collaboration with hospitals and emergency departments. The recent establishment of CPT codes for transition of care is an important foundation for strengthening the financial infrastructure to support postdischarge contact. New types of health care organizations (for example, accountable care organizations) and new payment incentives (for example, penalties for readmissions) may provide incentives for payers to offer these interventions.
This analysis showed that a key reason that postdischarge follow-up calls can be cost-effective is that they are a relatively inexpensive and effective intervention. However, we found variations in the length, frequency, and content of the calls and the types of professionals providing the calls. Our study was limited in not being able to examine the ROI for each different approach to postdischarge follow-up calls. There is some uncertainty about which ingredients in these different approaches contribute to decreased suicidal behavior. Some studies have argued that postdischarge follow-up calls and, more broadly, postdischarge follow-up contacts reduce suicidal behavior because they increase an individual’s social connectedness (
6,
8,
25). However, postdischarge follow-up calls may also reduce suicidal behavior by linking patients with needed services, which, in turn, have been shown effective in reducing suicide (
27–
30). The cost of effective postdischarge follow-up will be much higher and the ROI much lower if the primary active ingredient is follow-up treatment rather than just a contact. Future research needs to identify and estimate the effect of the active ingredients in postdischarge follow-up calls. It may be that some individuals will respond well to brief telephone calls as the only follow-up service, whereas others may need more intensive treatment. Research is also needed to clarify the most effective approaches, such as the length and frequency of calls, to leverage these active ingredients.
This study had several limitations. The first is the uncertainty in regard to the effect size of postdischarge follow-up calls on reducing readmissions. The second is that we were unable to examine potential differences in the ROI between individuals who express suicidal ideation and those who have made suicide attempts. The third limitation stems from the use of claims data, which may underestimate suicide-related admissions and emergency department visits because of undercoding (
20,
21). Finally, broadening the scope of our readmission statistic beyond readmissions with a suicide code to include any readmissions with a primary mental or substance use disorder diagnosis may have had an impact on our ROI calculation.
Conclusions
This study supports the business case for providing postdischarge follow-up calls to individuals with suicidal ideation or deliberate self-harm who are discharged from a hospital or emergency department. The findings may provide additional incentives for payers to develop financing and organizational structures to support postdischarge contact. More information is needed, however, to identify the key factors that make postdischarge follow-up calls effective, such as the relative importance of contact versus engagement in treatment.
Acknowledgments and disclosures
This research was funded by the Substance Abuse and Mental Health Services Administration (SAMHSA). The authors thank Manisha Vaze, M.S.S.W., of the National Suicide Prevention Lifeline. They also thank Safe Harbor Behavioral Health, Erie, Pennsylvania, and the following call centers: Austin Travis County Integral Care, Austin, Texas; Center for Community Resources, Butler, Pennsylvania; Contact Community Services, Syracuse, New York; Contact Crisis Line, Dallas, Texas; Crisis Center of Tampa Bay, Tampa Bay, Florida; FirstLink–North Dakota, Fargo, North Dakota; Pathways of Central Ohio, Newark, Ohio; and Volunteers of America Western Washington, Everett, Washington. The authors also thank James Wright, L.C.P.C., SAMHSA, and Dominic Hodgkin, Ph.D., Brandeis University. The authors thank the following employees or former employees of Truven Health Analytics: Greg Lenhart, M.S., Richele Benevent, M.S., Eva Witt, B.A., Karen Smoyer Tomic, Ph.D., Sabrina Malkani, M.P.H., Sasha Frankel, B.A., Leslie Preti, M.S., and Linda Lee, Ph.D. The views expressed in this article do not necessarily reflect those of SAMHSA or the U.S. Department of Health and Human Services.
The authors report no competing interests.