Persons with serious mental illness are disproportionately burdened by general medical conditions (
1,
2) and subsequent premature mortality (
3). Two out of every five veterans with serious mental illness experience substantial gaps in care (
4). Improving access to and continuity of health services may mitigate these risks (
3).
To address this disparity, the U.S. Department of Veterans Affairs (VA) tested the effectiveness of the Re-Engage outreach program, in which veterans with serious mental illness who had dropped out of care (defined as not seen by a VA provider for at least one year) were identified and encouraged to return to care (
5). Re-Engage consists of documentation of patients’ clinical status and of outreach to assess need for health care (
6); in a previous study, Re-Engage was associated with a greater proportion of veterans returning to VA care and with a sixfold reduction in mortality (
5).
Subsequently, in 2012 the VA approved a policy directive that authorized the national implementation of Re-Engage across VA facilities (
7). [A copy of this directive is available in an
online supplement.] VA program leaders sought to ensure that Re-Engage was effectively sustained nationally by local providers. VA program leaders sought to identify strategies to help providers implement Re-Engage and to ensure that this national program was effectively sustained by local providers. However, standardized implementation strategies (
7) have not been widely tested for their effectiveness. Taking advantage of the VA’s national implementation of Re-Engage, this study compared the effectiveness of a standard versus enhanced implementation strategy to promote the uptake of Re-Engage among sites not initially responding to six months of the standard implementation strategy.
Methods
The randomized controlled implementation intervention trial, described elsewhere (
7), was reviewed and approved by local VA institutional review boards. Sites not initially responding to an established implementation strategy (Replicating Effective Programs [REP]) were randomized (
8) at the VA regional network level to either continue with standard REP implementation of the intervention or receive an enhanced version of REP that included a facilitator to promote uptake of the Re-Engage intervention.
Using previously established population management techniques (
9), Re-Engage involved making initial queries of VA national administrative databases to identify veterans with a diagnosis of serious mental illness who had not been seen by a VA provider for a year or more. The intervention also required a mental health clinician to document veterans’ clinical status and to attempt to contact and link veterans to appropriate VA health care when needed (
5).
Investigators generated an initial list of veterans with either an inpatient or outpatient ICD-9-CM diagnosis for serious mental illness (schizophrenia, codes 295.0–295.9, or bipolar disorder, codes 296.0–296.1 or 296.4–296.89) recorded between fiscal year (FY) 2008 and FY 2011 who were last seen at a VA facility in the 50 United States, who remained alive throughout that period according to U.S. death records, and who as of FY 2011 had not received VA outpatient care for at least one year. The list was stratified by VA site where each patient was last seen, and the list was transmitted securely to a designated VA mental health clinician at that facility. These VA clinicians, known as local recovery coordinators, were identified by the VA national policy directive to implement the Re-Engage program. As licensed independent practitioners, a vast majority (96%) of local recovery coordinators were master’s-level social workers or doctoral-level psychologists, and they had the clinical expertise to implement the core components of the Re-Engage program, notably reviewing medical records, updating the patient’s clinical status in a Web-based registry, and assessing the veteran’s current medical and psychosocial needs in order to contact him or her and schedule needed appointments.
The primary focus of this study was to compare the two implementation strategies on the basis of improved uptake of Re-Engage (rather than on improvements in patient-level outcomes due to the Re-Engage program itself). The primary outcomes for this study were defined as the percentage of patients with an updated documentation of clinical status and percentage with an attempted contact by the provider. These measures represent core components of the Re-Engage program and were ascertained from the Web-based registry (
5,
9).
At the time the Re-Engage directive was implemented (March 2012), local recovery coordinators at all VA facilities (N=158 sites) in the United States were given the standard REP strategy, which included a toolkit, Web-based registry link, training in the Re-Engage program via conference calls, as-needed technical assistance to support implementation, and bimonthly progress reports on Re-Engage program implementation (
5). After six months of standard REP, 42% (N=70) of sites had achieved minimum program implementation, which was defined as initial effort to update clinical status for ≥80% patients in the Web-based registry. Sites that did not achieve minimum implementation (58%; N=88) were then randomized (September 1, 2012), with stratification by VA network level, to receive enhanced REP or continuation of standard REP.
Local recovery coordinators from sites randomized to enhanced REP were assigned to one of three doctoral-level facilitators, who provided coaching for six months. Providers from sites assigned to standard REP continued to have access to REP materials and could contact a separate technical assistant for Re-Engage program support but did not receive coaching from facilitators. All personnel who operationalized and provided the enhanced and standard REP implementation strategies, including facilitators and trainers, were located at one site. Facilitators were collaborators on a research project that was funded independently of national leadership, and they were not part of the local providers’ chain of supervision.
On implementing Re-Engage at a site, facilitators for enhanced REP provided coaching to local recovery coordinators via semistructured weekly calls (
9). During the calls, facilitators assessed site-level barriers to Re-Engage uptake, reviewed progress, provided support and encouragement, and developed action plans to resolve barriers to implementation. Facilitators also provided negotiation skills to help with securing time and resources from local leadership. Each facilitator recorded on a weekly log form the total time spent on facilitation activities, including attempted and completed calls with providers and meetings with national leadership to gain insight into local issues.
Descriptive statistics were used to compare the facilities achieving adequate reengagement after six months: percentage of patients with documentation of updated clinical status and percentage with at least one attempted contact within six months. Longitudinal repeated-measures analysis was used to compare site-level overall percentages between standard REP and enhanced REP groups, adding enhanced (versus standard) REP, time (in months), the enhanced REP × time interaction, facility size (overall number of unique patients at the site before site randomization), number of veterans on the site’s list for re-engagement, and whether the facility had an inpatient unit.
Results
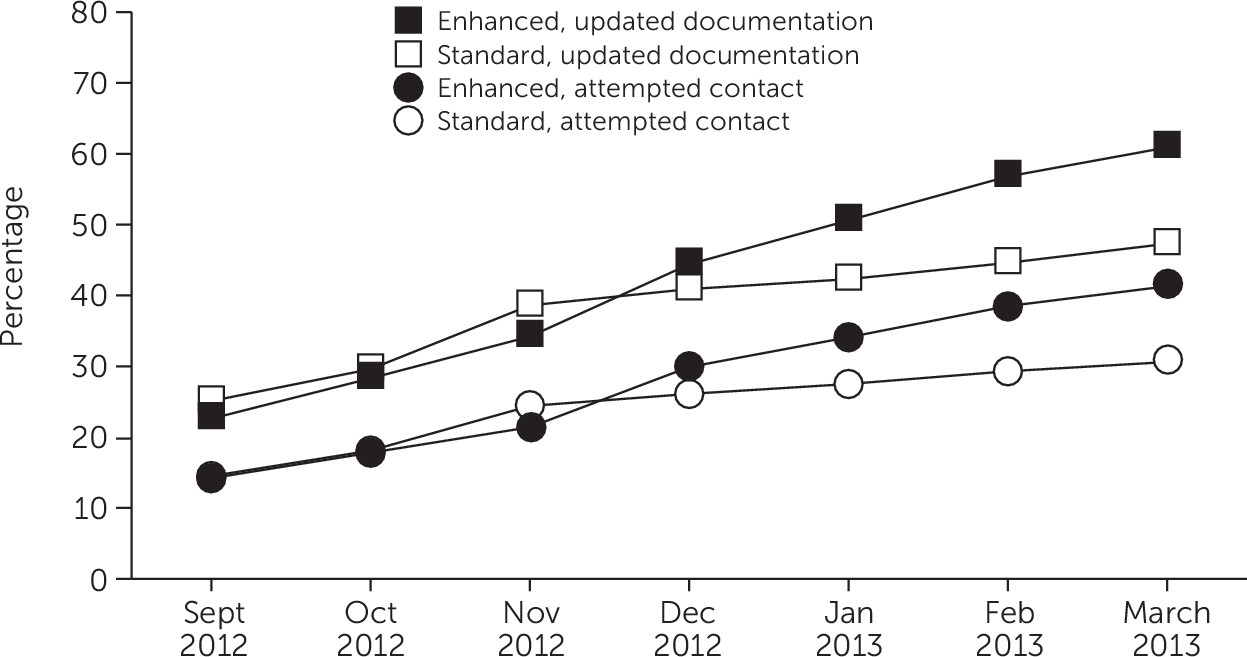
As of September 1, 2012, a total of 1,531 veterans had been lost to care in the 88 VA sites not initially responding to six months of standard REP, with a median of 17 veterans lost per site (range from four to 44 veterans). Six months later, sites receiving enhanced REP, compared with those receiving standard REP, had a greater percentage of veterans with updated documentation of clinical status (61% versus 47%; t=1.57, df=87, p=.01) and a greater percentage (N=579) with an attempted contact (41% versus 31%; t=1.58, df=87, p=.01) (
Figure 1). Results from the adjusted repeated-measures analysis indicated a greater rate of change among enhanced REP compared with standard REP sites in percentage of veterans with updated documentation (enhanced REP × time interaction, β=.03, t=3.17, df=462, p<.001) and attempted contact (enhanced REP × time interaction, β=.02, t=2.37, df=520, p=.01). The total amount of time all facilitators spent across the 39 sites during the six-month enhanced REP period was 284.6 hours, or a total of 7.3 hours per VA site for a six-month “dose” of facilitation support. Limiting the analyses to sites with ≥20 veterans who were lost to care produced similar results (data not shown).
Common barriers to Re-Engage program uptake addressed by facilitators included limited provider time to contact veterans because of multiple role responsibilities. Subsequently, facilitators provided guidance on delegating responsibilities. Providers also reported a loss in momentum when initial veteran contact efforts were unsuccessful, and facilitators encouraged providers to enlist peer specialists to help find veterans. Others reported a lack of appointment availability once veterans were contacted. Here, facilitators encouraged providers to meet with clinic leadership to secure scheduling assistance.
Discussion
In this implementation intervention trial, providers from sites randomized to receive added facilitation coaching compared with sites receiving a standard implementation strategy were more likely to implement an outreach program for veterans with serious mental illness who had dropped out of care. Few implementation strategies have been shown to improve the uptake of clinical programs, especially at the national level. Strategies such as enhanced REP can be useful to large health care organizations that strive to roll out evidence-based programs to improve access and outcomes for high-risk patients.
Assessing the effectiveness of enhanced REP among sites not initially responding to standard REP was important because not all sites needed a more intensive implementation strategy. This design also has the potential to inform the delivery of more cost-efficient implementation interventions (
8).
The priority to conduct a national rollout of the Re-Engage program precluded more intensive monitoring of program uptake or having facilitators make in-person site visits. Another study limitation was that the need to disseminate early findings mitigated the ability to wait for long-term patient-level outcomes data. Finally, there is a possibility that the effect of added facilitation resulted in more attention on the program. Nonetheless, Re-Engage was initiated as a national clinical mandate six months before facilitation was added across all sites, and all sites received reports on their implementation progress before randomization. Moreover, many local recovery coordinators saw facilitators as being in a position to ensure that Re-Engage was a priority to their local supervisors.