According to the 2010 U.S. Census, 19.3% of the U.S. population resides in rural areas, which places them at risk of poor detection and treatment of mental disorders (
1). Rural areas differ from urban areas in some significant ways that may explain this disparity, for example, longer travel distances, lack of colocation of mental health specialists in primary care settings, weak linkages to off-site mental health specialists, limited mental health insurance coverage, and higher levels of stigma (
2).
Collaborative care for depression has been shown to be highly effective (
3–
6) and cost-effective (
7–
10) in urban settings, but it is difficult to implement in federally designated mental health professional shortage areas (85% of rural counties) (
11). Collaborative care for depression can be adapted successfully for rural primary care settings by using telemedicine technologies (
12), but it is critical to also assess the cost-effectiveness of this approach.
Federally qualified health centers (FQHCs) are located in medically underserved areas and are a critical component of the health care safety net. In 2012, FQHCs served approximately 21 million patients, and this number could double by 2015 with the passage of the Patient Protection and Affordable Care Act (
13). Three-quarters of FQHC patients live in poverty, half live in rural areas, one-third is uninsured, and two-thirds are members of racial-ethnic minority groups. Mental health problems are the most commonly reported reasons for visits to FQHCs (
14), yet only 6.9% of encounters at FQHCs are with on-site mental health specialists (
15).
Two recent developments have focused FQHCs’ attention and resources on depression recognition and management. First, new federal standards require FQHCs to qualify as patient-centered medical homes (PCMHs) according to the National Committee for Quality Assurance. PCMH recognition requires team-based care that emphasizes care coordination. Second, the Centers for Medicare and Medicaid Services are expected to add depression to the list of clinical condition episodes included in the Bundled Payments for Care Improvement Initiative. The initiative will make clinics eligible to receive bundled payments for depression care.
A common decision facing clinics striving for PCMH recognition and preparing for bundled payments is whether to outsource care management services. To inform this decision, we conducted a cost-effectiveness analysis of two alternative approaches to providing depression care management in FQHCs. The on-site approach, practice-based collaborative care (PBCC), focused on improving depression outcomes by using local providers. The off-site approach, telemedicine-based collaborative care (TBCC), focused on utilizing off-site specialists to support local primary care (PC) providers.
Methods
Design Overview
This multisite, pragmatic randomized trial employed a comparative-effectiveness design (
16). Patients were randomly assigned to either TBCC or PBCC, both of which represented potentially feasible approaches to adapting the evidence-based collaborative depression care model for routine delivery in medically underserved areas. The intervention and evaluation methods are described in detail elsewhere (
12) and are summarized here. The base case or main analysis used Arkansas FQHC health care costs, and the secondary analysis used national cost estimates.
Setting and Participants
Six FQHCs were approached and five (83%) agreed to participate. Participating FQHCs employed between 1.3 and 9.7 full-time-equivalent PC physicians, served between 5,362 and 13,050 unique PC patients, and operated one to six clinics across multiple locations. None of the participating clinic locations had an on-site mental health specialist. From 2007 to 2009, a total of 19,285 patients were screened for depression, 2,863 (15%) patients screened positive (Patient Health Questionnaire–9 [PHQ-9] score ≥10), and 364 patients were enrolled. We excluded patients with schizophrenia, bipolar disorder, or acute suicide ideation. Patients (stratified by clinic) were randomly assigned to PBCC or TBCC. Blinded follow-up telephone interviews were completed for 318 (87%) of the 364 patients at six months, 287 (79%) at 12 months, and 283 (78%) at 18 months. This study was approved by the University of Arkansas for Medical Sciences (UAMS) Institutional Review Board. After complete description of the study to the patients, written informed consent was obtained.
Interventions
PBCC involved two types of providers: on-site PC providers and on-site nurse depression care managers (DCMs). Each clinic location employed a half-time DCM funded by the study. All DCMs received one day of training in depression care management, a care manager training manual, and access to a Web-based decision support system (
www.netdss.net) (
17). Encounters with a DCM were conducted either face to face or by telephone, depending on patient preference. The initial encounter with the DCM included PHQ-9 symptom monitoring, education and self-management behavioral activation, barrier assessment and resolution, and establishment of self-management goals, such as planning physical, rewarding, and social activities. Follow-up encounters included the monitoring of symptoms with the PHQ-9, medication adherence, side effects, and engagement in planned self-management activities. PBCC DCMs received no supervision from a mental health specialist. Patients could be referred to specialists at off-site locations, for example, community mental health centers. Progress notes were entered into the patients' paper medical record. Patients received the intervention for up to 12 months.
TBCC involved five types of providers: on-site PC providers and off-site DCM (a registered nurse), clinical pharmacist (Pharm.D.), psychologist (Ph.D.), and psychiatrist (M.D.). The off-site team was funded by the study and was located at UAMS. All encounters between DCMs and patients were conducted by telephone and followed the protocol described above. The DCM met weekly with the psychiatrist to discuss new patients and patients who were not responding to treatment and prepared progress notes containing stepped-care treatment recommendations. These notes were faxed to the FQHC for implementation by the PC providers. If the patient did not respond to the initial antidepressant, the off-site pharmacist conducted a medication history and provided medication management recommendations as needed. If the patient did not respond to two trials, a psychiatry consultation via interactive video was scheduled. At any time, patients had access to cognitive-behavioral therapy delivered via interactive video.
Depression Outcomes
It has been previously reported that the TBCC group experienced a significantly greater treatment response, significantly higher odds of remission, and significantly greater reductions in severity of depression over time compared with the PBCC group on the basis of the Symptom Checklist–20 (SCL-20) (
12).
Cost-Effectiveness Outcomes
Primary effectiveness outcomes for the analysis of cost-effectiveness were depression-free days and quality-adjusted life years (QALYs).
Depression-free days were calculated by using a formula originally developed by Lave and colleagues (
18) and adapted for use with the SCL-20 (
19). An SCL-20 score of .5 or less was considered depression free, a score of 1.7 or higher was considered fully symptomatic, and scores in between were assigned a linear proportional value. Sensitivity analyses using variations of these scores to define depression free (for example, .25 and .75) and fully symptomatic depression (for example, 1.5 and 2.0) resulted in minimal differences in number of depression-free days, so depression-free day scores using .5 and 1.7 thresholds are reported below.
QALYs were calculated in three ways. One method used a formula to convert incremental changes in depression-free days to QALYs (
20). We divided the difference in depression-free days over 18 months by 365 and then multiplied by the lower (.2) and upper (.4) bounds of the QALY increase associated with going from fully symptomatic to depression free (
20). In addition, previously published standard gamble utility weights were used to convert results of the Medical Outcomes Study 12-Item Short-Form Survey (SF-12) (
21) to QALYs. A third method used the Quality of Well-Being Scale (QWB) (
22) to calculate QALYs. Generic QALYs from the SF-12 and QWB are reported because generic QALYs are the recommended unit of effectiveness for the base case cost-effectiveness analysis (
23).
QALYs derived from the SF-12 used standard gamble preference weights (
21) that transformed SF-12 data into a preference-weighted index score that varied from .0 (death) to 1.0 (perfect health). Similarly, the QWB subscales represented preference-weighted scores that were subtracted from 1.0 (perfect health) to determine the QWB index score, which ranged from 0 (death) to 1.0 (perfect health) (
24).
Intervention costs and health care costs were collected by using a societal perspective (health care utilization and patient costs) and were adjusted to reflect 2009 dollars. The societal perspective was recommended by the U.S. Public Health Service Panel on Cost-Effectiveness in Health and Medicine. Fixed costs of the interventions included the cost of education materials for the DCM, DCM training, and interactive video equipment (TBCC only). There was one DCM for TBCC and six DCMs for PBCC. Costs of DCM training (eight hours) used 2009 Bureau of Labor Statistics median hourly wage for registered nurses plus 25% for fringe benefits (
www.bls.gov/oes/2009/may/oes_nat.htm#29-0000). Equipment costs included the purchase and installation of interactive video stations and routers, which depreciated in value over the course of the study. The annual depreciation rate was 18.33% (from the U.S. Bureau of Economic Analysis of depreciation of medical equipment) over four years (total duration of recruitment and intervention).
Variable costs of the interventions included the time spent by personnel delivering the intervention. Time costs for intervention personnel were estimated by using 2009 Bureau of Labor Statistics hourly wage data plus 25% for fringe benefits (
www.bls.gov/oes/2009/may/oes_nat.htm#29-0000). The DCM’s time was estimated by counting the number of encounters from chart review and estimating that an initial encounter would last 1.5 hours and follow-up encounters would last 1.0 hour (including time to reach the patient by phone, conduct the interview, and chart the encounter). For TBCC, variable intervention costs also included the time of the pharmacist, psychologist, and psychiatrist and monthly charges for the T1 line necessary for telemental health encounters. (A T1 line can carry about 192,000 bytes per second, roughly 60 times more data than a normal residential modem.) Intervention clinician time was estimated by the number of progress notes written by each provider and the time spent in team meetings. For the base case analysis, we assumed that 40% of T1 charges were attributable to TBCC, on the basis of reports in the literature that 40% of patients seen at a university-based telepsychiatry service had a primary depression diagnosis (
25). Sensitivity analyses varied T1-cost assumptions from 0% to 100%.
Health care costs were based on the Quality Improvement for Depression collaboration’s service utilization instrument, which measures service utilization on the basis of patients’ self-report. Patients are asked about service utilization for general medical problems and mental health problems (“personal or emotional problems such as feeling down or anxious, or for alcohol or drug problems”).
The base case analysis used FQHC costs and the secondary analysis used national costs. Outpatient FQHC visit costs were estimated by using the FQHC prospective payment system rates for Arkansas. Costs for outpatient visits to other facilities were estimated by using Arkansas Blue Cross Blue Shield data. Emergency room (ER) and inpatient costs were estimated by using data from the academic medical center and affiliated hospitals, including safety net providers, in the University HealthSystem Consortium Southern Region. Medication costs approximated the discounts provided to FQHCs by the 340B Drug Pricing Program by applying the average discount for the top ten medications prescribed in this study for general medical and mental (76% and 86%, respectively) conditions to the lowest average wholesale price listed in the Red Book. Patients’ time and mileage associated with health care utilization were collected from patients’ self-report. Patients’ time costs were estimated by using 2009 U.S. Census Bureau wage estimates related to age, gender, and education (for employed patients) or minimum wage ($7.25) (for unemployed patients). Patients’ mileage costs were estimated by using the 2009 General Services Administration reimbursement rate of 59 cents per mile.
For the secondary analysis, health care costs were estimated from LifeLink Health Plan Claims Data, which comprise data from 70 million enrollees from 80 managed care organizations and are nationally representative of the commercially insured U.S. population. Per diem costs for inpatient treatment of general medical conditions were estimated from the median allowed per diem cost of the top ten most frequent ICD-9 diagnoses other than mental health diagnoses. Per diem costs for inpatient treatment of mental health conditions and ER costs for general medical and mental health visits were estimated from their respective Clinical Classifications Software codes. Outpatient costs were estimated on the basis of their respective CPT codes. Medication costs were estimated by using the Red Book lowest average wholesale price.
Incremental cost-effectiveness ratios (ICERs) are the ratio of the difference in total costs between TBCC and PBCC divided by the difference in effectiveness (depression-free days or QALYs), as shown in the following formula: [cost (TBCC) – cost (PBCC)]/[QALY (TBCC) – QALY (PBCC)]. The base case analysis included the SF-12–derived QALYs and outpatient, ER, pharmacy, patient (travel and time), intervention, and 40% of monthly T1 costs. Sensitivity analyses included 0% or 100% of the T1 costs, QALYs derived from conversion of depression-free days (using the lower [.2] and upper [.4] bounds of the QALY increase) and the QWB, and mental health inpatient costs. Secondary analyses included cost estimates from the nationally representative LifeLink claims data.
Case Mix Variables
At baseline, information about sociodemographic and clinical case mix factors were collected by using the Depression Outcomes Module (
26), the Mini International Neuropsychiatric Interview (
27), the Duke Social Support and Stress Scale (
28), the Quality Improvement for Depression Treatment Acceptability Scale (
5), and the Depression Beliefs Inventory (
29). Zip codes were used to categorize patients’ residence as rural or urban according to Rural-Urban Commuting Area codes.
Statistical Analysis
Patients were the unit of the intent-to-treat analysis. Only patients with at least one research follow-up visit were included in the analyses. All models specified clinic as a random effect to control for intraclass correlation. Data were missing for four cost variables and two demographic variables (.3% each) and for the SF-12 at 18 months (15.7%). Variables with missing data were imputed by using multiple imputation methods. Because of the large number of available covariates, only those with significant differences between TBCC and PBCC (p<.20) were included in multivariate analyses. After model specification was finalized, prebaseline health care utilization costs were added to cost models as a covariate.
The depression-free day and cost outcomes were nonnormally distributed, so generalized linear models (GLMs) were used. The GLMs with a gamma distribution and identity link were the best fit for the cost data. The depression-free day and QALY data were normally distributed, so the normal distribution with identity link was used. To determine the incremental effect of treatment on QALYs, we used the regression coefficient for the intervention variable.
We used a nonparametric bootstrap-with-replacement method and 1,000 replications to generate an empirical joint distribution of incremental costs and QALYs (
30) and acceptability curves representing the probability of falling below cost-effectiveness ratio thresholds ranging from $0 to $100,000 per QALY (
31).
Results
In general, study patients were middle-aged, low-income, Caucasian women with moderate depression who were unemployed and uninsured (
Table 1). The only statistically significant differences between the intervention groups was a higher level of perceived barriers to depression treatment in the TBCC group (4.0) compared with the PBCC group (3.4) (p=.01).
Although there were no statistically significant group differences in terms of health care costs, the total cost per patient was significantly greater for TBCC than for PBCC because of the higher fixed and variable costs of TBCC (
Table 2). The unadjusted average incremental intervention cost (fixed plus variable intervention cost difference between TBCC and PBCC) was $1,132 ($376+$756). For the base case analysis, the adjusted total cost was significantly greater for TBCC compared with PBCC (β=1,146, 95% confidence interval [CI]=396–1,897, p=.003). The adjusted incremental cost ranged from $794 (CI=56–1,533, p=.03) for 0% monthly charges for a T1 line to $1,663 (CI=884–2,442, p<.001) for 100% monthly charges for a T1 line.
The adjusted incremental effectiveness on depression-free days was significant (β=109.6, CI=79.7–139.5, p<.001), as was the incremental effectiveness on depression-free day QALYs at both the lower (.2) and upper (.4) bounds of QALY increases associated with improving from fully symptomatic to depression free (β=.04, CI=.03–.05, and β=.078, CI=.06–.10, respectively; both p values <.001). The adjusted incremental effectiveness for generic QALYs was also significant (SF-12 QALY, β=.04, CI=.02–.07, p=.003; QWB QALY, β=.04, CI=.01–.07, p=.01).
When mental health inpatient costs were excluded, the bootstrapped mean ICER calculated by using FQHC costs and depression-free days was $10.75 per depression-free day; in the sensitivity analyses, it ranged from $7.49 (0% of T1 charges) to $15.49 (100% of T1 charges). The mean ICER calculated by using FQHC costs and SF-12 QALYs was $33,217 per QALY (
Table 3). The sensitivity analyses for the QALY estimates ranged from $14,714 (depression-free days and upper [.4] bound of the QALY increase) to $35,762 (QWB) per QALY. The T1-charge sensitivity analyses that used FQHC costs and SF-12 QALYs ranged from $22,548 per QALY (0% of T1 charges) to $48,789 per QALY (100% of T1 charges). Adding inpatient mental health costs to the SF-12 QALY base case analysis resulted in an ICER of $36,033 per QALY.
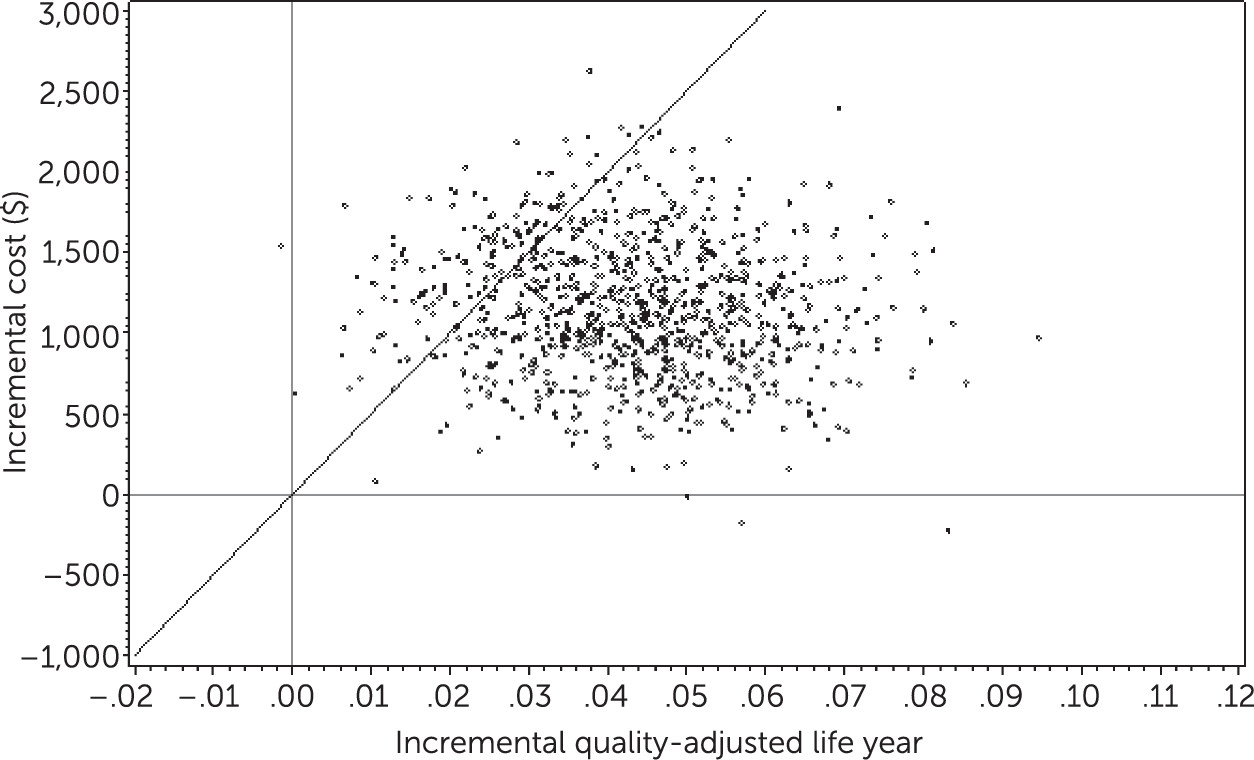
Figure 1 depicts a scatter plot analysis of incremental costs associated with increased QALYs derived from the SF-12.
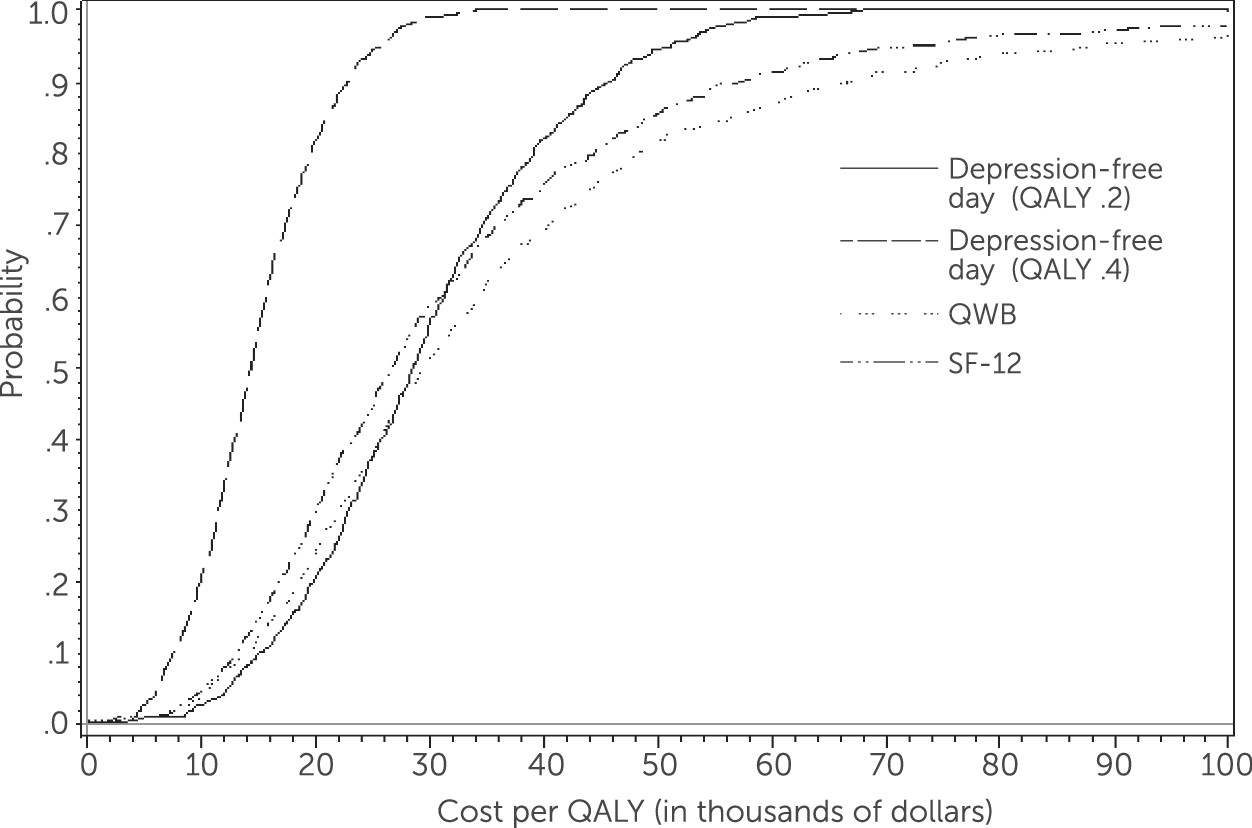
Figure 2 depicts an acceptability curve illustrating the probability of falling below cost-effectiveness ratio thresholds for QALYs associated with a range of costs.
When mental health inpatient costs were excluded, the bootstrapped mean ICER calculated by using national costs and depression-free days was $8.46 per depression-free day. The mean ICER calculated by using national costs and QALYs derived from the SF-12 was $25,728 per QALY. The sensitivity analyses for the QALY estimates ranged from $11,579 (depression-free day and upper [.4] bound of the QALY increase) to $28,017 (QWB) per QALY. Adding inpatient mental health costs to the analysis of national costs and SF-12–derived QALYs resulted in costs per QALY of $28,126.
Discussion
For primary care clinics lacking on-site mental health resources, there are increasing calls for collaborative care models in which off-site specialists support primary care providers by using telemedicine technologies (
32). To our knowledge, this is the first cost-effectiveness analysis to compare the value of outsourced TBCC with PBCC. The adjusted incremental cost (base case) of TBCC was $1,146, which is consistent with the incremental cost reported for other collaborative care interventions for depression ($389 to $1,772 per capita adjusted to 2009 dollars) (
7,
10,
19,
20,
33). Televideo equipment and T1-line charges accounted for 50% of the per capita direct costs of TBCC. However, results clearly demonstrated that TBCC was both more effective and more cost-effective compared with PBCC. The incremental cost-effectiveness of TBCC was $10.78 per depression-free day, which is less than what depressed patients report being willing to pay for an additional depression-free day ($14.40, adjusted to 2009 dollars) (
34). Other studies that have estimated the cost-effectiveness of collaborative care versus usual care for depression have reported ICERs ranging from $3.64 to $85.54 per depression-free day (2009 dollars) (
20,
35).
The mean ICERs for all methods of calculating QALYs were below the commonly used threshold of $50,000 per QALY for intervention adoption. The cost-effectiveness ratios calculated by using depression-free days and the upper (.4) bound of the QALY increase (which is the most commonly reported QALY measure for collaborative care interventions for depression) were less than $20,000 per QALY, which is considered the threshold for recommending immediate adoption (
23). In other studies, estimates of mean ICERs for collaborative care versus usual care for depression ranged from $3,325 to $99,335 per depression-free-day QALY, adjusted to 2009 dollars (
20,
35).
The TBCC intervention is a cost-effective model for delivering accessible and high-quality depression care to settings lacking on-site mental health resources. Thus, TBCC presents a viable option for organizations weighing whether to “make or buy” depression care management in order to achieve PCMH recognition. Telemedicine capability in primary care clinics is increasing within (
http://aims.uw.edu) and outside (
www.accesspsych.com) university research programs. Estimates from previous collaborative-care interventions indicate that approximately one DCM is needed for every 10,000 primary care patients and that TBCC could feasibly cover more than one site (
36). Adaptations of TBCC to enhance value and sustainability could be tested within specific settings and will be required within the changing health care environment (
37).
This study had the following limitations. Electronic health record systems were not in place at the FQHCs during this study, which limits the generalizability of the findings. However, electronic health records would likely improve communication between the TBCC intervention team and FQHC providers. The demographic characteristics of FQHC patients (typically poor, rural, and uninsured members of racial-ethnic minority groups) differ from private sector patients, which limited the generalizability of the findings to the private sector.
Conclusions
This pragmatic comparative cost-effectiveness study provides evidence to support the cost-effectiveness of TBCC in medically underserved areas. These results can help FQHCs and other health care delivery systems decide whether to provide on-site versus off-site depression care management as they work toward achieving PCMH recognition, utilize value-based purchasing, and prepare for bundled depression care payments.
Acknowledgments
The authors gratefully acknowledge the patients and staff at the Boston Mountain Rural Health Center, Inc., Community Clinic Northwest Arkansas, Corning Area Healthcare, Inc., East Arkansas Family Health Center, Inc., and Jefferson Comprehensive Care Systems, Inc., as well as staff at the Community Health Centers for Arkansas, Inc. They also acknowledge the important contributions of project staff, including Amanda Davis, M.A., Loretta Ducker, R.N., Debbie Hodges, Choi Lai, M.S., Michael McCarther, B.S., Camille Mack, B.S., Jennifer Stephens, and Vera Tate, M.D., and acknowledge Brad Martin, Pharm.D., Ph.D., and Anand Shewale, B.Pharm., M.S., for providing access to LifeLink data.