Posttraumatic stress disorder (PTSD) is a psychiatric disorder that arises from exposure to traumatic life events and is defined by symptoms of re-experiencing the traumatic event, hyperarousal, and avoidance of stimuli associated with the trauma (
1). In the general population, PTSD has been found to be associated with an increased likelihood of endorsing one or more psychotic symptoms, particularly positive psychotic symptoms (delusions and visual and auditory hallucinations), after adjustment for sociodemographic characteristics and psychiatric and general medical comorbidity (
2). PTSD in the general population is also linked to poorer general health, morbidity, and increased likelihood of seeking medical services and more intensive services (
3–
7). Population-based studies documenting the health care costs of individuals with PTSD in general health care settings have found increased costs for those scoring ≥45 points on the PTSD Checklist (PCL), indicating probable PTSD, compared with those scoring below 45 (
8).
For people with severe mental illness, PTSD is associated with other complicating conditions, such as substance abuse, increased use of general medical services, and impaired social functioning (
9–
12). Over the past two decades, much research interest has focused on trauma exposure and PTSD and their interactions with serious mental illnesses such as schizophrenia, bipolar disorder, and severe major depression (
13,
14). Whereas rates of trauma exposure in the general population are reported to be around 50%, and lifetime rates of PTSD are reported between 8% and 13% (
15–
19), the rates found among people with severe mental illness are much higher. Reported trauma exposure rates are as high as 98% in this population (
20–
25), and reported PTSD rates vary between 19% and 43% (
10,
11,
14,
20,
26–
28).
Although many studies have reported higher rates of trauma exposure and PTSD among persons with severe mental illness, documentation of PTSD in medical records remains remarkably low (
29,
30). In two studies, the rate of chart diagnosis was 2% (
20,
27); in another, 5% (
31). The source of the discrepancy between what research diagnoses reveal and what clinicians document in the chart is not clear. One suggested explanation is that the clinical chart diagnosis is driven by reimbursement needs, and because PTSD is not considered a major mental illness, it is not reimbursable at the same rate as schizophrenia, bipolar disorder, or major depression and therefore is not reliably recorded (
32). Another possible explanation for the gap is the inadequate assessment of trauma exposure and PTSD and the lack of evidence-based treatment for this population in typical clinical settings (
32).
Whatever the cause, the screening, diagnosis, and treatment of PTSD in public mental health centers remain at a suboptimal level (
32), and PTSD is mostly overlooked and untreated (
9,
28). After several decades of research with this population, what is still missing is a clear understanding of the interaction between trauma exposure, PTSD, and comorbid severe mental illness. Mueser and colleagues (
33) proposed a model in 2002 that posited PTSD as mediating negative effects and outcomes of severe mental illness. Yet in their conclusion, they stated:
Although exposure to trauma in persons with severe mental illness is related to more severe psychiatric symptoms, substance abuse and higher use of acute care treatment services, little is understood about how these relationships are mediated. [italics added for emphasis]
Little is known about the stability of PTSD in this population, its demographic and clinical correlates and the interaction between PTSD, clinical status and service utilization. [italics added for emphasis]
Fasoli and colleagues (
34) addressed the issue of predicting mental health service utilization on the basis of Andersen and Newman’s (
35) model, where the amount and intensity of service use are affected by predisposing characteristics, such as age, gender, and race; enabling resources, such as easy access to and financial responsibility for care; and clinical need indicators, such as symptom severity. Among other factors, worse self-reported mental health on the Behavior and Symptom Identification Scale (BASIS-24) (
36), indicating need, predicted more use of outpatient and residential services but not inpatient care. To the extent that PTSD is associated with more severe psychiatric symptoms (
2), we planned to explore whether high risk of PTSD (even without a chart diagnosis) affects the service use of people with severe mental illness in a service environment.
The Study and Primary Hypotheses
In 2007, as part of a study that was funded by the National Institute of Mental Health for cognitive-behavioral therapy (CBT) for PTSD, a PTSD screening tool was introduced at Rutgers University Behavioral Health Care (RUBHC) (
31) to identify patients who, in addition to having severe mental illness, were likely to have a PTSD diagnosis. Clinicians were trained in the administration and scoring of the tool. Subsequently, the PTSD screening tool became part of the routine intake assessment in both outpatient and partial-hospitalization programs at RUBHC.
Using the routine PTSD screening data in tandem with other data in RUBHC’s electronic medical record (EMR), we aimed to determine whether the finding in the general population that PTSD is associated with more severe psychiatric symptoms is confirmed in a sample of individuals with severe mental illness in a community-based treatment setting, to evaluate whether PTSD is associated with a lower rate of engagement in psychiatric treatment, and to evaluate whether PTSD is associated with increased service utilization, especially high-intensity services (that is, inpatient and partial-hospitalization services).
In addition, because recent evidence suggests that PTSD may be more common among African Americans but is frequently not recognized clinically (
36–
38), we examined rates of PTSD by race. Furthermore, it has been suggested that the well-documented higher rate of schizophrenia and psychosis in clinical charts of African Americans, which is not found in population surveys of African Americans (
36), may be related to the lower recognition of PTSD in clinical settings (
2,
37–
40). As a consequence, some PTSD symptoms, such as flashbacks, dissociative states, and hyperarousal, are misinterpreted as indicators of schizophrenia rather than PTSD. Therefore, we also examined the interrelationships between self-reported PTSD symptoms, self-reported psychotic symptoms, and race.
We hypothesized that PTSD would be associated with greater impairment in self-reported functioning and more severe symptoms after we controlled for demographic and clinical variables, such as diagnosis, race-ethnicity, and gender. Additional hypotheses were that clients who screened positive for PTSD would show more difficulty engaging in services, demonstrated by higher no-show rates, and show greater use of high-intensity services, including inpatient days, acute or partial-hospitalization program days, and emergency visits, compared with clients without positive screens.
Methods
Study Site
The study site was RUBHC, one of the largest mental health service organizations in New Jersey and providing services annually to approximately 11,000 individuals with severe mental illness. Available programs include an inpatient unit, outpatient services, and partial-hospitalization, screening/emergency, and mobile outreach programs and other community-based services (such as supportive housing, intensive case management, and family support services).
The data used in this study were taken from the administrative and clinical databases of RUBHC. No new data were directly collected from clients. The study received institutional review board approval from Rutgers University.
Sample
The sample included all active clients at RUBHC between January 2007 and November 2010 who were screened for PTSD after the implementation of the CBT study (
31) and for whom there were electronic data from the Behavior and Symptom Identification Scale (BASIS-24 [
41]), another routine screening tool used at RUBHC. We have excluded from our analysis the 201 clients who participated in the CBT study because they received the special treatment that the study was focused on and inclusion would have inflated the service use data for our analysis. Demographic and clinical data as well as the BASIS-24 results and the PTSD screening scores were available from the RUBHC EMRs. Service data included services provided a year before and a year after the screening date. However, because there was no difference between the two periods, the entire service data set was used in further analyses.
Measures
The civilian version of the PCL, developed by Blanchard and colleagues (
42), was used to screen and identify cases of probable PTSD diagnosis and to assess PTSD symptom severity. The PCL includes one question for each
DSM-IV-TR PTSD symptom, requiring the respondent to rate the severity of each symptom over the past month on a 5-point Likert scale (range 17–85). The PCL has good test-retest reliability and convergent validity for people with severe mental illness (
43,
44). A total score ≥45 was used to identify cases of probable PTSD during the initial screening (
42).
The BASIS-24 is a 24-item self-report scale of functioning and symptoms (
41). The scale is routinely used at RUBHC for all clients at intake. In outpatient and partial-hospitalization programs it is used midtreatment, and in acute care inpatient programs it is also used at discharge.
Statistical Analysis
We sought to determine the impact of probable PTSD on service use, no-show rates (a measure of low treatment engagement), and psychiatric symptoms and functioning (BASIS-24 scores). The data were analyzed with SAS/PC software. We compared two groups of clients: one group with PTSD screening scores ≥45, the other with scores <45. Statistics used depended on the nature of the dependent variables in question; for example, Fisher’s exact test was used for categorical data, and t tests were used for continuous data. For more complicated models examining the effect of probable PTSD on dependent variables of interest (service use, for example), multiple regression was used to control for demographic covariates (including gender, race-ethnicity, and age).
Results
Of the 1,834 clients with PTSD screening, 906 (49%) of the clients scored ≥45, and 928 (51%) scored below the cutoff of 45.
Table 1 presents the demographic characteristics of the sample. In the probable PTSD group, although there were more women in the sample (1,048 versus 786) the percentage of probable PTSD was higher for men (56% versus 45%). The racial-ethnic distributions were similar for African Americans and European Americans; however, the rate of PTSD was lower among Hispanics compared with these groups. The diagnostic distributions indicated that the group with schizophrenia and other psychoses had less probable PTSD (36% versus 64%), but the reverse was true for groups with major depression, bipolar disorder, or other psychiatric diagnoses.
The most striking finding about service use and no-shows was that partial-hospitalization services were used less by the group with probable PTSD than by those who probably did not have PTSD (
Table 2). No other service use differences between groups were significant. Those with probable PTSD had significantly more no-show appointments for outpatient and partial-hospitalization services than did the group without probable PTSD.
Although not shown in
Table 2, diagnosis and race-ethnicity also had significant main effects; appointment no-shows were more frequent among African Americans and European Americans with probable PTSD compared with those from the same racial-ethnic groups without probable PTSD. Persons in any of the three most severe diagnostic groupings (schizophrenia, major depression, and bipolar disorder) had higher no-show rates if they also were classified as probably having PTSD.
Tables 3 and
4 present the results of six regression analyses, one for each of the six BASIS-24 domain scores, with each regression examining probable PTSD as a predictor and controlling for diagnosis, race-ethnicity, age, and gender. Bonferonni corrections were used to account for multiple tests.
Table 3 shows that PTSD was associated with increased symptomatology across all six domains of the BASIS-24, with controls for clinical and demographic variables. Significant main effects were also found for the interpersonal, emotional lability, and psychosis subscales (p<.001 for all). In addition, African Americans reported more severe symptoms than European Americans, and women reported more emotional lability and depression than men did (p<.001; data not shown in table). There were no significant effects for age.
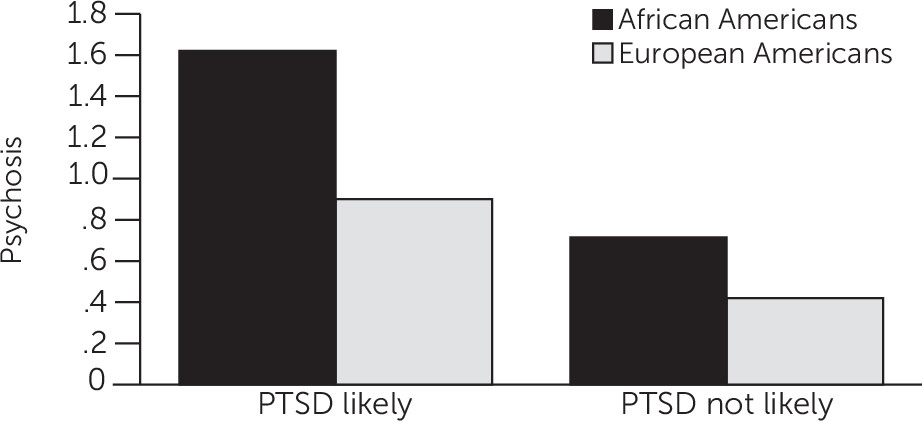
Table 4 presents the results of the same six regression analyses described above for the PTSD × race-ethnicity interaction. This interaction was statistically significant in three domains (depression, emotional lability, and psychosis). The most robust effect was associated with psychosis. Comparisons of the four means constituting the PTSD × race-ethnicity interaction (p<.001) indicated that self-reported psychosis was significantly higher among African Americans with probable PTSD compared with African Americans without probable PTSD and compared with European Americans regardless of their PTSD group (
Figure 1).
Discussion
The first hypothesis tested in this study—that clients who screen as probably having PTSD would have more severe psychiatric symptoms than those who screen as probably not having PTSD—was confirmed. Consistent with existing literature (
20), in this study, clients with probable PTSD, compared with those without probable PTSD and with controls for clinical and demographic variables, reported more severe psychiatric symptoms, as well as more impaired functioning, across all six domains of the BASIS-24. Compared with clients without probable PTSD, those with probable PTSD reported more interpersonal problems, more substance abuse, more depression, more self-harm, increased mood instability, and elevated psychosis.
The second hypothesis, regarding engagement in services, as measured by the frequency of no-show events, also was supported by the data. Clients with probable PTSD were more likely to miss appointments and thus not receive recommended treatment compared with those without probable PTSD.
Finally, our third hypothesis—that the probable PTSD group would have increased use of high-intensity services, including inpatient days, acute or partial-hospitalization program days, and emergency visits—was not supported by the data. This hypothesis was based on the assumption that people with significant trauma would be more impaired and therefore require more services, particularly the more intensive services (such as inpatient or partial-hospitalization services). The results of the study showed, however, that the probable PTSD group used slightly more outpatient services but significantly fewer partial-hospitalization and inpatient days. It is not clear whether this finding was due to the clients’ own choice or the inability of the system to provide services that are appropriate for clients with trauma and PTSD in addition to their serious mental illness. The reduced level of services overall may replicate earlier findings that documented lack of appropriate trauma-informed services (
9).
The interaction between race-ethnicity, probable PTSD, and the symptom domains of the BASIS-24, especially the psychosis domain, was intriguing. African Americans with co-occurring probable PTSD showed more self-reported psychosis symptoms than did African Americans without probable PTSD and showed more psychosis than European Americans, regardless of the PTSD status of the latter. This interaction was evident even though there was also a main effect of race-ethnicity alone on the psychosis domain score. A smaller interaction effect was evident for the emotional lability and depression domains.
These findings suggest that self-reported or clinician-documented psychotic symptoms may be elevated for African Americans with comorbid PTSD, compared with European Americans regardless of PTSD status and with African Americans without PTSD. The implications for the well-documented higher rates of diagnosis of psychosis (
36) among African Americans are intriguing and call for additional focused research.
Conclusions
In summary, the study showed the value of screening for PTSD and traumatic events in a general psychiatric population, particularly because chart diagnoses of PTSD are rarely documented in the EMR, most likely because services for PTSD are reimbursed at a lower level than those for the major mental illnesses. The study also suggested that the high rates of diagnosis of psychosis among African Americans may be associated with an increased risk for PTSD. Because a subset of PTSD symptoms overlaps with psychotic symptoms, the study suggests the importance of carefully assessing traumatic history and symptoms before making a diagnosis of psychotic disorder, particularly schizophrenia.