Collaborative care programs in primary care are effective for a wide variety of mental health conditions (
1,
2). The benefits of collaborative care in terms of efficiency have been inconclusive until recently (
3). In randomized trials investigating the effectiveness and efficiency of collaborative care, the follow-up period is usually limited to the period of active treatment (mean±SD=13.7±9.8 months, range of three to 36 months [
1]). Furthermore, collaborative care has been compared with various types of usual care, yielding different results for comparative effectiveness and efficiency. Most studies have compared collaborative care programs with usual care by a primary care physician. Compared with regular treatment by a primary care physician, collaborative care is often a more intensive treatment and more expensive (
4). Only a few studies have compared collaborative care with usual specialized mental health care for patients with common mental disorders. In a study with elderly primary care patients, a group that is said to underutilize mental health services, collaborative care was associated with a greater number of mental health contacts compared with usual care (
5). This finding was, however, accompanied by substantially greater treatment attendance at the collaborative care setting.
Because most of the evidence about treatment efficiency is limited to a relatively short follow-up period, little is known about utilization and costs over the longer term. There is preliminary evidence that the additional costs associated with provision of enhanced collaborative care for depressed patients compared with provision of usual care by a primary care provider disappear over time (
6) and that collaborative care may even result in lower total health care costs (
7). It is especially important to assess long-term mental health care utilization of collaborative care compared with specialized care because collaborative care has recently been promoted as a more cost-saving alternative than specialized mental health care. It may be that that efficiency gains resulting from collaborative care in the short term are lost over the longer term because of diminishing effectiveness of treatment and the need for greater treatment intensity.
This study analyzed data from patients formerly enrolled in a cluster-randomized controlled trial that compared the effectiveness and utilization of collaborative mental health care and usual care in the specialized mental health care setting (
8). The hypothesis of that study was that referral to and treatment in a collaborative care program (CCP) would lead to fewer contacts with a mental health care professional than referral to and treatment in specialized mental health care (usual care). After the trial’s one-year follow-up period, we were able to confirm this hypothesis. The mean annual difference in the number of mental health care contacts was 6.5 in favor of the CCP, with no significant differences in patient outcome. The mean difference in mental health care costs was €563, also in favor of the CCP. We also found, however, that 32% of the total sample (28% in the CCP and 46% in usual care) did not terminate treatment within the one-year follow-up period. Extending the follow-up period to the point at which all patients had terminated treatment may have yielded different results.
In the study reported here, we used post-hoc analyses to investigate long-term use of mental health care in the CCP and in usual care. Therefore, we extended the follow-up term to five years after referral. More specifically, we investigated whether the one-year differences between CCP and usual care in mental health care contacts, total treatment duration, proportion of patients receiving a new treatment, and time to a new treatment episode persisted over a five-year follow-up period.
Methods
Participants
We conducted a retrospective analysis of mental health care utilization among patients included in a cluster-randomized controlled trial that was conducted from 2003 until 2005 (
8). For the trial, 27 general practitioners (GPs) were randomly assigned to either the CCP or the usual-care condition (specialized mental health care). Most of the GP practices in the region were not eligible for randomization, because they already had a collaborative care mental health professional working in their practice. A total of 165 patients were included in the trial: 102 patients were referred to and treated in the CCP, and 63 were referred to usual care (off-site specialized mental health care) if indicated. All patients were followed up for one year after referral by their GP. Ten patients dropped out of the study during the trial phase. Only one of these patients was also excluded from the post-hoc analyses because we lacked utilization data. Informed consent and institutional review board approval were obtained for the trial.
Interventions
In the CCP, GPs gave a mental health professional a position in their practice. The mental health professional was able to offer treatment based on a short-term model (
9) to patients with nonacute common mental disorders, with a maximum of five appointments. If indicated on the basis of severity or complexity of symptoms, patients could be referred to specialized mental health care for more intensive treatment after the initial clinical assessment with the mental health professional or at a later date. For patients assigned to the usual-care condition, the GP continued his or her regular way of treating and referring the patient to specialized mental health care, usually to specialized mental health care.
Measures
For the analyses, data about utilization, including termination, were extracted from the electronic health record of the local mental health care institution in The Hague and surrounding area that offered both the CCP and specialized mental health care. Mental health care use by study participants within five years after the date of referral by their GP was documented. The total time frame of the follow-up period was seven years (2003–2009).
Mental health care contacts encompassed all direct patient contacts with a mental health professional, such as face-to-face contacts, telephone contacts, and e-mail contacts, during all received treatments. Treatment duration encompassed the total time in weeks of all mental health care contacts. Initiation of new treatment refers to the proportion of patients who initiated one or more new treatment episodes after termination of the initial treatment within the five-year period. The new treatment could be a follow-up treatment because of recurrence of symptoms or another treatment for other symptoms. Time to new treatment refers to the number of weeks between termination of the initial treatment episode and the start of a new or follow-up treatment. A treatment was usually mutually terminated by the professional and the patient or, in fewer cases, by one of them. Various reasons for terminating a treatment were documented. In most cases, termination occurred because treatment goals formulated by the professional and patient at the start of the treatment were achieved. Sometimes treatment was terminated because no further improvement was expected.
The treatment groups were compared on four variables collected at the trial’s baseline: age, gender, diagnosis according to the Mini-International Neuropsychiatric Interview (
10,
11), and symptom duration before referral, rated by the GP on a 3-point Likert scale (zero to three months, three to nine months, and more than nine months).
Statistical Analyses
Differences between the two treatment groups on baseline variables (gender, age, diagnosis, and symptom duration before referral) were analyzed with chi square tests and t tests in SPSS 20. To assess the difference between CCP and usual care in mental health care contacts and treatment duration, generalized linear mixed models were fitted in R (
12) by using the glmmADMB package (
13), which is an implementation of the AD Model Builder (
14). Both outcome variables were assumed to follow a negative binomial distribution. Patients were designated as level 1 and GP as level 2. Group differences were assumed to be present if the model containing both a random intercept and the group variable had a better fit to the data than the random-intercept–only model as assessed by Akaike’s information criterion (AIC) (
15). In general, a lower AIC represents a better model fit. Treatment group was included as the primary predictor, and the baseline variables were included as covariates if these variables were significantly different between the two treatment groups. First, a random-intercept–only model was fitted, and it was then determined whether addition of the treatment group to the statistical model would lead to a better fit. Subsequently, the baseline variables were added if there were group differences.
To compare CCP and usual-care patients regarding time to a new treatment episode within the five-year time frame, Cox regression was used. The time interval in weeks between termination of the initial treatment and initiation of the follow-up treatment was entered as the time variable, and a dichotomous variable indicating the presence of a follow-up treatment was used as the state variable. Group participation was entered as a covariate. Five patients were excluded from the Cox regression because they remained in their initial treatment for the entire five-year period (that is, their treatment started late in the five-year period).
Results
A total of 139 (84%) of the 165 patients enrolled in the randomized trial could be included in the follow-up analyses. Ten CCP patients (10% of the total CCP group) and 16 usual-care patients (26% of the total usual-care group) had not been registered at the local mental health care institution during the five-year period. [A figure illustrating recruitment is available in an online supplement to this article.] These patients could have received treatment from another mental health care provider or had not had any mental health treatment at all. Of the 139 patients, 134 (96%) had terminated their initial treatment within the five-year period after enrollment. Four patients from the usual-care group and one in the CCP-group had not terminated their initial treatment.
No significant differences were noted between the two treatment groups on the baseline variables gender, age, diagnosis, and symptom duration before referral (
Table 1). Negative binomial mixed-effects models examined the effect of treatment group on the number of mental health care contacts. The model containing treatment group as the predictor had the best fit (AIC=1,271.85), performing better than the random-intercept–only model (AIC=1,273.10). The fixed effect of treatment group was .61 (SE=.33), which means that in general, the usual-care group was predicted to have 1.84 times the number of contacts that the CCP group had (e
.61=1.84). Generalized linear mixed models with a negative binomial distribution for treatment duration, in weeks, showed no group differences (random-intercept AIC=1,606.57; random-intercept plus group AIC=1,608.37).
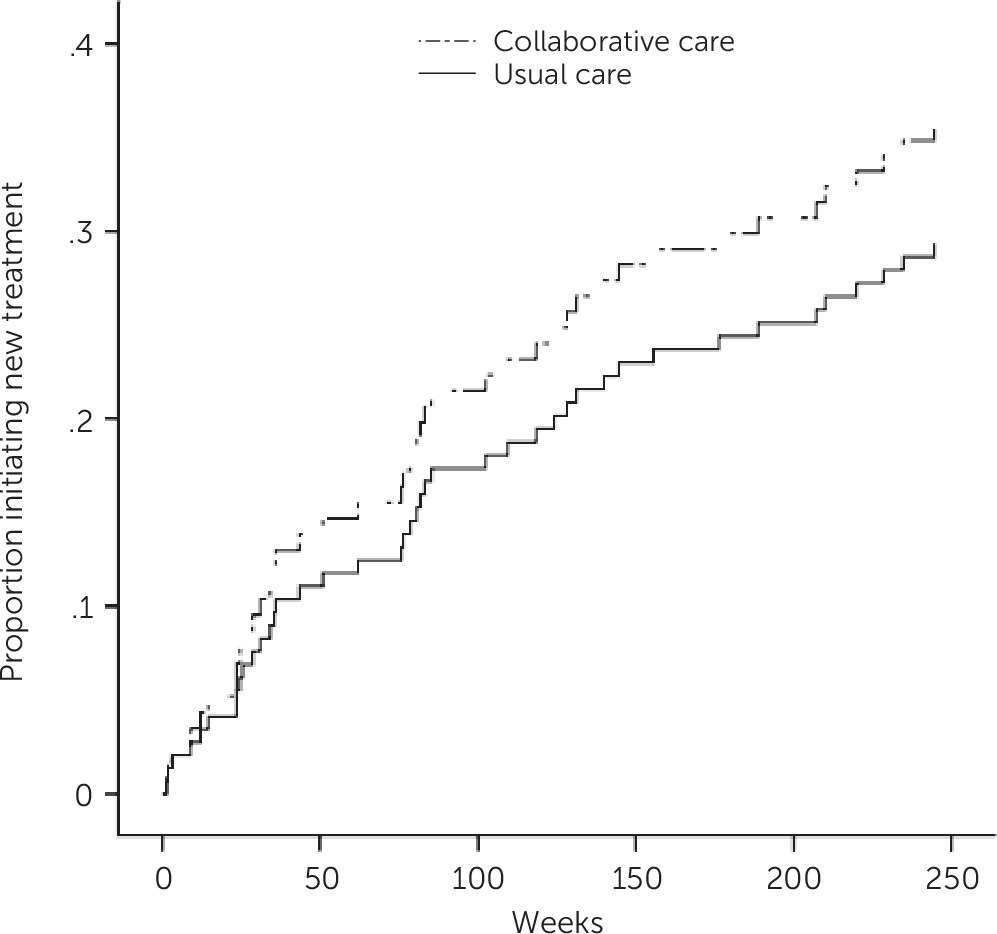
Results of chi square tests showed no significant difference between the CCP group and the usual-care group in the proportion that initiated a new treatment episode. In regard to the time to new treatment, Cox regression analysis did not show any between-group difference. The proportion of participants that received new treatment as a function of time in weeks is depicted in
Figure 1.
Discussion
In this five-year, post-hoc analysis of data from a previously published randomized controlled trial (
8), we found that the short-term (one-year) efficiency gains that resulted from referring patients to collaborative care in the primary care setting rather than to specialized mental health care (usual care) persisted five years after referral. Patients allocated to CCP or to usual care had an equal chance of initiating a new treatment episode (approximately 30% in both groups), and the groups did not differ in the time to new treatment and total treatment duration. Most important, mental health care use by CCP patients was almost half that of the usual-care group. We found no indication of a catch-up effect of mental health care use among CCP patients over the long term. In other words, short-term reduction in the use of mental health care did not lead to a higher use over the longer term.
As far as we are aware, no previous studies have investigated the long-term efficiency of collaborative care compared with usual mental health care. There is evidence that collaborative care is more efficient than usual care provided by a primary care physician over the long term (
6,
7). We now provide preliminary evidence that this is also the case for collaborative care compared with specialized mental health care, at least in terms of mental health care utilization.
The obvious difference in mental health care use could have been caused by several factors: the type and model of the underlying CCP treatment model and the service concept. The treatment model of the CCP is considered to be very intensive, although there is limited contact between the therapist and the patient (
9). In addition to symptom reduction, two important goals of the model are increased empowerment and improved problem-solving abilities (
16). To achieve these goals, patients must be very active between therapy sessions in working on their problems. Usually the interval between sessions increases with the course of therapy. Patients may incorporate this way of working on their problems such that even if a new episode of treatment is necessary, they need fewer contacts with the therapist because they are used to working more independently on problems in their daily life.
Besides this model-based explanation, the difference in use of mental health care could also have resulted from aspects of the collaborative care service concept. Short and intensified communication lines between the GP and therapist, quick referral, and receipt of treatment in the familiar premises of the GP’s offices are factors that may have influenced mental health care use. Favorable effects on access and attrition of offering mental health services in primary care have been demonstrated (
17).
Finally, the shortcomings of this study in regard to the scope and availability of the utilization data should also be noted as a possible explanation. First, the analyses were based on mental health care use at a regional mental health care organization, and services received from other mental health professionals, such as private psychiatrists and psychologists, were beyond the scope of our analyses. The second limitation was the inability to assess possible shifts in costs to other sectors (for example, costs of general health care and productivity losses) because we did not contact the patients to assess additional costs. There is some evidence that patients receiving minimal interventions tend to seek subsequent additional treatment elsewhere (
18). Thus it is possible that the actual amount of care that the patients received was underestimated. Inclusion in the analyses of cost data for services delivered by other mental health care providers and in other health care sectors as well as cost data for productivity losses could have produced different results.
Notwithstanding these limitations, the loss of information from dropout or failure to track patients was restricted because the vast majority of the study group was treated by the same regional mental health care organization. However, there was a noticeable difference between the two treatment groups in the number of patients for whom we did not have utilization data. Although only 10% of the original CCP study group was not traceable in the electronic health record, the proportion not traceable in the usual-care group was 26%. Patients in the CCP may have been more likely to seek help than patients who received specialized care, and CCP patients may have been more accepting of care than those who received specialized care, as found in a study of elderly patients by Bartels and colleagues (
5). Focused research is needed to compare acceptance of collaborative care and of regular specialized mental health care in an adult patient population.
Collaborative mental health care with a primary care physician who works in close alliance with a mental health professional has become an important part of mental health care in many industrialized countries, and reforms to extend collaborative care even more are under way (
19,
20). In the Netherlands, mental health care reforms were implemented in 2014. Currently, the primary-care sector and a part of the specialized mental health sector form so-called basic-mental health care. Basic care is for patients with mild to moderate, noncomplex mental health problems and patients with stable chronic mental health problems. Specialized secondary mental health care is for patients with severe mental health problems.
Favorable short-term effects of collaborative care on effectiveness and efficiency have been documented (
1,
8). A thorough evaluation of the efficiency of collaborative care demands the extension of the follow-up period for cost analyses.
Conclusions
The findings provide preliminary evidence that for patients with nonacute common mental disorders referral to collaborative mental health care as a first intervention, compared with referral to specialized mental health services, leads to fewer contacts with a mental health care professional over the short and long terms. Further research on long-term costs and benefits from a societal perspective is recommended.