The passage of the Affordable Care Act (ACA) provides new opportunities to address the fragmented system of care that exists in the United States for persons with serious mental illness and chronic general medical conditions (
1). Persons with serious mental illness have earlier mortality compared with the general population, which is due in part to harmful behaviors such as smoking, shortened lifespans due to common chronic conditions, and less access to and use of primary care (
2). The potential for improving health outcomes through the increased coordination of mental health and general medical care has been demonstrated both in randomized controlled trials and by a nationwide demonstration project (
3–
8)
The Medicaid Health Home State Plan Option provides states with an opportunity to improve access to care for persons with multiple chronic health conditions, including serious mental illness. Health homes, also called medical homes, are intended to provide a person-centered system of care that includes coordination of general medical and behavioral health services along with community-based health supports in an effort to improve the quality of health care and reduce costs (
9–
11). For example, Medicaid beneficiaries with serious mental illness who were enrolled in a medical home in North Carolina were shown to have greater use of primary and specialty mental health care, improved medication adherence, and reduced use of emergency services compared with similar beneficiaries who were not enrolled (
12). To date, 19 states have approved state plan amendments to implement the health home provision of the ACA; 11 of these states have a specific focus on persons with serious mental illness (
13).
California is among the majority of states currently without the Medicaid health home provision. However, the state is unique in having signed into law the Mental Health Services Act (MHSA) (
14), which places a 1% tax on incomes greater than $1 million to create new funding streams for community mental health services. One of these funding streams supports piloting time-limited programs to test innovative delivery models. The Los Angeles County Department of Mental Health applied its funding to develop integrated health homes for persons with serious mental illness, thus providing an opportunity to study the implementation of integrated care in a diverse population in a large public mental health system.
This study examined two models of integrated health homes that were implemented in Los Angeles County to improve access to care among persons with serious mental illness, chronic general medical conditions, and co-occurring substance use disorders. Although research supports increased coordination of mental health and general medical care, less is known about the relationship between implementation of integrated health homes at the system level and health outcomes among persons with serious mental illness (
15).
Methods
In the first model, five integrated mobile health team combined a Housing First approach to supportive housing—providing immediate housing without readiness requirements or requirements for treatment participation—with an assertive community treatment model of behavioral health services. The mobile health teams paired with a federally qualified health center (FQHC) to provide general medical services. Primary care was embedded in the mobile teams to provide field-capable clinical services, including blood draws, blood pressure measurements, and wound care, and to coordinate general medical care with the FQHC. In the second model, five integrated clinics paired community mental health centers with FQHCs. Both models aimed to improve the coordination of care by providing mental health, general medical, and substance abuse services within an integrated multidisciplinary team.
This study examined changes in two measures of health outcomes: client self-reported physical health status and clinician-reported mental health recovery. Physical health status was measured by using the physical health items of the Global Health Scale of the Patient Reported Outcome Measurement System, an assessment system for self–reported health sponsored by the National Institutes of Health. The Global Health Scale assesses overall health and includes ten items that assess physical, mental, and social health (
16).
Mental health recovery was measured by using the Illness Management and Recovery (IMR) scale. The IMR scale includes 18 items that address involvement in recovery activities, for example, progress toward personal goals, social connectedness, and relapse prevention planning; illness management, for example, symptom distress, impairment in functioning, and coping; and substance abuse, for example, impairment of functioning caused by alcohol or drug use (
17). Total scores for each measure were calculated as the mean score for all items.
This study also examined rates of screening for common chronic conditions and changes in their associated clinical indicators. Screening included measurement of blood pressure, cholesterol, and blood glucose to indicate hypertension, high-risk cholesterol levels, and prediabetes and diabetes, respectively.
Hypertension and high-risk cholesterol levels were identified according to guidelines from the American Heart Association. Stage 1 hypertension was indicated by systolic blood pressure of ≥140 mmHG or diastolic blood pressure of ≥90 mmHG. High-risk cholesterol was indicated by low-density lipoprotein of ≥160 mg/dl or high-density lipoprotein of ≤49.9 mg for men or ≤39.9 mg for women. Prediabetes or diabetes was identified according to guidelines from the American Diabetes Association as a fasting plasma glucose level of ≥100 mg/dl or a glycosylated hemoglobin level of ≥5.7%.
Programs were instructed to collect health outcome measures at the baseline visit and during follow-up visits at three-month intervals. Clinical indicators were collected at baseline and six month intervals. Demographic data were collected at baseline. Data were collected by using a secure, Web-based health outcomes measurement system that provided data to evaluators and individual- and program-level reports to providers that allowed them to track the health outcomes of their clients. Data collection was reinforced through quarterly learning collaboratives, which were used to convey the importance of data collection for program evaluation and for the development of strategies for quality improvement. The learning sessions focused on establishing a level of trust among providers and between providers and the Department of Mental Health. These relationships supported exploration of the outcome data and transparency in the use of the data to improve service delivery and to inform future funding decisions. Key activities included targeted training, focused small-group discussions, and panel discussions to promote collaboration between providers, enhance service offerings, and improve collection and sharing of data.
Program-level integration of mental health and general medical care was measured during site visits by using the Integrated Treatment Tool (ITT) (
18). The ITT was developed through a Primary and Behavioral Health Care Integration grant from the Substance Abuse and Mental Health Services Administration (SAMHSA) to develop a framework to guide the implementation of a person-centered health care home for individuals with serious mental illness. The ITT was designed to serve as an assessment for program improvement. Among the tools recommended by SAMHSA to measure primary and behavioral health care integration, the ITT has the strongest focus on persons with serious mental illness. Most existing measures consider the integration of mental health care into primary care, whereas the ITT considers integration of primary care into specialty mental health care (
19).
The ITT consists of 30 discrete items across three domains: organizational characteristics, treatment characteristics, and care coordination and management characteristics. Each item is scored on a scale of 1 to 5, with higher scores representing increased levels of integration. Scores are determined by using predefined algorithms, and data are derived from interviews with program staff, observation of program activities, and a review of program documents. Factor analysis was used to map the 30 items to a single factor score and to rank programs by level of integration; a natural cut point was used to categorize programs as having a high or a low level of integration (
20). [A copy of the ITT is available as an online
supplement to this article.]
Changes in physical health status and mental health recovery by level of integration were estimated by using generalized estimating equations, which allows for errors that are correlated within individuals and over time as well as for missing data from some individuals and time points (
21,
22). The primary independent variables of interest were indicators of level of integration by time. Additional covariates controlled for model type and individual-level characteristics, including age, gender, race-ethnicity, and clinical diagnosis. Predicted values at each time point were used to create graphs illustrating changes in physical health status and mental health recovery by level of integration over time. Chi-square tests were used to assess the difference in participants’ physical health status and mental health recovery by level of program integration at baseline, and joint chi-square tests were used to assess changes in physical health status and mental health recovery at follow-up time points (three, six, nine, and 12 months). Logistic regression was used to compare the probability of screening by level of integration. Changes in clinical indicators from baseline to six-month follow-up were estimated by using paired t tests.
Results
Differences in Program Characteristics by Level of Integration
Differences across programs in organizational characteristics, treatment characteristics, and care coordination and management characteristics by level of integration are shown in
Table 1. There were few differences across programs with respect to organizational characteristics. For example, both high- and low-integration programs received high scores with respect to organizational philosophy, meaning that organization stakeholders understood and accepted core elements of the integrated health care model and were committed to a strategic plan for its implementation. Yet they received low scores with respect to organizational policies and procedures, indicating that they did not have written policies and standardized procedures for each element of the integrated health care model. However, more highly integrated programs had higher scores for peer supports, meaning that they were more likely than programs with low levels of integration to employ individuals with lived experience as members of their multidisciplinary teams. They also had higher scores for continuous quality improvement, meaning that they were more likely than programs with low levels of integration to monitor patient-level outcomes and program-level implementation process measures for program improvement.
With respect to treatment characteristics, more highly integrated programs were more likely than programs with low levels of integration to use pharmacological approaches that followed state-of-the-art guidelines for persons with serious mental illness. More highly integrated programs also employed more strategies than programs with low levels of integration to encourage patients to identify members of their social support networks and to engage those persons in the treatment process.
The greatest differences across programs were in the domain of care coordination and management characteristics. Compared with programs with low levels of integration, more highly integrated programs had more sophisticated approaches to coordination and management of care, referral to specialists, and tracking the results of referrals. More highly integrated programs had a more structured approach to reconciling the multiple medications used by persons with multiple chronic conditions. These programs also provided more systemized reminders for clients and providers for upcoming appointments, tests, or procedures.
Changes in Health Outcomes by Level of Integration
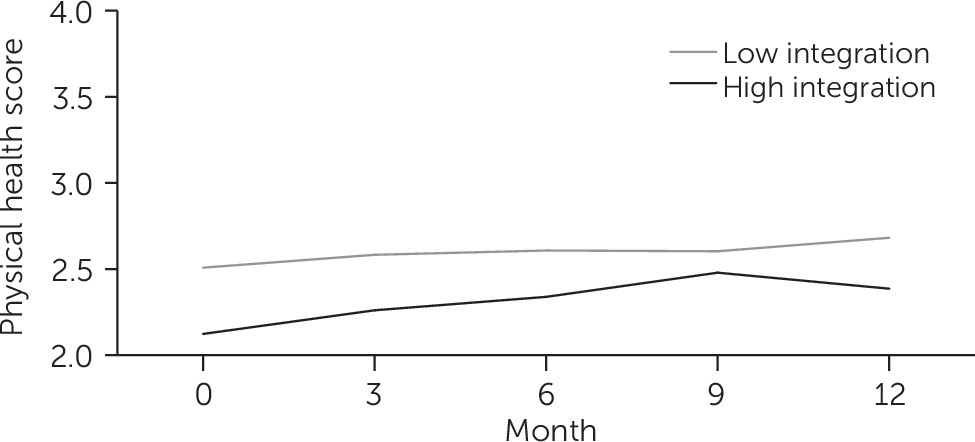
Changes in self-reported physical health status by level of program integration are shown in
Figure 1. Mean scores on the client-reported physical health items of the Global Health Scale were lower at baseline among clients in more highly integrated programs (p<.01). Physical health status did not improve significantly among clients in programs with low levels of integration but improved significantly among clients in more highly integrated programs (p<.01). Scores improved to a greater extent among clients in more highly integrated programs compared with clients in programs with low levels of integration (p<.05).
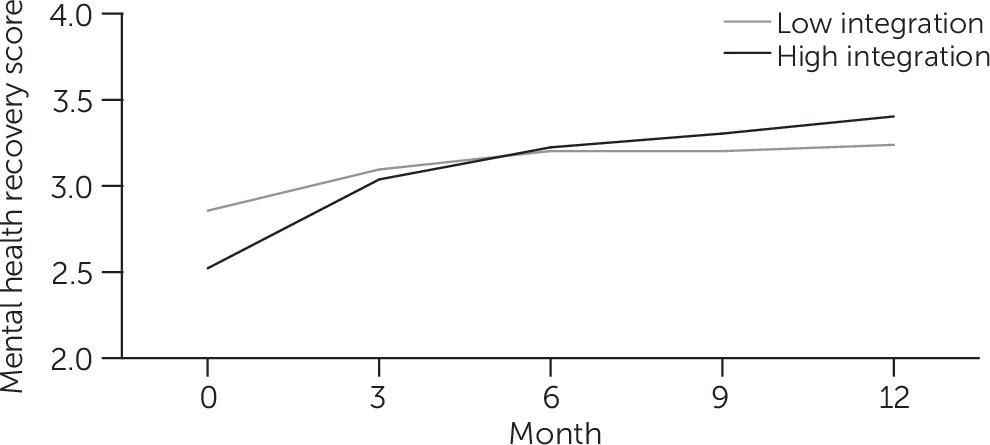
Changes in clinician-reported mental health recovery by level of program integration are shown in
Figure 2. Mental health recovery scores were also lower at baseline among clients in more highly integrated programs (p<.01). Mental health recovery improved among clients overall (p<.01) and improved to a greater extent among clients in highly integrated programs compared with clients in programs with low levels of integration (p<.01).
The capture of health outcomes data was incomplete. Overall, 1,941 individual enrolled in the integrated care programs; 1,480 individuals (76%) provided one or more measures of physical health status, and 1,668 (86%) individuals provided one or more measures of mental health recovery. Although the capture of health outcomes data declined over time, there were no statistically significant differences in follow-up at 12 months between programs with high and low levels of integration for either health status or mental health recovery.
Differences in Screening Rates and Changes in Clinical Indicators by Level of Integration
Screening rates for blood pressure, cholesterol, and blood glucose by level of program integration at baseline and six-month follow-up are shown in
Table 2. Clients in programs with a high level of integration were more likely to receive all types of screening compared with clients in programs with a low level of integration (p<.01). Indicators of clinical risk factors among clients who received screening at baseline and six-month follow-up are shown in
Table 3. Among more highly integrated programs, there was a decline in the number of clients who were identified with hypertension and an increase in the number of clients who were identified with prediabetes or diabetes (p=.01). There were no statistically significant changes in clinical risk factors among clients in programs with lower integration; however, the observed changes in clinical risk factors were similar in direction and relative magnitude to those observed among clients in more highly integrated programs, and the sample size was considerably smaller, limiting the power to detect significant changes in this group.
Discussion
This study examined the implementation of integrated health homes for persons with serious mental illness in Los Angeles County. We found that clients who enrolled in programs that were more highly integrated with respect to their organizational, treatment, and care coordination and management characteristics had greater improvement in self-reported physical health status and clinician-reported mental health recovery. We also found that rates of screening for common chronic conditions were higher among more highly integrated programs. With respect to clinical outcomes, there were reductions in the numbers of clients with hypertension in more highly integrated programs, although this was accompanied by a worrisome increase in the number of clients with prediabetes or diabetes. These findings suggest that additional efforts may be needed to target specific contributing factors to glucose intolerance, including the metabolic effects of antipsychotic medication.
Integration of general medical and behavioral health care was measured by using the ITT, which SAMHSA recommends as a measure of integration of health care for persons with serious mental illness. Using the ITT, we found that the greatest differences between programs with high or low levels of integration were in the area of care coordination and management, followed by treatment characteristics and organizational characteristics. The differences in outcomes among programs with high or low levels of integration reflect differences in ITT characteristics for this particular sample of programs. Among different samples of integrated programs, there may be greater differences between other ITT characteristics (for example, organizational characteristics), in which case the outcomes of high- and low-integration programs may be associated with these characteristics. A much larger sample of integrated programs, with greater variation across all ITT items, would be required to assess the importance of the full range of items measured by the ITT in measuring outcomes of integrated care.
Future efforts should also focus on achieving higher rates of screening and greater improvements in clinical indicators. These efforts could include a greater emphasis on health promotion, chronic disease self-management, and integrated pharmacotherapy for mental and general medical disorders in order to provide optimal treatment of psychiatric illness that does not result in deleterious side effects, such as metabolic syndrome (
23). Mental health and general medical providers should work more collaboratively to ensure that the medications used to reduce symptoms of mental illness do not negatively affect clients’ health.
The Los Angeles County Department of Mental Health pursued its health home pilot program by using a funding stream from the MHSA that emphasized the testing and evaluation of innovative programs. A similar result could have been achieved by using the Medicaid health home option, which provides an enhanced federal match for care management and care coordination, transition care management, and linkages to community services. The Medicaid Health Home State Plan Option will support the generalizability of health homes for persons with serious mental illness. The option is not currently available in California, but the legislature has authorized the state to submit an application, and the California Department of Health Care Services has developed a concept paper describing health homes for patients with complex needs.
This study had several limitations. Health outcomes were measured by client or clinician report. Outcomes were collected during ongoing treatment, and clients who did not visit a provider during a collection period did not provide outcomes data. Although we found no differences in rates of follow-up by level of integration, loss to follow-up overall was fairly high, limiting the generalizability of the findings. In addition, despite SAMHSA’s promotion of the ITT, there is insufficient evidence to consider the ITT a fully validated instrument to measure integration. Nevertheless, the ITT provides a framework to consider differences among integrated programs.
Assuming that the ITT differentiates between programs with high versus low integration, it is unknown whether integration was a causal factor in the findings or if other, unobserved program characteristics were related to both integration and health outcomes. Further work is necessary to understand facilitators of and barriers to integration as well as how various domains of integration are related to health outcomes. Finally, although we were able to compare programs identified as having high versus low integration, this study did not include a comparison group of nonintegrated programs, which reflects an assumption that integrated care has been established as superior to nonintegrated care.
Conclusions
In this study of Los Angeles County’s integrated health home pilot program, we found that clients in more integrated programs had greater improvements in physical health status and mental health recovery, higher rates of screening for common chronic conditions, and greater reductions in blood pressure compared with clients in less integrated programs. Administrators and policy makers may want to consider implementing policies and procedures that encourage the measurement and continuous improvement of integration in combined general medical and mental health programs. Additional research is necessary to identify predictors of integration and to determine whether improved integration or other aspects of high-performing health programs drive improvements in health outcomes.