Evidence is building that a host of specific cultural competence activities conducted by organizations, programs, and clinicians can improve outcomes (
1) and reduce costs (
2). The definition of cultural competence by Cross and colleagues (
3) as “a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals and enables that system, agency, or those professionals to work effectively in cross cultural situations” emphasizes that cultural competence is a systemic intervention encompassing activities at all levels of a care system. The beneficiaries of cultural competence are, of course, consumers. However, the distinct role that consumers can play in its promotion has not yet been addressed.
Health activation is embraced by health care reformers as a way to improve patient outcomes. It is a person-centered concept reflecting that the efficacy of health care is a two-way street. Health-activated patients participate in their care delivery by becoming health literate and asking questions of their providers about their treatments, ways to pursue healthy life styles, and actions to control their health challenges. The Patient Activation Measure (PAM) assesses a patient’s level of health activation (
4). More activated patients have been shown to have better health outcomes (
4,
5). In behavioral health care, consumers are also being encouraged to take more active roles in their care. The New York State Office of Mental Health MyPSYCKES (
6), a computer-based tool that supports shared decision making, allows Medicaid beneficiaries to view and comment on their psychotropic medication use history, access educational materials and recovery tools, and use a shared decision-making tool. The Cambridge Health Alliance’s DECIDE Intervention, a three-session health education curriculum, teaches clients to formulate questions and devise plans to communicate about and address factors that affect their mental health care (
7). Neither of these approaches specifically addresses cultural issues.
Cultural Activation and Its Measurement
“Cultural activation” is defined as a consumer’s recognition of the importance of providing cultural information to providers about cultural affiliations, challenges, views about, and attitudes toward behavioral health and general medical health care, as well as the consumer’s confidence in his or her ability to provide this information. Cultural activation is a form of shared decision making and a facet of consumer empowerment. The American Psychiatric Association (APA) has recognized that cultural information is critical to appropriate diagnosis and treatment and to recovery planning (
8).
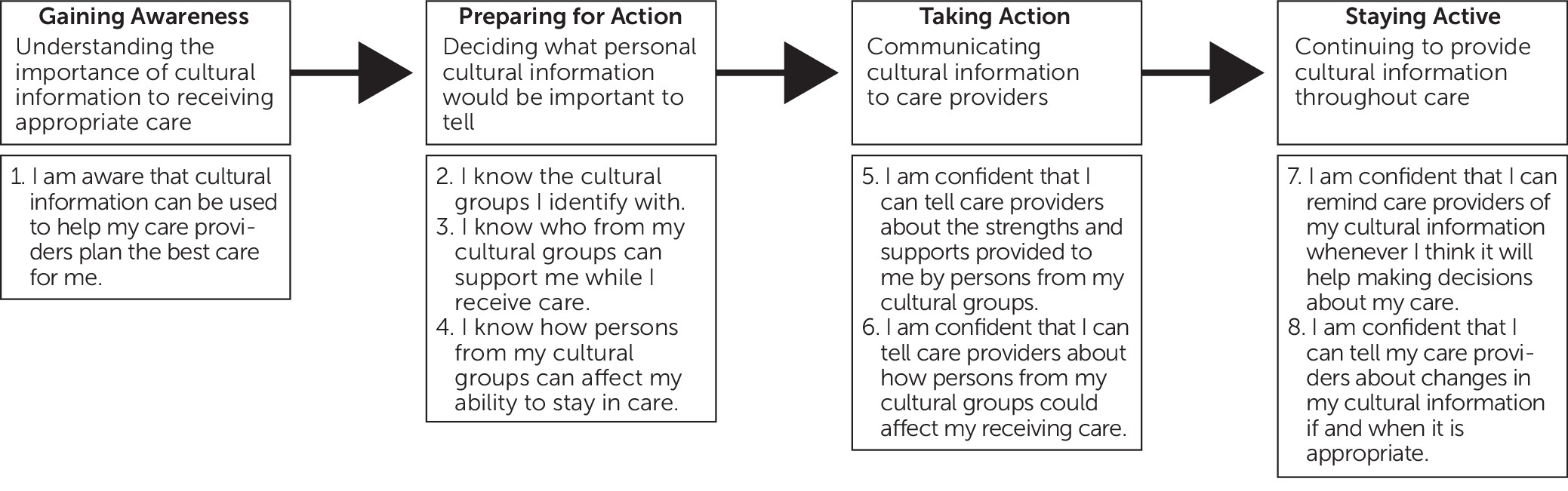
Cultural activation takes place over time and through multiple stages (
Figure 1). Stages have been conceptualized parallel to the patient activation process described by Greene and colleagues (
5) and to the stages of behavioral change in addiction treatment (
9). In stage 1, a consumer gains awareness of the value of cultural information, a form of health literacy, because the consumer may not be aware that cultural information about his or her mental health challenges can inform diagnosis, treatment planning, and recovery recommendations for community living. Stage 2 involves preparing for action and is a consciousness-raising phase in which consumers affirm their cultural identities and review cultural facets of their life that might affect their view of their mental health challenges to determine what helps and hinders them in recovery. Stage 3 is preparing to take action—that is, feeling comfortable to transmit information. Culturally activated consumers might be prepared to present cultural information whenever or to whomever they feel would benefit from hearing it. Stage 4 is staying active—that is, feeling confident to repeat information when the consumer feels it is appropriate and updating the information as life circumstances change. The Cultural Activation Measurement Scale (CAMS) has been developed in a group research process to measure a consumer’s progress through these stages guided by the items of the PAMS. It is currently being tested for its reliability.
Cultural Activation Prompts
Consumers can be culturally activated by using educational materials, videos, and group discussion processes. One deliberate way is through the “Cultural Activation Prompts (CAPs),” a set of 15 prompts designed to help consumers give providers cultural information about their identities, their views of their mental health challenges, and the supports and barriers that they may encounter (
10). [A table listing the CAPs is included in an
online supplement to this column]. Conversations with providers can take place as early as possible, whenever needed. Prompts can be wholly or partly used and expanded upon.
CAPs prompt consumers to talk about their multidimensional cultural identities, because most persons identify with an “inherent group,” such as an ethnic group, and with one or more experiential groups based on life circumstances; for example, a peer specialist may strongly identify with a peer culture. The CAPs draw on the domains covered in the
DSM-5 Cultural Formulation Interview (CFI) (
11) and on the “three C’s” of Kleinman’s (
12) explanatory model of illness: call, cause, and course. The CFI, which was developed by an APA committee, is intended to be administered to elicit a cultural definition of the consumer’s problem; cultural perceptions of cause, context, and support; and cultural factors affecting self-coping and past and current help seeking (
11). APA recommends that providers make a cultural assessment with the CFI to enhance the cultural validity of the diagnostic assessment, facilitate treatment planning, and promote patient engagement and satisfaction.
A culturally activated consumer can relay information at any time. Peer specialists are an excellent choice to facilitate the cultural activation process. They have lived experience of mental illness and work in clinical programs to provide supports to consumers to engage and remain in care. They could help consumers understand the value of the CAPs and rehearse them in using the CAPs. Training materials for peer specialists and advocates are currently being prepared to facilitate this process. Care coordinators working in new integrated care programs could also facilitate cultural activation because they take a holistic view of clients. Waiting rooms could have consumer friendly materials to encourage activation and even a poster with the CAPs. The concept could be introduced in medical education and residency training programs and in cultural competency curricula for clinician training to garner clinical support and openness to hearing this information.
Feasibility of Cultural Activation
Reactions to cultural activation among stakeholder groups at state and local community Multicultural Advisory Committee meetings, at conference work groups for peers and providers, and at a keynote address at the College for Behavioral Leadership Academy of Community Health have been mostly enthusiastic. Consumers and provider agency representatives have been supportive, although clinician reactions have been mixed. One psychiatrist suggested that cultural activation would be useful in preparing a consumer for assessment with the CFI by helping the consumer understand and better respond to CFI queries, which may reduce the time needed to conduct the CFI. On the other hand, some clinicians expressed their concern that use of shared-decision making and cultural activation may lead consumers to discount the value of clinicians’ clinical work, which would diminish their efficacy. Peer specialists felt that some clinicians would not be interested in cultural information, regarding it as unimportant or concluding that such information is “trumped” by other clinical information obtained through conventional interviewing techniques.
The introduction of new models of integrated care increases the likelihood that cultural activation will become an integral component of usual care. For example, components of cultural competence are being mandated in Medicaid reform initiatives, including managed care, health homes, accountable care organizations, and provider networks established under Delivery System Reform Incentive Payment (DSRIP) program (
13). DSRIP monies are used to support value-based payment models of integrated care in which provider networks are financially incentivized as a group when clients in the network have improved outcomes. In New York State, both health literacy and cultural competence have been singled out as necessary organizational components for achieving “value,” and patient activation is endorsed. Its measurement in New York State provides points toward a value-based payment. Cultural activation is a logical next step because it supports the goals of health literacy, patient activation, and cultural competence.
Conclusions
Cultural activation is a new construct. Although it passes the test of face validity, with endorsements from both clinicians and consumers, testing is required to show its relationship to outcomes. However, we hypothesize that increased cultural activation will improve consumer outcomes and that tools such as the CAPs can increase consumer cultural activation. New health care models are rapidly being introduced with strong endorsements of both cultural competence and patient-centered care approaches. These models offer an opportunity to test the value of cultural activation.