Schizophrenia affects approximately 1% of the world’s population, and it is characterized by potentially devastating symptoms, including abnormal perceptual experiences, lack of expressiveness, social withdrawal, and cognitive difficulties (
1). Because of the chronicity, severity, and marked psychosocial impairment that may characterize the illness, schizophrenia is estimated to cost $23 billion in direct costs and nearly $40 billion in indirect costs annually (
2).
Illness relapse substantially contributes to the expense of schizophrenia, and inpatient costs for patients experiencing a relapse have been estimated to account for $2.3 billion annually (
3). Treatment costs for individuals who have relapsed remain elevated for 12 months after they have been discharged from the hospital because of increased service utilization. Therefore, preventing relapse of illness and resultant hospitalization is an important cost-saving strategy to employ in the treatment of schizophrenia (
4,
5).
Early-intervention (EI) services for schizophrenia have been shown to attenuate many of its psychiatric, general medical, and social comorbidities. EI services focus on aggressive identification and treatment of the illness as early as possible in the disease course (
6,
7). As such, EI services offer a potentially powerful vehicle for reducing the financial costs associated with schizophrenia. Prior studies of the cost of EI services to date have generally shown that these services are associated with savings in the cost of mental health care (
8–
10).
One such EI service is the Prevention and Recovery Center for Early Psychosis (PARC), an EI program in Indianapolis that opened in May 2009. The guiding principle at PARC is to “prevent the preventable,” which includes a strong emphasis on relapse prevention. Services are targeted toward patients with first-episode psychosis (FEP) and are provided in an outpatient setting offering enhanced staff-to-patient ratios and youth-friendly engagement techniques. Flexible physician and nurse scheduling allows patients to be seen by a clinician from these disciplines as frequently as needed during regular treatment and as quickly as needed during crises. This staffing model improves both early detection and quick intervention for relapses.
This study was a retrospective review of medical records and health service utilization data. Its aim was to compare health service utilization and cost of care for FEP patients in the PARC model and a matched cohort of FEP patients who received treatment as usual.
Methods
Two Eskenazi Health Midtown Community Mental Health (Midtown) clinics served as study sites: PARC (intervention cohort) and the James Wright Center (JWC) (treatment-as-usual cohort). Eskenazi Health is one of the nation’s largest safety-net health systems and is affiliated with Indiana University. Patients were selected via review of the Midtown electronic medical record. Individuals in both cohorts were identified by the following inclusion criteria: between ages 16 and 30 and having experienced within the past two years the onset of psychotic symptoms that caused dysfunction or prompted treatment. Individuals were not included if they had a known IQ of less than 70 or a known affective or substance-induced psychosis. All participants in both cohorts were diagnosed as having a schizophrenia spectrum disorder.
All patients who were receiving treatment at PARC from May 14, 2009, to April 30, 2011, a total of 717 days, were included. Thus the maximum duration of treatment possible for any patient at PARC was 717 days.
The comparison cohort was identified from JWC, an adult outpatient community mental health clinic treating individuals with severe mental illness without exclusion for age or duration of illness; there is no specific focus for treatment of FEP, and FEP patients are treated alongside all other patients. JWC provides standard, community-based schizophrenia treatment (treatment as usual) and was chosen as the source for the comparator group because prior to the development of PARC, it was the Midtown treatment center for individuals in all stages of psychotic illnesses, including persons with FEP. Both sites have academic affiliations, but clinical services are provided within a community mental health center framework, and clinical research was not conducted at either site during the data collection periods. A principal difference between the two treatment settings is the greater frequency of clinical contacts by physicians and nurses at PARC to monitor for early signs of relapse and to facilitate rapid intervention when needed.
The treatment-as-usual cohort included patients who enrolled in treatment at JWC between January 1, 2005, and May 1, 2008, who would have met entry criteria into the PARC program had it been developed at the time. A longer enrollment period was necessary for the comparison sample in order to enroll comparable sample sizes in both groups because fewer JWC patients met the inclusion criteria per year compared with PARC patients. To avoid introducing bias on the basis of the differing enrollment periods, the study restricted the data collection period for each participant to a maximum of 717 days (the maximum possible period of treatment at PARC) in both groups; thus, although the enrollment periods differed in duration, the data collection periods did not.
The two FEP cohorts were then matched by age, race, sex, and diagnosis. In addition, it should be noted that both cohorts were drawn from the same health care system, covering the same catchment area, such that the participants in both samples were similar with regard to living environment and socioeconomic status.
Procedures
Approval was obtained from the Indiana University Institutional Review Board, along with a waiver of informed consent for participation in the study.
Diagnostic, demographic, and health service utilization data for each participant were extracted from the Midtown electronic medical record and from the Regenstrief Medical Record System, which captures clinical and health service utilization data for PARC, JWC, and all major hospitals in the Indianapolis metropolitan area.
Health service utilization data were collected for all services rendered for both cohorts. Health services were grouped into the following categories: emergency medical treatment (emergency room visits), psychiatric crisis assessment and treatment (ambulatory outpatient mental health crisis center visits), psychiatric inpatient treatment, and outpatient clinic treatment.
In order for the study to evaluate the individual services rendered, outpatient clinic treatment was further broken down into the following service categories: case management (individual and group psychoeducation, training in activities of daily living, and linkage to resources), therapy (initial biopsychosocial assessment and individual, group, and family psychotherapy), nursing services (nursing assessments, for example, vital signs and movement scales; medication injections; and medication education), psychiatrist services (initial assessments and medication management), and occupational therapy (specifically geared toward improving work and school functioning).
Fees for each service were determined by using Midtown service fee charges for fiscal year 2013 for outpatient services and the Eskenazi Health McKesson Charge Descriptor Master File for emergency and inpatient services. For emergency medical treatment, psychiatric crisis assessment and treatment, and psychiatric inpatient treatment, the fee for the service rendered most frequently for both cohorts was chosen to represent the charge for all services within each category. The emergency medical treatment fee was established to be $1,364 per service, the psychiatric crisis assessment and treatment fee was $165 per service, and the psychiatric inpatient treatment fee was $1,443 per service (one hospitalization day). Of note, although emergency and inpatient services were captured for all major Indianapolis hospitals, fees were based on those charged by Eskenazi Health, the hospital where the majority of emergency services, psychiatric crisis and assessment services, and inpatient hospitalizations occurred.
The outpatient clinic treatment fees were established by taking the average fee for all services provided in each category (case management, $44 per service; therapy, $228; nursing services, $66; psychiatrist services, $251; and occupational therapy, $305).
Rehospitalization rates and total number of hospital days were also collected. Global psychiatric hospitalization rates for the health system (the number of inpatient psychiatric admissions divided by number of patients presenting for emergency treatment) were also calculated in order to evaluate the potential impact of practice patterns over time. Differences in these rates over time would be expected if substantial changes occurred in treatment practice patterns, such as a change in the number of inpatient beds, in the criteria for admission, or in the number of patients presenting for emergency treatment.
Analyses
Chi-square and independent-samples t tests were used, as appropriate, to compare differences between the groups in demographic variables (
11). Because of the difference between cohorts in the mean days in treatment (
Table 1), group comparisons were covaried for number of days in treatment. The health services utilized by patients in both cohorts were then converted to total fees for these services by using the amounts listed above. General linear model multivariate analysis of variance was applied to the cost of each service, with cohort as the between-subjects factor.
Results
The PARC sample comprised 76 patients, and the treatment-as-usual sample comprised 75 patients.
Table 1 lists demographic characteristics and number of days in treatment for both groups. The groups differed in total number of days in treatment (p=.001). Therefore this variable was used as a covariate in all further comparisons.
Table 2 lists total number of visits by participants in both groups, by type of visit.
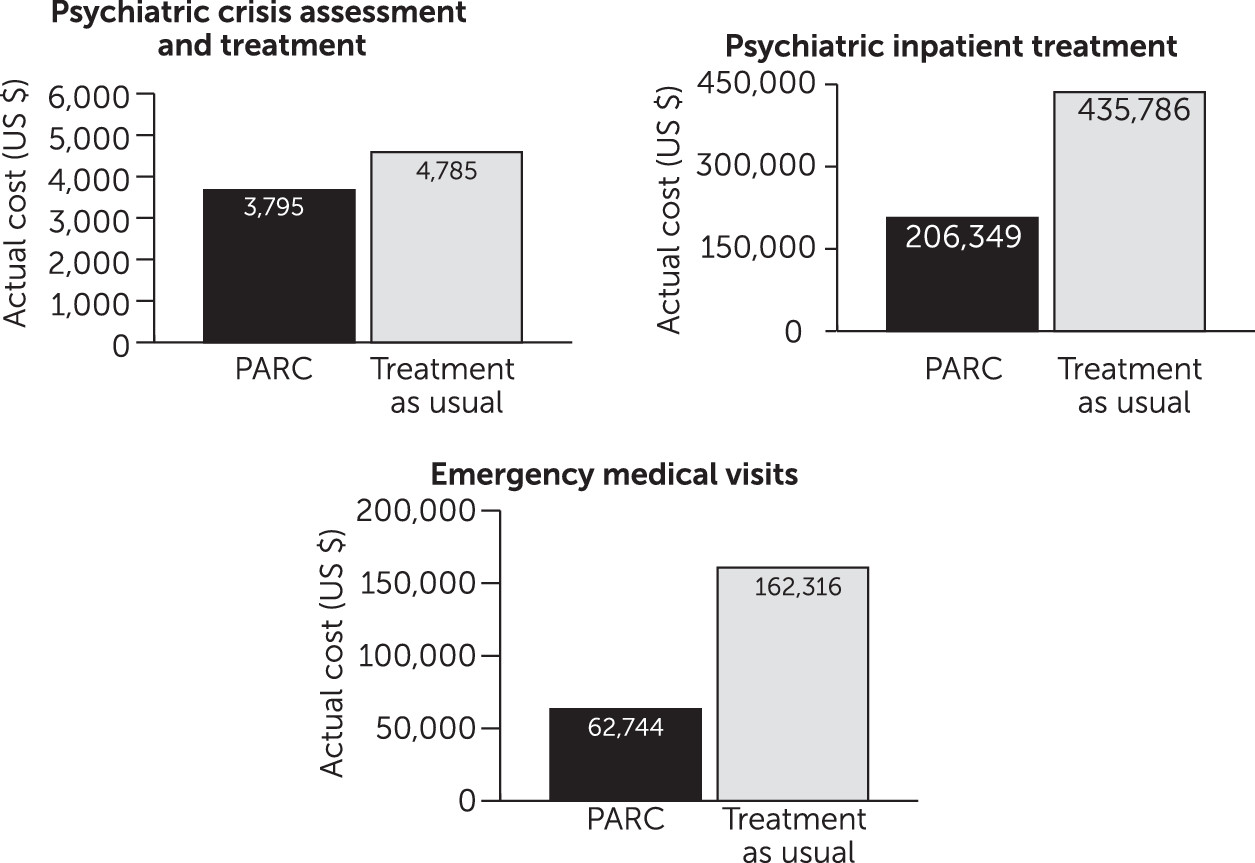
Group comparisons showed that treatment at PARC resulted in an overall reduction in total treatment cost (F=3.71, df=1 and 151, p=.05) compared with treatment as usual. The overall total cost for acute services was also lower for the PARC cohort (F=13.32, df=1 and 151, p
<.001). When broken down further by visit type, the costs of all services were lower for the PARC cohort (psychiatric crisis assessment and treatment [F=5.68, df=1 and 151, p
<.05], psychiatric inpatient treatment [F=10.41, df=1 and 151, p
<.01], and emergency medical visits [F=8.04, df=1 and 151, p<.01)]) (
Figure 1).
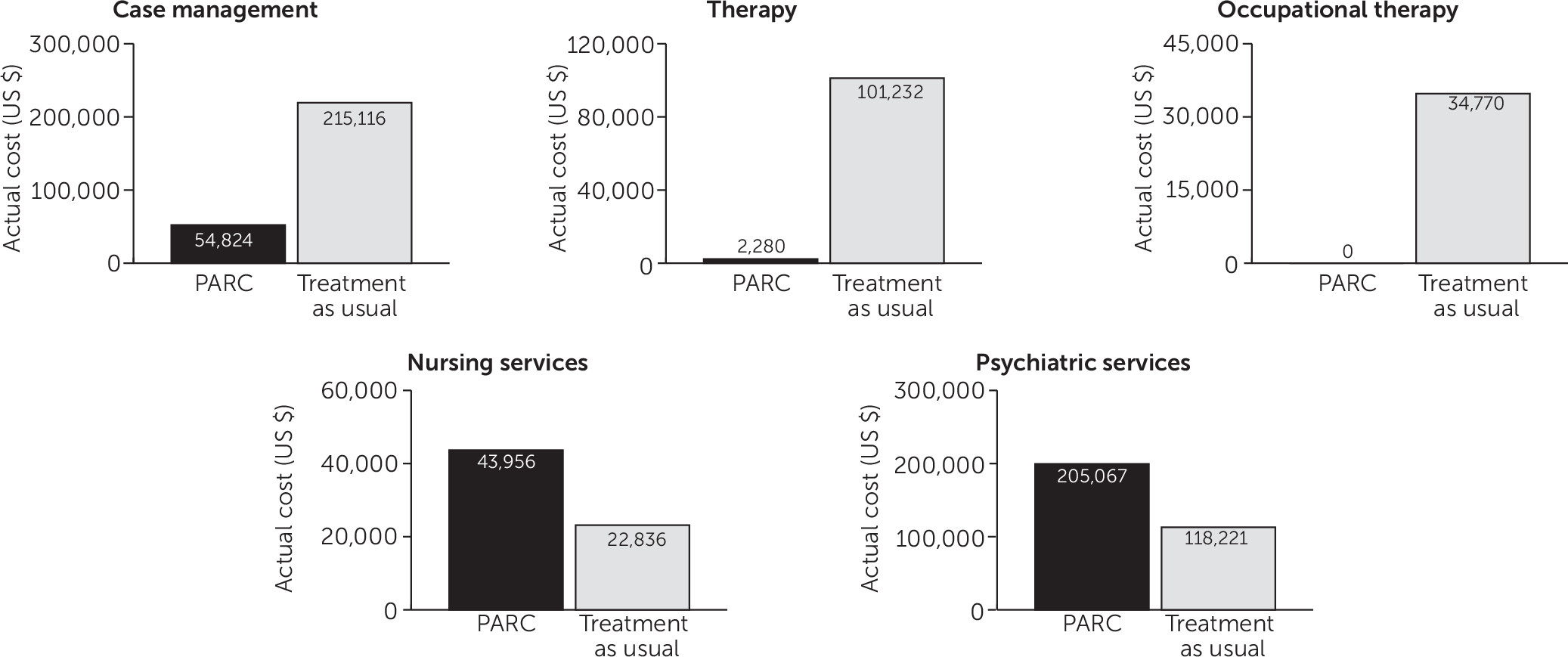
For outpatient clinic services, group comparison showed no overall difference in outpatient costs. The costs of case management (F=14.85, df=1 and 151, p<.001) and therapy (F=6.46, df=1 and 151, p=.01) were reduced in the PARC cohort compared with the treatment-as-usual cohort, whereas the costs of psychiatry (F=60.22, df=1 and 151, p<.001) and nursing (F=11.13, df=1 and 151, p=.001) visits were higher in the PARC cohort (
Figure 2). The cost of occupational therapy did not statistically differ between groups, given that PARC did not offer this service.
In the PARC cohort, ten patients were hospitalized during the study period. Of those, two were rehospitalized, for a total of three rehospitalizations. The total number of hospital days for the PARC cohort was 143. In the treatment-as-usual cohort, 22 patients were hospitalized during the study period. Of those, nine were rehospitalized, for a total of 16 rehospitalizations. The total number of hospital days for the treatment-as-usual cohort, when corrected for the difference between the two cohorts in days of treatment, was 213.
During the period from 2005 to 2011, global psychiatric hospitalization rates varied from .04 to .07 annually.
Discussion
This study compared EI service delivery and overall health service utilization and associated fees among patients at PARC and an FEP sample matched for age, sex, race, and diagnosis that received treatment as usual at a geographically similar facility. We found that there were no differences between the cost of outpatient clinic services utilized by the PARC and treatment-as-usual cohorts but that the PARC cohort utilized significantly fewer inpatient, psychiatric crisis, and emergency medical services, leading to lower acute service costs. Cost analyses reflected an estimated savings at PARC of over $6,900 per patient.
These savings are consistent with those reported by Mihalopoulos and others at Australia’s Early Psychosis Prevention and Intervention Center—approximately $7,000 AUD in the first year and $6,000 AUD annually over the first eight years (
8,
9)—and at the Parachute project in Sweden (
10). In both cases, lowered cost was driven by a reduction in inpatient services, which was offset to some degree by an increase in outpatient clinic services. Unlike those studies, however, our analysis showed a decrease in all acute service utilization without a compensatory increase in total outpatient clinic service use. Similarly, Goldberg and colleagues evaluated the impact of an EI service in Ontario, Canada, on acute service use and reported similar cost savings, although a time-series analysis of their data could not confirm that the reduction in cost was related specifically to introduction of the EI service, and outpatient service costs were not evaluated (
12).
Our results differed from those reported by McCrone and colleagues (
13) and by Hastrup and colleagues (
14) in the Lambeth Early Onset and OPUS trials, respectively. Both trials examined cost-effectiveness of EI services and found no difference between the total mean cost of EI and treatment-as-usual interventions. However, a substantial difference between those studies and our study is that both McCrone and colleagues and Hastrup and colleagues reported markedly higher rates of inpatient hospitalization compared with findings from our cohorts. This dissimilarity, which may reflect differences in health care practice patterns between our catchment area and the catchment areas studied in Denmark (OPUS) and the United Kingdom (LEO), might certainly lead to disparate findings from our own, given that the large inpatient costs in these studies may have offset any savings in costs for outpatient services. Our results also differed from those reported by Rosenheck and others (
15), who evaluated the cost-effectiveness of the Recovery After an Initial Schizophrenia Episode–Early Treatment Program (RAISE-ETP) Navigate intervention in a randomized, controlled, multisite study in the United States. They found the intervention to be more costly compared with treatment as usual, although the additional cost was offset in their cost-effectiveness evaluation by improvements in quality of life and symptoms.
In contrast to prior assessments of EI service cost, this study also evaluated the utilization of specific mental health services in order to assess the relative significance and cost burden of each service. Although overall outpatient clinic service utilization by PARC and treatment-as-usual patients did not differ, PARC patients saw their physicians and nurses at higher rates. Although these visits accounted for a large portion of the outpatient clinic costs and psychiatrist and nursing costs were substantially higher in the treatment-as-usual cohort compared with the PARC cohort, the overall expense of outpatient clinic treatment was not increased for the PARC cohort compared with treatment as usual. This suggests that providing medical management via physician and nurse visits, rather than other services that were much more frequently utilized in the treatment-as-usual cohort, contributed more substantially to the overall decrease in acute service utilization and resultant costs.
That is not surprising, given that treatment at PARC emphasizes frequent physician and nurse visits in order to focus on antipsychotic medication use and adherence with a goal of decreasing illness relapse rates. Given that nonadherence to treatment accounts for approximately 40% of the hospital readmissions of patients with schizophrenia (
3) and has been estimated to account for nearly $1.5 billion annually in direct costs (
16), attention to treatment adherence is critical. In addition to promoting an emphasis on medication adherence, an increased frequency of contacts with physicians—the EI team clinicians who are most able to institute rapid changes to treatment—presumably improves the ability to provide both early detection and quick intervention for illness relapses, preventing utilization of higher-cost services in many cases. Although a thorough evaluation of patient outcomes is beyond the scope of this study, lower rehospitalization rates and fewer total hospital days in the PARC cohort supported this conclusion.
A potential limitation of this study was its retrospective nature; however, the two cohorts were well matched and captured the entire sample of patients with nonaffective FEP who were treated within the second-largest community mental health center in the country over a period of several years. Both samples were drawn from the same geographic area and received their care within the same health care system. Participants in the PARC cohort had fewer days of treatment than the treatment-as-usual cohort, so this variable was used as a covariate to adjust the analysis accordingly.
The difference in the time epochs during which data collection was undertaken was a potential limitation, although there was overlap in the data collection periods for a number of patients. (Several patients in the treatment-as-usual cohort were receiving treatment during the data collection period for the PARC cohort). Although a contemporary sample could have been chosen from outside the health care system, we believe that the practice pattern differences between two health systems are likely to be more substantial than those within the same health system over a fairly circumscribed time period (in this case, six years). Throughout that period, the clinical and administrative leadership at the Eskenazi Health Midtown system was unchanged, the availability of acute services remained consistent, and practice patterns were fairly static. In addition, a review of the global psychiatric hospitalization rates, representing the likelihood that an individual presenting for emergency treatment would be hospitalized, revealed little variability throughout this period. An additional benefit of working with cohorts within the same system included access to the Regenstrief Medical Record System for both samples, allowing for review of health service utilization data from most of the major mental health and nonpsychiatric medical providers in the large metropolitan area and capturing health service utilization data across multiple service delivery sites and systems. However, one further limitation was that local charges were used as a proxy for cost. This limited the ability to generalize gross dollar amount savings to other settings.
Although health care trends often favor services delivered by nonphysician providers over physician encounters, in part to decrease costs, the balance of services provided at PARC—specifically, a higher frequency of physician and nursing visits—ultimately reduced the overall cost of care for FEP individuals.
Conclusions
The findings in this study indicate not only that EI services result in cost savings but that a focus on increasing medical services may be key in reducing the use of acute services, presumably because of a reduction in psychiatric and nonpsychiatric medical pathology. Future evaluation of other outcomes of this EI population besides use of services would further validate these findings. If replicated, these findings could support changes in public health policy to increase support for EI. In particular, increased reliance on the medical management of psychosis may confer particular benefits, significantly improving the lives of individuals with psychosis while providing an opportunity for reduced health care expenditures.