Obesity prevalence is nearly double among people with serious mental illness compared with the general population (
1,
2). Obesity is also a major contributor to cardiovascular disease and the resulting significantly reduced life expectancy for individuals with serious mental illness (
3). Among people with serious mental illnesses, achieving meaningful reduction in cardiovascular risk requires not only significant and sustained changes to modifiable risk factors such as poor diet and sedentary behaviors but also overcoming challenges such as poverty, metabolic effects of psychoactive medications, and the impact of symptoms on motivation (
4). Young adulthood represents a critical time to address this early mortality disparity because even though young adults are at greatest risk of gaining weight (
5), they are also poised to experience lasting benefits through participation in lifestyle interventions by learning and adopting positive habits that they can carry forward across the lifespan.
Young people with serious mental illness are at risk of substantial weight gain as a result of mental illness onset and its consequences on life functioning and motivation, as well as the initiation of some antipsychotic treatments (
6). Recent reports have documented the high prevalence of cardiometabolic risk factors among young people with first-episode schizophrenia spectrum disorders (
7) as well as the elevated risk of cardiovascular disease among young people with bipolar disorder and major depressive disorder (
8). A review found that young people with serious mental illness were more likely than young people in the general population to engage in poor lifestyle habits such as eating more high-fat foods and getting less exercise, resulting in elevated risk for long-term general medical problems, including cardiovascular disease and diabetes (
9). However, there is limited research on the effect of lifestyle interventions targeting weight loss among overweight and obese adults age 30 and under who have a serious mental illness, such as a schizophrenia spectrum disorder or a mood disorder.
For young adults in the general population, recent systematic reviews of lifestyle interventions targeting weight loss have found that the effectiveness of these efforts has been variable (
10,
11). For example, prior studies have been limited by small sample sizes, short intervention periods, homogeneous samples, and elevated participant attrition (
12). Research findings also suggest that these mixed findings are partly attributable to challenges with engaging this age group in services, as well as to the predominant focus in prior research on childhood obesity or on developing interventions for middle-aged adults that may not appeal to the interests and unique lifestyles of young adults (
12).
Among adults with serious mental illness, there is increasing evidence to support the effectiveness of behavioral interventions promoting fitness and healthy eating for weight loss (
13). A series of randomized controlled trials of different lifestyle interventions has demonstrated the effectiveness of these programs for achieving clinically significant weight loss—5% or greater—or reducing cardiovascular risk for as many as half of participants with serious mental illness (
14–
17). However, across these recent studies, the impact of lifestyle intervention on outcomes among young adults has not been specifically examined and therefore remains unclear. Prior studies have also demonstrated that behavioral interventions can lessen antipsychotic-induced weight gain during illness onset among young adults with serious mental illness who are initiating treatment (
18–
20). Less clear, however, is whether overweight or obese young adults with serious mental illness who are receiving stable pharmacological treatment can achieve meaningful health benefits, including weight loss, improved fitness, and reduction in cardiovascular risk through participation in a lifestyle intervention.
This study examined the impact of the 12-month In SHAPE lifestyle intervention on weight loss and fitness among overweight and obese young adults with serious mental illness who were ages 21 to 30 compared with adults over age 30. Secondary outcomes, including change in body mass index (BMI), waist circumference, physical activity, blood pressure, and lipid levels and program adherence, were also compared between the two age groups. The primary aim was to determine whether young adult participants with serious mental illness would lose weight, improve fitness, and achieve reduced cardiovascular risk at levels comparable with those of participants over age 30.
Methods
This study used combined data for 194 participants with serious mental illness who received the In SHAPE lifestyle intervention and who completed baseline and follow-up assessments across three separate clinical trials. The trials included a randomized trial of 133 persons with serious mental illness who participated in the In SHAPE program or who had a gym membership from April 2007 to November 2011 in Concord, New Hampshire (
14); a randomized trial that compared 210 persons with serious mental illness who participated in In SHAPE or who had a gym membership from April 2008 to May 2013 in Boston (
15); and a trial with 122 persons with serious mental illness who participated in In SHAPE implemented in two community mental health centers or who received usual care in two additional centers from December 2009 to March 2013 in rural and urban settings in New Hampshire. Forty participants who completed baseline but not 12-month assessments were not included in this analysis. These individuals did not differ on any baseline characteristics from participants (N=194) who completed the study.
All participants had a serious mental illness, defined by an axis I diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder, and persistent impairment in multiple areas of functioning (such as work, school, or self-care); were age 21 or older; had a BMI greater than 25, indicating excess weight; were on stable pharmacological treatment, defined as receiving the same psychiatric medications over the prior two months; and provided informed consent for participation. Study procedures were approved by Committees for the Protection of Human Subjects at Dartmouth College and specific to each site.
In SHAPE Program
The 12-month In SHAPE lifestyle intervention consists of a gym membership, weekly individual meetings with a certified fitness trainer, and instruction on healthy eating and nutrition. The fitness trainers are trained in tailoring individual wellness plans to the needs of people with serious mental illness and complete a one-week In SHAPE training course consisting of instruction in motivational interviewing, fitness goal setting, nutrition, tracking eating and exercise, and strategies for health behavior change, such as addressing mental health symptoms that interfere with exercise and healthy eating. Participants obtained medical clearance from their primary care provider to enroll in the In SHAPE program. At the start of the program, the fitness trainers conducted lifestyle and fitness evaluations to develop personalized fitness plans for each participant and to use shared goal setting. The fitness trainers delivered the In SHAPE program according to a standardized protocol. For the program duration, fitness trainers met with participants individually each week for 60 minutes at a local gym (YMCA). Each weekly session consisted primarily of fitness coaching, support, and reinforcement for exercise, followed by individualized nutrition education for at least 15 minutes, which emphasized a balanced diet, portion control, and healthy eating on a budget. To ensure fidelity to the In SHAPE program, the fitness trainers received weekly supervision from a health psychologist, a personal fitness trainer, and a registered dietitian.
Measures
Trained research interviewers collected several outcome measures at baseline and 12 months.
Weight.
Change in body weight was measured in pounds. The proportion of participants who achieved clinically significant weight loss of ≥5% and ≥10% was calculated because modest weight loss, in this range, contributes to reduction in cardiovascular risk among overweight and obese individuals (
21,
22).
Fitness.
Change in fitness was assessed with the 6-Minute Walk Test (6-MWT), which measures the distance that an individual can walk in six minutes and is a reliable and valid measure of fitness (
23). The proportion of participants who achieved clinically significant improvement in fitness, defined as an increase in distance of >50 m (about 164 feet) on the 6-MWT, was also calculated because this improvement is associated with reduced cardiovascular risk (
24).
Secondary obesity measures.
Change in BMI, calculated as weight (kg)/height(m)2, and change in waist circumference, measured in inches, were reported.
Physical activity.
Change in total physical activity was measured with the short-form International Physical Activity Questionnaire, which is a reliable and valid measure of physical activity among people with serious mental illness (
25).
Blood pressure and lipid levels.
Blood pressure was measured after participants completed the 6-MWT. Lipid levels were measured with the CardioChek PA Analyzer, a portable testing system that produces reliable values for total cholesterol, low-density lipoprotein, high-density lipoprotein, and triglycerides (
26).
Program adherence and retention.
Adherence was measured as the number of sessions with the fitness trainer, out of 50 planned visits, over the 12-month intervention period. Study retention was defined as completion of the 12-month assessment.
Psychiatric medications.
Participants’ medication use was assessed because different antipsychotic agents are associated with varying degrees of weight gain (
27,
28) and are known to affect ability to lose weight (
2). Participants’ antipsychotic medications were classified as having a high (including olanzapine and clozapine), medium (risperidone), or low (ziprasidone) propensity for associated weight gain. Change in psychiatric medication use and the medication’s weight gain propensity was also examined because medication changes can interfere with ability to lose weight (
6).
Statistical Analysis
Young adult participants (ages 21–30 years) were compared with participants over age 30 at baseline on demographic characteristics, obesity measures, fitness, blood pressure, lipid levels, and use of antipsychotic medications and on their psychiatric medications’ propensity to lead to weight gain. Chi-square tests were used for categorical variables, and t tests were used for continuous variables. Linear regression models were used to compare young adult participants and participants over age 30 at 12 months on continuous outcome variables, including primary outcomes of weight loss and fitness and secondary measures of obesity, physical activity, blood pressure, and lipid levels. Logistic regression models were used to compare the age groups on binary outcomes of whether the participant lost weight compared with baseline weight, achieved ≥5% weight loss, achieved ≥10% weight loss, showed improved fitness (>50-m increase on the 6-MWT), or achieved reduced cardiovascular risk (≥5% weight loss or >50-m increase on the 6-MWT) at 12 months. All regression models controlled for study (trial 1, 2, or 3), gender, diagnosis, race-ethnicity, and level of program adherence. A value of p≤.05 was considered significant. All statistical analyses were performed in 2015 with Stata 14.0 software.
Results
Participants’ baseline characteristics are listed in
Table 1. Greater proportions of young adult participants compared with participants over age 30 were living in supervised or supportive housing and were either never married or were currently married. Young adults also had higher levels of fitness at baseline. Other demographic characteristics, physical activity, smoking status, obesity measures, blood pressure and lipid levels, and use of antipsychotic medications did not differ between age groups at baseline.
At 12 months, the overall sample showed significant mean±SD weight loss of 4.37±19.20 pounds (p=.002 for pre-post change) and significant improvement in fitness, as reflected by an increase on the 6-MWT of 59.89±228.98 feet (p=.002 for pre-post change). As highlighted in
Table 2, there were no significant differences in outcomes between age groups. Although these results were not statistically significant, average weight loss and average BMI reduction were greater for participants over age 30 compared with young adults.
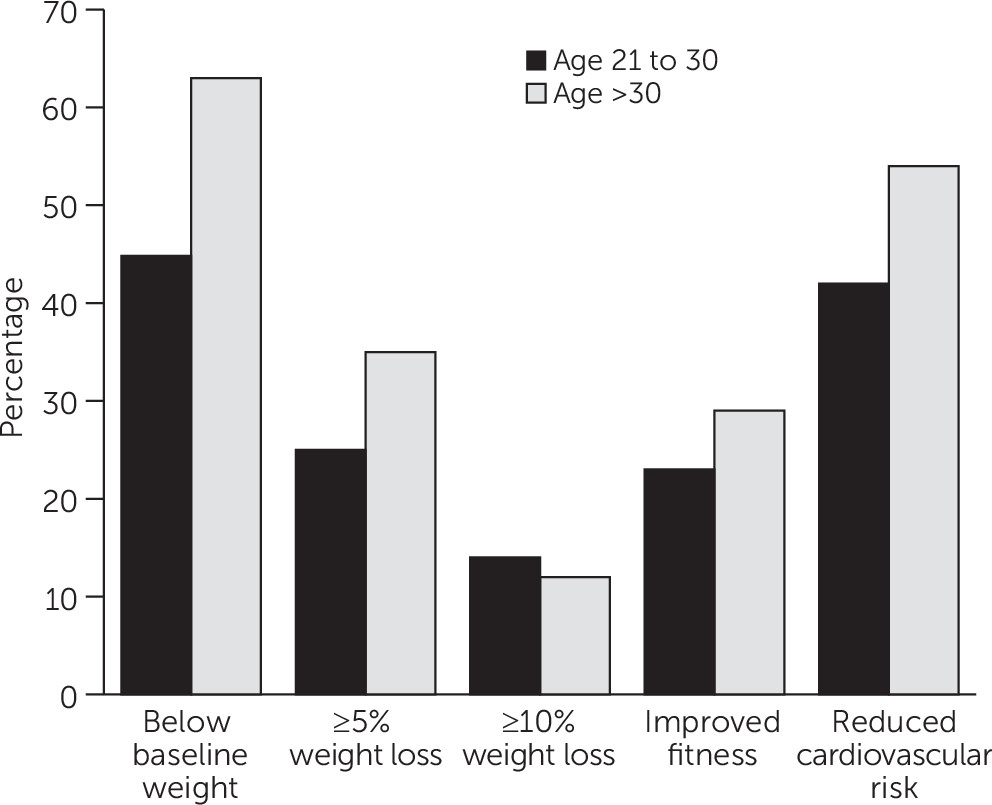
Figure 1 illustrates the proportions of participants in both age groups who lost weight or who achieved clinically significant weight loss, improved fitness, or cardiovascular risk reduction. At 12 months, a greater proportion of participants over age 30 compared with young adults were below their baseline weight, achieved ≥5% weight loss, and showed improved fitness and cardiovascular risk reduction; however, none of these differences were statistically significant. Nearly half (45%) of young adult participants were below their baseline weight, 25% achieved ≥5% weight loss, 14% achieved ≥10% weight loss, and 23% showed clinically significant improved fitness based on a >50-m increase on the 6-MWT. Overall, 42% of young adult participants (compared with 54% of participants over age 30) showed clinically significant cardiovascular risk reduction, defined as either clinically significant weight loss or improved fitness (the difference was not statistically significant).
Study attrition did not differ between young adults (17%) and participants over age 30 (17%). Adherence to the In SHAPE intervention, measured as session attendance with the fitness trainer out of a possible 50 sessions over the 12-month study period, was comparable between age groups. On average, young adults attended 27.0±14.4 sessions compared with 29.2±13.5 sessions for participants over age 30. There were no differences in medication changes between the groups.
Discussion
This study showed that overweight and obese young adults with serious mental illness were able to achieve clinically significant benefits through participation in the In SHAPE lifestyle intervention. At 12 months, 42% of young adult participants achieved reduction in cardiovascular risk, defined as ≥5% weight loss or >50-m increase on the 6-MWT. Although average weight loss and average BMI reduction were greater among participants over age 30 than among young adults, these differences were not statistically significant. These findings expand on existing efforts to prevent weight gain among young adults with serious mental illness (
18,
19) and show promise for offering behavioral weight loss interventions to overweight and obese young adults in community mental health settings.
Another important finding was that neither attrition nor program adherence differed between age groups. This finding suggests that when young adults with serious mental illness enroll in a lifestyle intervention, they are as motivated as participants over age 30 to continue participating throughout the 12-month program. This finding is in contrast to findings of many prior studies of standard behavioral weight loss treatment consisting of education and didactic instruction in the general population, in which young adults seemed reluctant to participate or sustain involvement in programs over time (
11).
Benefits of the In SHAPE lifestyle intervention among young adults with serious mental illness may be due to the emphasis on physical activity through the use of personalized health coaching sessions with a fitness trainer at a fitness facility located outside of the mental health center, which is consistent with research from the general population showing that young adults prefer physical activity over other methods for losing weight (
29). In addition, research has shown that young adults respond well to emotional support for weight loss (
29). The personal connection and support provided by the fitness trainers, who were mostly young adults themselves, in the In SHAPE program may have been especially motivating for young adult participants with serious mental illness. For example, during weekly meetings with participants, the fitness trainers helped participants to develop individualized fitness plans, supported personal goal setting, and suggested strategies for overcoming mental health symptoms that interfered with healthy eating or exercise, which may have promoted engagement with the program (
30).
The findings are promising in that 45% of young adult participants in the In SHAPE program were below their baseline weight at 12 months given the substantial risk of weight gain observed in this group. This result suggests that a lifestyle intervention delivered through community mental health settings may benefit both younger and older groups of adults. These findings could also inform continued efforts needed to target the young adult participants who were not successful at losing weight. Approaches that appeal specifically to the unique interests, perspectives, and attitudes of young adults with serious mental illness and that focus on sensitive issues for young people, such as self-esteem and body image (
31), may afford added impact. For example, lifestyle interventions for young adults with serious mental illness could promote the benefits of adopting a healthy lifestyle to look and feel good while offering opportunities to socialize and have fun (
12,
29). Interventions targeting this group could also include brief education about the role of psychiatric medications and weight gain and provide training on how to talk to mental health providers about weight gain from psychotropic medications (
4,
6).
Emerging mobile and online technologies may also offer advantages for promoting and supporting weight loss and fitness among young adults with serious mental illness (
4). Popular social media and smartphone technologies are increasingly becoming part of the daily lives of young people with serious mental illness (
32) and may afford new opportunities for delivering scalable interventions capable of reaching and engaging these individuals at their own convenience (
33). In the general population, Facebook has been successfully used to support weight loss among college students (
34), and hybrid approaches using Facebook, text messaging, and smartphone applications appear promising for promoting engagement and retention in behavioral weight loss efforts for young adults (
35). Recent preliminary pilot studies have highlighted the feasibility, acceptability, and potential effectiveness of supporting lifestyle interventions for people with serious mental illness by using Facebook, smartphone technologies, and wearable activity tracking devices (
36,
37). However, use of these technologies for specifically targeting and supporting behavioral weight loss among young adults with serious mental illness has not yet been explored.
Several limitations warrant consideration. First, all participants were receiving services at community mental health centers, indicating that these findings may not be generalizable to individuals with serious mental illness not receiving treatment. Second, nearly 70% of the sample was non-Hispanic white, which may limit generalizability across diverse racial or ethnic groups. Third, fewer young adult participants received the In SHAPE lifestyle intervention compared with participants over age 30. This may have increased the risk of type II statistical error (that is, failure to detect an effect that was present).
Conclusions
As young people with mental illness grow older, they often experience a decline in physical function and risk developing serious medical conditions resulting from the cumulative impact of obesity, poor health behaviors, low socioeconomic status, and effects of living with mental illness on motivation and personal well-being (
9). Efforts are urgently needed to alter this trajectory and to support young adults with serious mental illness as they develop behavioral patterns and habits and learn to balance their mental health symptoms with life demands and pursuits. Drawing from the findings presented here, future lifestyle interventions must specifically target weight loss and fitness among overweight and obese young adults with serious mental illness, so that these individuals can build confidence, learn necessary skills, and adopt healthy behaviors that may decrease the significant early mortality gap affecting this high-risk group.