Among U.S. children and adolescents, the estimated prevalence of psychiatric disorders has risen to 13%−20% (
1,
2), with recent studies identifying mental illness as one of the five most common pediatric conditions (
3), as well as the most expensive (
4). The presence of community risk factors, such as poverty and violence, contributes to higher prevalence rates—as high as 25%—in vulnerable populations (
5). Despite high need, only one in five U.S. children with a mental or substance use disorder receives treatment (
6). Race- and class-based disparities in health care quality delay identification of the needs and timely treatment of people with mental or substance use disorders, which in turn contributes to a greater burden of illness for both children and adults, particularly those who have been exposed to adverse childhood experiences (
7).
In addition, chronic general medical conditions, which are thought to co-occur among 60% of children with mental disorders, may present further challenges (
8,
9). The presence of mental or substance use disorders, in children or parents, can complicate treatment of routine medical conditions and contribute to greater levels of morbidity. Moreover, because the prevalence of psychiatric conditions has increased without symmetrical growth in workforce capacity, pediatricians have struggled with their growing responsibility for managing psychiatric needs within primary care.
Despite increased mental and substance use disorder screening efforts in primary care for youths who receive Medicaid (
10), children continue to face insufficient access to treatment for mental or substance use disorders (
11), with a disappointingly high percentage of no-shows (40%) reported for psychiatry evaluations even when specialty referrals were made (
12). Case studies and meta-analysis have shown the benefits of integrated medical-behavioral primary care in improving child mental or substance use disorder outcomes (
13,
14). Integrated teams develop a shared practice (
15,
16) and are designed to reduce barriers to care.
Implementation of new outcome-based reimbursement, consistent with health care reform (
17,
18), provides an opportunity to pilot integrated care for children via a collaborative-practice model (CPM). The CPM is designed to foster interdisciplinary collaboration between mental health and primary care (
19), use continuity of intent (
20) to improve family engagement (
21), and address social determinants of health.
The primary objective of this study was to examine treatment access and engagement outcomes for the CPM.
Methods
We hypothesized that providing highly integrated outpatient child psychiatry consultation to primary care pediatricians, combined with peer-to-peer parent support and outreach, would be associated with improved treatment access and engagement for at-risk youths compared with usual care. We tested this hypothesis by means of a quasi-experimental design in which youths meeting inclusion criteria were nonrandomly selected at the clinic level to receive either the CPM intervention or usual care.
Sample and Setting
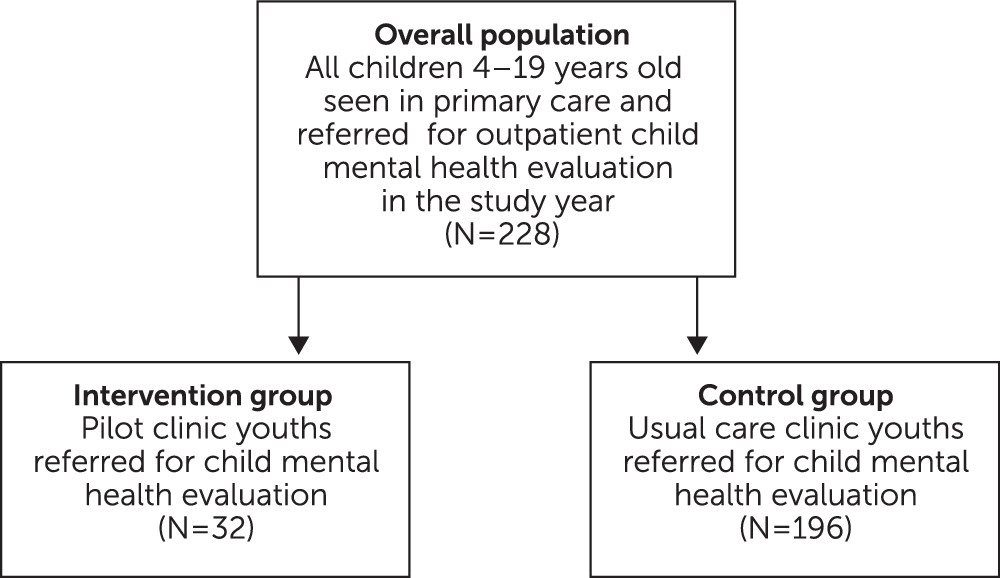
The study sample consisted of 228 youths (ages four to 19 years) referred for child psychiatric evaluation in 2013 (
Figure 1). All youths received primary care in a safety-net health system, serving a mostly Medicaid-insured population.
Eligibility for Intervention Group
The CPM program was piloted in one of eight pediatric clinics. The CPM group included all youths at the pilot clinic referred by primary care for psychiatric evaluation (N=32). Informed consent for participation was obtained from referred families.
CPM Team
The CPM brings inpatient child psychiatry consultation-liaison elements, such as team-based rounds, to an outpatient setting. Child psychiatry and family support specialist (FSS) staff were available weekly in the pediatrics clinic. FSS staff were nonclinician parents with lived experience caring for a child with mental or substance use disorder needs. They received training in how to assist with child and family evaluations and to provide peer-to-peer support. The FSS role in the CPM was bidirectional: bringing a family perspective to interactions with clinicians, for whom they translated families’ concerns while also explaining and reinforcing the team’s recommendations to families. FSS staff foster engagement via parent interviews, active follow-up, and home visits. These activities, in turn, inform FSS communications to the clinical team.
CPM Process
At the pilot site, CPM team members developed new processes to facilitate integration of clinical care. Innovations included the following: child mental health specialists joining pediatrics team “huddles,” psychiatry notes shared with pediatricians via the electronic health record (EHR), and active inclusion of pediatricians in preevaluation discussions with the CPM team and postevaluation recommendations for the family. CPM evaluations were conducted by the paired specialty team of a consulting child psychiatrist and an FSS. This pairing allowed for separate, multifaceted assessment of parent and child, along with a joint session to deliver recommendations, effectively combining in one visit what often requires three visits for a solo clinician to accomplish.
The CPM clinical intervention was individualized for each child on the basis of team-identified needs and level of treatment intensity and youth and family preferences. However, the intervention reliably included basic elements: weekly onsite sessions at the pediatrics clinic for the paired specialty team to provide “curbside” (indirect) or face-to-face (direct) consults to primary care providers (PCPs); ongoing clinical collaboration (“shared practice”) between child psychiatry and pediatrics before, during, and after an evaluation; and, when needed, communication with school personnel, child welfare, and community-based resources.
Control Group
The primary care mental or substance use disorder screening process for youths in the control group at the usual care clinics (N=196) was the same as that at the pilot clinic. Similarly, pediatricians could make referrals to child psychiatry for evaluations via the EHR and receive messages from psychiatry intake staff regarding scheduling efforts. As in the intervention group, youths in the control group were evaluated by child psychiatry attending physicians and the same child psychiatry fellows who rotated through the CPM clinic, but the encounters took place in psychiatry offices on a separate campus away from primary care sites, and no FSS team members were present. Documentation by the psychiatrists was entered in the EHR but, as a result of confidentiality protocols in place at the time, was typically inaccessible to pediatricians. Control group data on referrals for psychiatric evaluation were extracted from the EHR, deidentified, and transferred to the research team via an institutional review board–approved protocol.
Variables
Two outcome measures were assessed: treatment access and treatment engagement. Treatment access was a dichotomous variable defined as whether youths received a psychiatric evaluation. Treatment engagement was also dichotomous and was defined as whether youths participated in one or more follow-up activities recommended postevaluation. Recommendations fell into four groups: individual therapy, family therapy, psychotropic medication, and other.
The primary independent variable indicated membership in the CPM group versus the control group. Other covariates were age, gender, race-ethnicity, language (self-identified), and diagnosis, all extracted from EHR data. Age was continuous, ranging from one to 19 years. Gender was defined as female or male. Race-ethnicity was coded as Hispanic (including Brazilian), non-Hispanic black, non-Hispanic white, and non-Hispanic other. Language preference was coded as English, Spanish, or other. EHR diagnoses were recoded into the four most frequent categories: anxiety, mood, attention-deficit hyperactivity disorder, and other. Because diagnosis was determined by psychiatric evaluation, the 42 patients who did not complete an evaluation had no diagnosis. All referrals were included in analysis of access, but only youths with diagnoses were included in analysis of treatment engagement.
Analysis
Statistical analysis proceeded sequentially, matching the nested structure of the study design and outcome measures. Only youths who accessed evaluation, the first outcome, were eligible to be assessed for treatment engagement, the second outcome. The analytic samples were therefore different for each outcome (treatment access, N=228; treatment engagement, N=186).
Descriptive statistics were generated to compare outcomes and covariates between the two treatment groups (
Table 1). Because treatment was nonrandomly assigned at the site level, we expected to find significant differences between groups on many variables. Depending on how each variable was distributed, statistical significance of differences between groups was tested using t tests, chi-square tests, and Fisher’s exact test. In both the access and the engagement samples, the CPM and control groups were significantly different on all covariates except gender (the treatment engagement sample included diagnosis).
To address confounding due to nonrandom treatment assignment, we estimated propensity-score weights balancing the CPM and control groups on pretreatment attributes, using all available covariates. Propensity scores were estimated using a nonparametric generalized boosted regression technique that has been used with good results in other recent studies of adolescent behavioral health interventions (
22,
23). We computed the average treatment effect on the treated population, weighting members of the control group so that they more closely matched the CPM group on pretreatment covariates. After applying propensity-score weights, the treatment groups were no longer significantly different on any of the covariates (
Table 1).
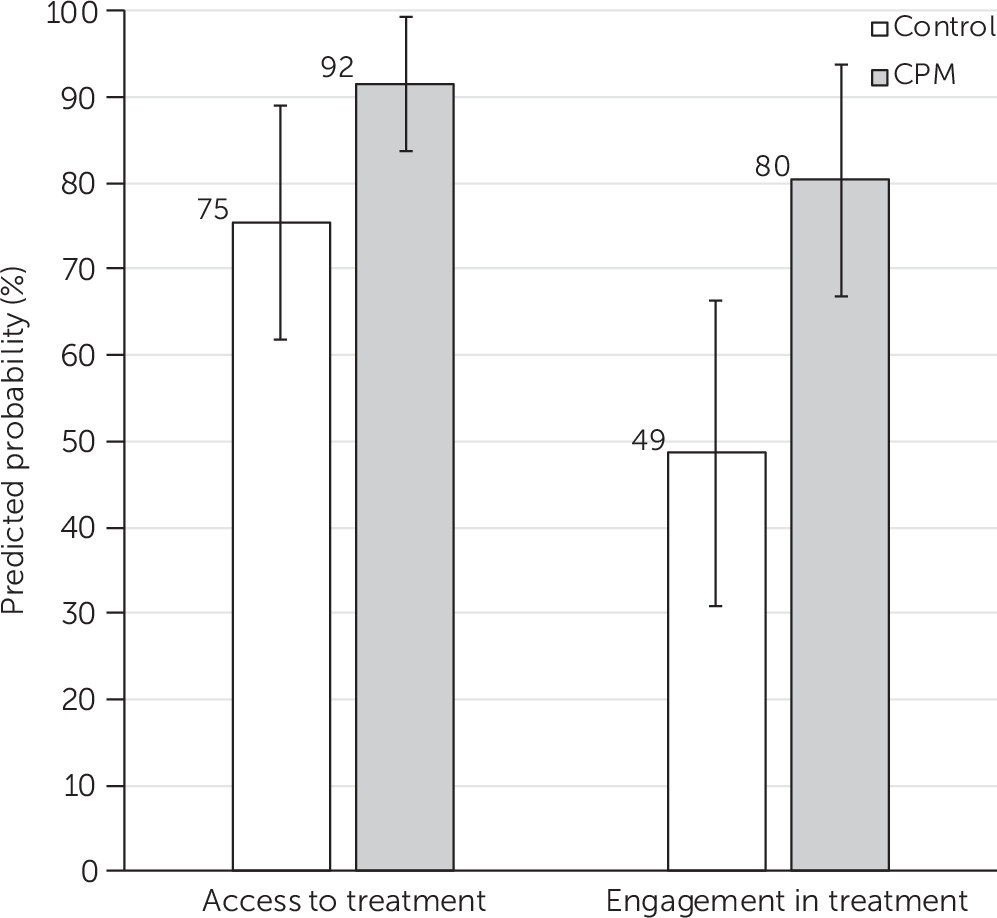
To answer the main research question of the study—whether the CPM intervention would be associated with higher rates of treatment access and engagement than usual care—we fit propensity-score–weighted logistic regression models estimating the likelihood of each outcome, with treatment group as the independent variable of interest. We specified unadjusted and adjusted models for both outcomes (
Tables 2 and
3), with the adjusted models controlling for the same covariates used to generate the propensity-score weights. After fitting the adjusted models, we also computed predictive margins to show in terms of probability the average effect of CPM on both outcomes (
Figure 2).
Results
Descriptive differences in sample characteristics and outcomes between treatment groups are shown, before and after propensity-score weighting, in
Table 1. Among the 228 youths referred by pediatrics for psychiatric evaluation, 32 were referred from the CPM pilot clinic and 196 were referred from the seven usual-care clinics (
Figure 1). Of the 186 youths who accessed a psychiatric evaluation, 29 were from the CPM group and 157 were from the control group. Before applying propensity-score weights, we found no statistically significant difference between groups in evaluation access rates. On average, compared with the control group, the CPM group was significantly older (p<.001), with a mean±SD age of 13.1±4.9 years old versus 8.7±3.6 years old, and was significantly more likely to be Hispanic (63% vs. 47%) or black (25% vs. 19%) and less likely to be white (3% vs. 29%), (p<.01). Compared with the control group, the CPM group was significantly more likely to speak Spanish (41% vs. 10%) and less likely to speak English (56% vs. 71%) (p<.001). Both groups were majority male. After applying propensity-score weights, none of the differences in covariates between the treatment groups remained significantly different.
Among the 99 youths who engaged in treatment, 23 were from the CPM group and 76 were from the control group. Before propensity-score weighting, CPM group youths were significantly more likely to engage in treatment than control group youths (79% vs. 48%; p<.01). As in the sample who accessed treatment, youths receiving the CPM intervention were significantly older (p<.001) and were more likely to be Hispanic or black and less likely to be white (p<.05). They were also more likely than the control group to speak Spanish and less likely to speak English (p<.01). The treatment groups were also significantly different in terms of diagnosis (p<.01). Mood disorders were most common in the CPM group (41%), whereas anxiety disorders were most common in the control group (36%). After propensity-score weights were computed and applied, no covariates remained significantly different between treatment groups (see
Table 1.)
All regression model results are shown in
Table 2 (treatment access) and
Table 3 (treatment engagement) and were estimated with propensity-score weights applied. In the unadjusted model, the odds of achieving treatment access were not significantly different between groups. After the model was adjusted for age, gender, race-ethnicity, and language, however, a significant difference emerged, with members of the CPM group having more than four times greater odds of accessing treatment than the control group (adjusted odds ratio [AOR]=4.16). This translated into significantly different predicted probabilities of treatment access for each group: 92% for youths in CPM versus 75% for youths receiving usual care (p<.05;
Figure 2).
For the treatment engagement outcome, results from the unadjusted model indicated marginally significant greater odds of engagement for youths in CPM compared with those in the control group (OR=3.35). After the model was adjusted for age, gender, race-ethnicity, language, and diagnosis, however, the difference increased in magnitude and became highly significant: The odds of engagement for the CPM group were more than seven times higher than those for the control group (AOR=7.54). In terms of predicted probabilities, about 80% of youths in CPM who completed psychiatric evaluation would be expected to engage in further recommended care compared with 49% of youths receiving usual care (p<.01;
Figure 2). Therefore, conditioning engagement on access, about 74% of all youths receiving a referral for a psychiatric evaluation via the CPM intervention would be expected to complete the referral and engage in recommended follow-up treatment compared with about 37% of youths receiving a referral under usual care conditions.
Discussion
Social factors associated with poverty, such as parental illness, transient housing, and legal issues, can present impediments to diagnosis and management of chronic illness among children, including mental illness (
24). In this study, the CPM intervention was designed to address these challenges, weaving together elements of integrated child psychiatry consultation with community-based FSS, to create a more patient-centered delivery system for at-risk youths. Findings of significantly higher rates of access and engagement associated with the CPM intervention than with usual care lend preliminary support to the hypothesis that a family-centered, integrated approach can reduce treatment barriers in a population at risk for health disparities (
25).
Although child psychiatry evaluations involving multidisciplinary teams were also available to the control group population, one explanation for the higher rates of access and engagement in the CPM group could be that the initial locus of care for evaluation was in the familiar pediatric care setting. Families reported great trust in their PCPs; this relationship could have contributed to sharing of key information with the CPM team and the building of a connection that facilitated treatment initiation. The FSS role was crucial; family history and current stressors identified by the FSS would not otherwise have been known to the team. These details aided the development of individualized treatment recommendations that were more likely to be endorsed by the family. The jointly created treatment plan, developed with the PCP, the parent, and the child, was then written down and provided to the parent, along with contact information. The fact that treatment engagement was sustained even after care was transitioned to other clinicians indicates the need for further research to confirm whether there is a CPM effect that persists after the team’s evaluation.
Clarifying the right diagnosis for youths with complex health care needs is a crucial step in efficient care delivery. Active involvement of child psychiatrists in the initial process of triaging consultation requests may be one reason why access and engagement rates were higher for the CPM model. Because the pilot population was known to face access barriers, the CPM team recognized that they might get only one opportunity to assess the child’s psychiatric diagnosis and treatment needs and share them with the family. They thus attempted to compress the objectives of multiple usual care visits into one CPM visit. Trainees who worked in both intervention and usual-care clinics observed that the CPM evaluation process was more intensive. They saw this as the result of active partnership among child psychiatry, FSSs, families, and pediatricians and noted that the shared approach to evaluation contributed to continuity of intent with regard to treatment planning.
Additional mechanisms for increased treatment engagement may include the following: achievement of a high level of diagnostic clarity sooner, which helps children get appropriate treatment; brief interventions onsite at the primary care clinic, with follow-up advice for pediatricians and families, strengthens recommendations; and individualized hand-offs to treatment resources reduce the need for families to start over. Postevaluation contact may have served to further facilitate initiation of follow-up treatment. The integrated CPM team also created a culture within primary care of shared practice management of youths with complex needs, including those with comorbid general medical conditions.
Because this was a nonrandomized, quasi-experimental study, this research is subject to confounding factors that could have influenced the results. First, because sample selection and assignment to treatment were not randomized, compositional and contextual differences between treatment groups could account for some of the differences in outcomes that we observed. We were able to partially address this risk by propensity-score weighting the control group to achieve statistical balance with the intervention group across a limited but relevant set of pretreatment covariates. We simultaneously controlled for these covariates in multivariate regression models, yielding doubly robust estimates to the extent that at least one of the techniques was correctly specified (
26,
27). However, our set of covariates was relatively small, and additional unobserved confounders that we did not account for could remain.
Another potential limitation stems from the fact that treatment assignment took place at the site (i.e., pediatric clinic) rather than at the individual level. Although this approach was a strength in that it limited the potential for spillover effects, we cannot rule out the possibility that the pilot clinic implementing the CPM intervention was characteristically different from the remaining control group clinics in ways that gave youths treated in the pilot clinic a better chance of achieving treatment access and engagement regardless of intervention type.
In addition, our intervention group sample size was relatively small, limiting the precision of our estimates as well as our ability to test hypotheses about the degree to which the CPM may have been associated with different results for different subpopulations of youths needing psychiatric care. Nonetheless, our propensity-score weighted multivariate models revealed between-group differences that were statistically significant and large in magnitude; after holding other factors constant, the CPM was associated with youths being twice as likely to achieve both access to treatment and treatment itself.
Conclusions
These findings serve as preliminary evidence suggesting that the CPM for integrated pediatric care should be further studied to isolate potential causal effects on the odds that children and families will receive needed mental health treatment. Additional areas for future investigation include heterogeneity of effect among subpopulations and across delivery systems; effectiveness of substituting other child mental health clinicians into the child psychiatrist role (given workforce capacity) or coordinating with other resources, such as telephone-based child psychiatry consults; and the unique effects of the FSS role on CPM outcomes.