Modeling the Cost-Effectiveness of Interventions to Reduce Suicide Risk Among Hospital Emergency Department Patients
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
Triage and Case Identification
| Category | Point estimate | Range | Sourcea |
|---|---|---|---|
| Prevalence | |||
| Suicide risk status at time of index ED visit | |||
| High risk | 2.8% | Author calculation | |
| Low risk | 9.6% | Author calculation | |
| No risk | 87.6% | Author calculation | |
| Triage | |||
| Medical branch patientsb | 93% | 90%–97% | Author calculation |
| As a percentage of general ED population (study cohort) | 13.4% | 12.2%–14.6% | Author opinion and National Hospital Ambulatory Medical Care Survey (NHAMCS), 2008 (21), and NHAMCS, 2011 (22) |
| Hospitalized for medical reasons, no sign of suicidality | 7.04% | Author calculation | |
| No risk | 100% | — | Author calculation |
| Hospitalized for medical reasons, apparent self-injury | 4.5% | 2%–8% | Author opinion |
| High risk | 20% | 15%–25% | Author opinion |
| Low risk | 30% | 25%–35% | Author opinion |
| No risk | 50% | Author calculation | |
| Received medical treatment in ED | 88.46% | Author calculation | |
| High risk | 1.75% | .75%–2.75% | Author opinion and Parkland Hospital, 2015 (23) |
| Low risk | 8% | 6%–10% | Author opinion and Classen and Larkin, 2005 (35), and Parkland Hospital, 2015 (23) |
| No risk | 90.25% | 87.25%–93.25% | Author opinion and Boudreaux et al., 2016 (38) |
| Psych branch patientsc | 7% | 3%–10% | Personal communication, Claassen CA, 2016 |
| High risk | 7.5% | 5%–10% | Author opinion and personal communication, Claassen CA, 2016 |
| Low risk | 25% | 20%–30% | Author opinion and personal communication, Claassen CA, 2016 |
| No risk | 67.5% | 60%–75% | Author opinion and Boudreaux et al., 2016 (38) |
| Sensitivity and specificity | |||
| Medical branch, suicide screening | |||
| Sensitivity, high risk | 30% | 20%–40% | Author opinion |
| Sensitivity, low risk | 3% | 0%–6% | Author opinion |
| Specificity, no risk | 99% | 95%–100% | Author opinion |
| Medical branch, suicide risk assessment among those with positive suicide screening | |||
| Sensitivity, high risk | 95% | 90%–100% | Author opinion |
| Sensitivity, low risk | 66% | 50%–80% | Author opinion |
| Specificity, no risk | 50% | 40%–60% | Author opinion |
| Psych branch, suicide risk assessmentc | |||
| Sensitivity, high risk | 95% | 93%–97% | Author opinion |
| Sensitivity, low risk | 66% | 50%–80% | Author opinion |
| Specificity, no risk | 56% | 46%–66% | Pokorny, 1983 (24) |
| Sensitivity and specificity of identifying suicide risk among patients admitted to hospital from ED for medical reasons | |||
| Sensitivity, high risk | 100% | 100%–100% | Author opinion |
| Sensitivity, low risk | 100% | 100%–100% | Author opinion |
| Specificity, no risk | 50% | 40%–60% | Author opinion |
| Event probability: psychiatric hospitalization | |||
| Medical branch, positive suicide screen and positive suicide assessment | 35% | 25%–45% | Author opinion and Healthcare Cost and Utilization Project (HCUP), 2017 (32) |
| Psych branch, positive suicide assessment | 80% | 70%–90% | Author opinion and HCUP, 2017 (32) |
| Psych branch, negative suicide assessment | 10% | 5%–15% | Author opinion |
| Base costs | |||
| Medical ED visit | |||
| No risk; discharged alive | $675 | $25–$2,850 | Author opinion and HCUP, 2017 (32) |
| High risk or low risk; discharged alive | $890 | $25–$3,350 | Author opinion and HCUP, 2017 (32) |
| Psychiatric ED visit; discharged alive | $695 | $25–$2,950 | Author opinion and HCUP, 2017 (32) |
| Suicide risk assessment | $150 | $100–$200 | Author opinion |
| Medical hospitalization | |||
| No risk; discharged alive | $8,765 | $1,450–$33,500 | Author opinion and HCUP, 2017 (32) |
| No risk; died in hospital | $21,740 | $1,650–$104,000 | Author opinion and HCUP, 2017 (32) |
| High risk or low risk; discharged alive | $11,080 | $1,550–$49,500 | Author opinion and HCUP, 2017 (32) |
| High risk or low risk; died in hospital | $21,460 | $2,650–$123,000 | Author opinion and HCUP, 2017 (32) |
| Psychiatric hospitalization | |||
| Discharged alive | $5,875 | $1,050–$20,500 | Author opinion and HCUP, 2017 (32) |
| Died in hospital by suicide | $18,790 | $1,350–$85,000 | Author opinion and HCUP, 2017 (32) |
| Inpatient suicide treatment | $2,000 | Author opinion | |
| Death and reattempt rates | |||
| Death by nonsuicide manner (in 6 weeks)d | .02044% | WONDER online databases, 2017 (25) | |
| Probability of new suicide attempt (assuming no treatment) | |||
| High risk: 1st Markov cycle after index event | .048 | Author opinion and Qin and Nordentoft, 2005 (26) | |
| High risk: 2nd–4th Markov cycle (each) | .00038 | Author opinion and Qin and Nordentoft, 2005 (26) | |
| High risk: 5th Markov cycle | .00029 | Author opinion and Qin and Nordentoft, 2005 (26) | |
| High risk: 6th–9th Markov cycle (each) | .00020 | Author opinion and Qin and Nordentoft, 2005 (26) | |
| Low risk: no treatment: false negative (distributed by 6-week cycles) | 50% of high rate | Author opinion | |
| No risk | 0% | Author opinion | |
| Ratio of suicides to suicide attempts | 1:13 | Author opinion and American Foundation for Suicide Prevention, 2013 (27) and Centers for Disease Control (CDC) (28) | |
| Years of potential life lost per suicide | 24 | Author opinion and CDC (28) | |
| Interventions: uptake, outcomes, and costs | |||
| Usual care (UC) (also provided to patients who receive inpatient suicide treatment)e | |||
| Uptake (receiving any outpatient suicide treatment) | 35% | 10%–50% | Author opinion |
| Reduction in attempt and reattempt rate versus no treatment | 15% | 10%–20% | Author opinion |
| Costf | $340 | Author opinion and Centers for Medicare and Medicaid Services, 2016 (31) | |
| Postcards | |||
| Uptake | 100% | na | Carter et al., 2013 (11) |
| Reduction in attempt and reattempt rate versus UC | 45% | 35%–55% | Author opinion and Carter et al., 2013 (11) |
| Additional costg | $145 | $135–$500 | Author opinion and Carter et al., 2013 (11) |
| Telephone outreach | |||
| Uptake | 70% | 60%–80% | Author opinion and Vaiva et al., 2006 (12) |
| Reduction in attempt and reattempt rate versus UC | 34% | 25%–45% | Author opinion and Vaiva et al., 2006 (12) |
| Additional costh | $300 | $300–$900 | Author opinion and Vaiva et al., 2006 (12) |
| Cognitive-behavioral therapy | |||
| Uptake | 65% | 55%–75% | Author opinion and Brown et al., 2005 (13) |
| Reduction in attempt and reattempt rate versus UC | 50% | 40%–60% | Author opinion and Brown et al., 2005 (13) |
| Additional costi | $810 | $810–$2,000 | Author opinion and Brown et al., 2005 (13) |
Outpatient Suicide Interventions
Postcards.
Telephone outreach.
CBT.
Costs
Outcomes
Results
Cost-Effectiveness
Base case analysis.
| Treatment cost ($ per person) | Life-years (per person) | ||||
|---|---|---|---|---|---|
| Strategy | Total | Incremental | Total | Incremental | ICE ($ per life-year) |
| Usual care (reference) | 1,961.812 | 0 | .979321179 | 0 | — |
| Postcards | 1,960.454 | –1.36 | .979693574 | .000372395 | —a |
| Telephone outreach | 1,962.855 | 1.043 | .979565566 | .000244387 | 4,300 |
| Cognitive-behavioral therapy | 1,966.77 | 4.96 | .979584921 | .000263742 | 18,800 |
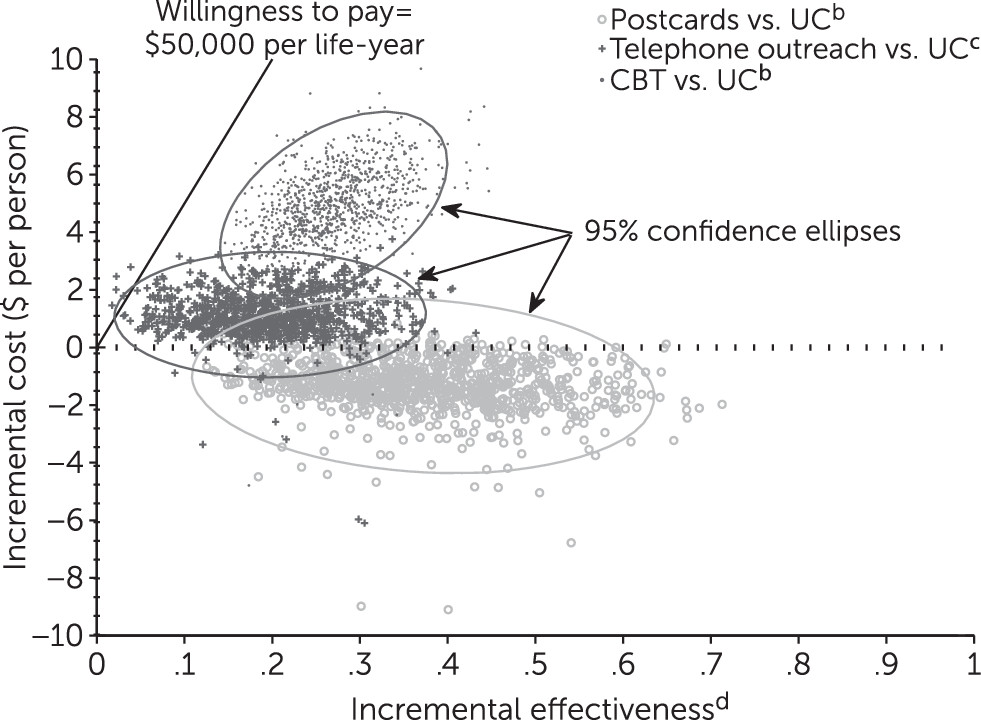
Monte Carlo simulation.
Sensitivity analysis.
| Strategy and cost of delivery ($) | Risk reduction relative to usual care (%) | |
|---|---|---|
| $50,000 | $100,000 | |
| Postcards | ||
| 135a | —b | —b |
| 270 | 3 | 2.5 |
| 500 | 7 | 4.5 |
| Telephone outreach | ||
| 300a | 6 | 3 |
| 600 | 16 | 9 |
| 900 | 26 | 14 |
| Cognitive-behavioral therapy | ||
| 810a | 20 | 10 |
| 1,600 | 45 | 23 |
| 2,000 | 68 | 30 |
Population Impact
Discussion and Conclusions
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 534.07 KB
References
Information & Authors
Information
Published In
Cover: Understanding, by Michael Olszewski, 1984. Dyed and pleated silk plain weave with silk embroidery. Philadelphia Museum of Art, gift of Nancy and David Bergman, 2015.
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).