Individuals with schizophrenia have high rates of psychiatric hospitalization (
1) and rehospitalization. In the United States, 25% of individuals with schizophrenia are rehospitalized three months after discharge (
2). The high readmission rate is likely attributable to discharge before adequate stabilization or to receipt of inadequate community-based services, neither of which reflect good care. Assertive community treatment (
3) and intensive case management (
4), two modes of intensive service delivery for individuals with severe mental illness, have been shown to be associated with reduced hospitalization but may not be available to, or necessary for, all patients with schizophrenia.
Although psychiatric readmission rates are high, and high quality and intensity of care appear to reduce hospitalization, only a few studies have specifically evaluated interventions to reduce readmissions. Also, these studies have focused on specific clinical populations (
5) or specific postdischarge clinical interventions (
6). The type of physician follow-up that reduces early psychiatric readmission is unknown. Access to psychiatrists is limited in many jurisdictions (
7–
9); individuals with schizophrenia often have access only to a primary care physician (PCP). Furthermore, individuals with schizophrenia have high rates of general medical comorbidity (
10,
11); access to both a PCP and psychiatrist may be necessary for optimal outcomes (
12). With an increasing emphasis on collaboration between psychiatrists and PCPs in the care of patients with complex conditions, such as those with schizophrenia (
13–
15), knowing what type of physician follow-up (for example, PCP, psychiatrist, or both) has the greatest impact is important.
The objective of this study was to evaluate the impact on readmission within the subsequent 180 days of follow-up care by a physician in the 30 days after discharge from a psychiatric inpatient unit. We hypothesized that seeing any physician after discharge would be associated with a reduction in the rate of psychiatric readmission and that patients who see a psychiatrist would have a lower risk of psychiatric readmission than patients who see a PCP only.
Methods
Data Sources
Ontario, Canada’s largest province, provides universal health coverage for all medically necessary health care. Patient-level records from multiple health administrative databases containing information on all publicly insured hospital and physician services were linked by using unique, encoded identifiers. These included the Ontario Mental Health Reporting System (OMHRS), which provides information from psychiatric hospitalizations; the Ontario Health Insurance Plan database, which provides information from physician visits; the National Ambulatory Care Reporting System for data on emergency department (ED) visits; and the Registered Persons Database for patient demographic information and deaths. Physician type (PCP or psychiatrist) was acquired from the Institute for Clinical Evaluative Sciences Physician Database. Neighborhood income level for each individual was based on his or her residential postal code and derived from Statistics Canada 2006 census estimates for income. This study was approved by the Sunnybrook Health Sciences Research Ethics Board.
Study Population
We included all adults ages 19 and older discharged with a most responsible diagnosis of schizophrenia (DSM-IV codes 295.x) between April 1, 2007, and March 31, 2012, after a nonforensic psychiatric hospitalization in Ontario that lasted three to 90 days. The most responsible diagnosis refers to the diagnosis that was the reason for the psychiatric hospitalization, as opposed to secondary diagnoses. We excluded individuals whose hospital length of stay was longer than 90 days because this relatively small number of patients with complex conditions may face specific challenges related to discharge. We also excluded individuals whose hospital length of stay was less than 72 hours because diagnostic information was missing. Similarly, we excluded a small number of individuals who were ineligible for health coverage in Ontario in the year prior to the incident admission (for example, recent immigrants). We also excluded those who died or were readmitted within 30 days of their discharge to allow a window of opportunity for patients to be seen by a PCP or a psychiatrist. For individuals with multiple hospitalizations over the study period, we included in our analysis the first hospitalization, with one exception: when a readmission occurred within 30 days of discharge from a hospitalization, that readmission was considered as the index admission, provided all other selection criteria were met.
Exposure Groups
Participants were classified into four groups on the basis of physician follow-up within 30 days postdischarge: no physician follow-up (reference group), follow-up by a PCP only, follow-up by a psychiatrist only, and follow-up by both a PCP and psychiatrist. Visits to other specialists were not considered.
Outcome
The primary outcome was readmission to a designated psychiatric bed in Ontario (that is, any readmission captured within the OMHRS database) between 31 and 210 days postdischarge to allow for a 30-day physician follow-up window after the discharge date and 180 days for outcome observation. The 180-day outcome period was chosen to be long enough to detect an effect but within a period when physician visits would be associated with readmission. Because a death would preclude a rehospitalization, we also assessed all-cause mortality between 31 and 210 days postdischarge. Physician follow-up in the outcome observation period (31–210 days) could influence readmission rates, and patients who did not receive follow-up within 30 days could have received follow-up shortly after the 30-day exposure period. Therefore, we measured PCP and psychiatrist visits in two periods during the outcome period—early (31 to 60 days) and late (31 to 210 days) to determine consistency of follow-up during the first 30 days throughout the outcome period. Consistent physician engagement (or lack of engagement) throughout both the exposure and outcome periods further establishes the association between physician follow-up and psychiatric readmission risk.
Covariates
Sociodemographic characteristics included age, sex, neighborhood income quintile, and residence (rural versus urban). We measured number of ED visits and psychiatric hospitalizations 12 months prior to admission. Health service utilization measures during the six months prior to the index hospitalization included visits to a psychiatrist or a PCP; PCP visits were categorized as mental health related or non–mental health related on the basis of a validated algorithm (
16). General medical comorbidities in the 12 months prior to the index hospitalization were identified by using the Johns Hopkins composite Aggregated Diagnostic Groups (cADGs), which provide 12 groupings of comorbidity categories based on prior health care utilization; these categories are good predictors of mortality in the general population (
17) and among persons with schizophrenia (
18).
Psychiatric symptom severity and psychosocial functioning at discharge were measured on the basis of information from the Resident Assessment Instrument for Mental Health (Inter-RAI-MH) (
19,
20), which was administered at the time of discharge and is part of the OMHRS data set. We included variables based on the following rating scales, which are included in the Inter-RAI-MH: Aggressive Behavior Scale, Activities of Daily Living Scale, Cognitive Performance Scale, Depression Rating Scale, Positive and Negative Syndrome Scale, CAGE Questionnaire, Suicide Behaviors Scale, and Global Assessment of Functioning (
21).
We used a validated readmission risk prediction tool (READMIT) (
22) to stratify the sample into three readmission risk categories (low, medium, and high). The READMIT was developed by using all psychiatric hospitalizations in Ontario between 2008 and 2011; it uses information available at the time of discharge to predict the probability of readmission. The READMIT generates scores between 0 and 41; a score <15 indicates a low risk of readmission, 15–18 indicates a medium risk, and >18 indicates a high risk.
Statistical Analysis
In the primary analysis, time to psychiatric readmission or death between 31 and 210 days after discharge from the index hospitalization was analyzed by using a Cox proportional hazards (PH) model. Patients with no physician follow-up visit formed the reference group. We adjusted for the following patient characteristics: demographic (age, sex, age-sex interactions, neighborhood income, and rural versus urban residence), clinical (cADGs in the 12 months preceding admission and psychiatric symptom severity and psychosocial functioning at discharge as measured by the Inter-RAI Mental Health [
19]), and health service utilization variables (total number of prior psychiatric hospitalizations and total number of prior ED visits). For the main outcome analyses (psychiatric readmissions) and the main sensitivity analyses (psychiatric readmission or death), the regression models included demographic variables, clinical variables, and health service utilization variables. Patient data were censored if the patient died during the follow-up period; we conducted a sensitivity analysis that combined death with psychiatric readmission as an outcome.
In secondary analyses, we stratified the cohort into psychiatric readmission risk tertiles. We also tested whether the timing of a physician visit (PCP or psychiatrist) postdischarge influenced readmission risk by categorizing patients into different postdischarge physician visit time periods (first visit within one to seven days, eight to 14 days, or 15 to 30 days postdischarge), with no physician visit as the reference group. Violation of the Cox PH proportionality assumption was tested by using time-dependent covariates in all analyses. We used SAS version 9.3 (
23) for all statistical analyses.
Results
Cohort Description
Between April 1, 2007, and March 31, 2012, a total of 22,640 unique patients had 47,280 hospitalizations associated with a most responsible discharge diagnosis of schizophrenia. [A figure presenting details on cohort creation is included in an online supplement to this article.] Exclusion criteria were applied to both hospitalizations and patients; 2,667 hospitalizations were excluded because of a missing discharge assessment or other missing data, 4,788 because the hospital length of stay was less than three or more than 90 days, and 6,105 because the patient was readmitted within 30 days postdischarge (the readmission was potentially eligible for cohort inclusion). Patients were excluded if they were younger than 19 or older than 105 (N=614), ineligible for health insurance in the year prior to admission (N=686), or died within 30 days postdischarge (N=68). In total, there were 3,508 patients (15%) excluded for reasons cited above. The excluded patients differed from the final cohort in readmission risk at discharge and in age [see table in online supplement]. The final cohort in readmission risk at discharge and in age [see table in online supplement]. Considering only the first eligible hospitalization during the study period, the final cohort comprised 19,132 unique patients with a discharge diagnosis of schizophrenia (85% of all hospitalized schizophrenia patients), of whom 6,649 (35%) did not have any follow-up visits with a PCP or a psychiatrist within 30 days of discharge; 4,026 (21%) saw a PCP only; 5,374 (28%) saw a psychiatrist only; and 3,083 (16%) saw both a PCP and psychiatrist.
Baseline Characteristics
Psychiatric symptoms or psychosocial functioning at discharge, proportion with ED visits (all cause), psychiatric hospitalizations within 12 months preceding the index admission, and mean psychiatric readmission risk at discharge were similar across the four follow-up groups (
Table 1). However, there were notable differences in sociodemographic variables and in some health service use: patients followed up by a PCP (with or without a psychiatrist) were more likely to be women and older, compared with those not followed up or followed up by a psychiatrist only. Patients followed up by a psychiatrist (with or without a PCP) were more likely to reside in urban areas, compared with those not followed up or followed up by a PCP only. The type of physicians that patients saw prior to the index admission was strongly indicative of the type of physician they saw postdischarge.
Outcomes
The psychiatric readmission rate in the entire cohort was 23% (N=4,421 of 19,132 patients). Patients with no physician visit within 30 days postdischarge had the highest rate of psychiatric readmission (26%) within 31–210 days (
Table 2). Rates of psychiatric readmission were modestly but significantly lower among those who were followed up by any of the three physician follow-up categories, compared with those with no physician visit. Results were unchanged when death was combined with psychiatric readmission in the outcome (
Table 2). For both outcomes, the adjusted hazard ratios (aHRs) for physician follow-up did not vary with sequential inclusion of demographic, clinical, and health service utilization covariates.
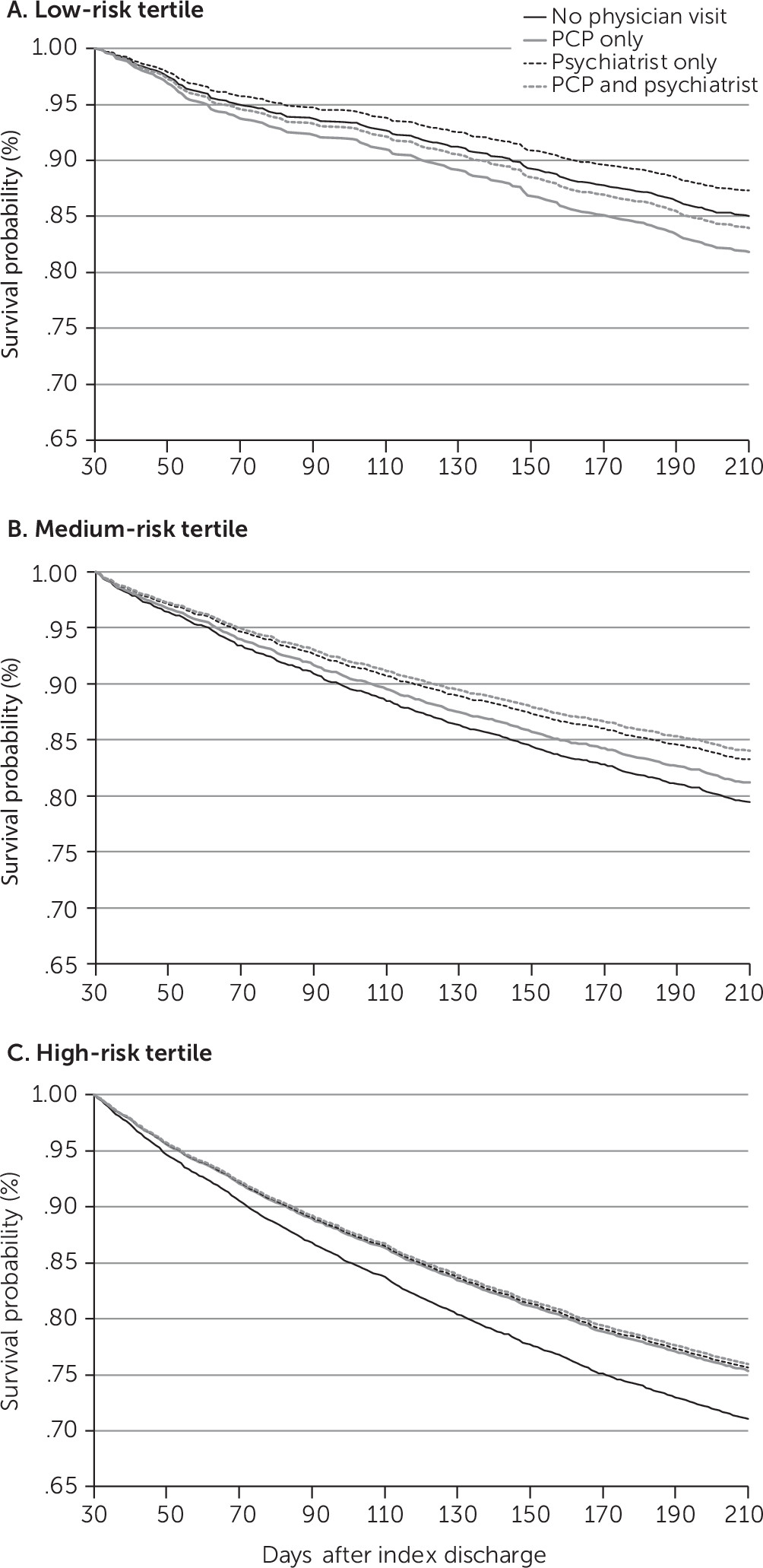
In stratified analyses, 66% of patients were in the highest psychiatric readmission risk tertile, 26% were in the medium tertile, and 8% were in the low tertile [see
online supplement]. Psychiatric readmission rates for the low, middle, and high tertiles were 15%, 18%, and 26%, respectively. For patients in the low tertile, postdischarge follow-up was not associated with a significant reduction in psychiatric readmission rates (
Figure 1, panel A). For patients in the medium tertile, only those seen by a psychiatrist had a significant reduction in psychiatric readmission rates (aHR=.82, 95% confidence interval [CI]=.69–.97) (
Figure 1, panel B). However, for patients in the high-risk tertile, each of the follow-up groups was associated with a significantly lower risk of psychiatric readmission, compared with the no-visit patients in the high-risk tertile group, whose readmission rate was 29%. Follow-up by a PCP or a psychiatrist was associated with a reduction in readmission rates of about 15%, compared with the no-follow-up group (PCP only, aHR=.85, CI=.77–.94; psychiatrist only, aHR=.84, CI=.77–.92). Seeing both a psychiatrist and a PCP was associated with a 19% reduction in psychiatric readmission rates, compared with the no-follow-up group (aHR=.81, CI=.73–.90) (
Figure 1, panel C).
Psychiatric readmission rates were reduced by a similar magnitude, compared with the no-visit group, when the first follow-up visit with any physician was categorized on the basis of timing, as shown in the model that included all covariates (
Table 2): a visit to any physician within one to seven days postdischarge, aHR =.86; within eight to 14 days, aHR=.82; within 15 to 30 days, aHR=.85.
The proportions of patients in each physician follow-up category who saw either a PCP or a psychiatrist between 31 and 60 days and between 31 and 210 days are shown in
Table 3. The patterns observed in the first 30 days postdischarge were similar to the patterns seen between 31 and 210 days,
Discussion
For patients with schizophrenia, seeing a PCP or a psychiatrist within 30 days after a psychiatric hospitalization was associated with a significant but modest reduction in the likelihood of a psychiatric readmission within 31 to 210 days. This result was driven primarily by the two-thirds of patients at high risk of psychiatric readmission at discharge. Compared with patients in the high-risk group who had no follow-up visit with a physician, patients who were followed up by a PCP or psychiatrist were between 15% and 19% less likely to be readmitted. In the overall sample, more than one-third of patients did not see a physician within 30 days of discharge, even though half had seen a PCP and two in five had seen a psychiatrist in the six months preceding the index admission. To our knowledge, this is one of the first studies to evaluate the association between one mental health performance indicator—postdischarge follow-up by a physician—and another universally measured performance indicator—psychiatric readmission.
Few studies have evaluated the impact of physician follow-up on postdischarge transition to the community (
5). In a large U.S. Medicaid study of postdischarge access to care among individuals with schizophrenia, 41% of patients received no outpatient care in the 30 days postdischarge (
24), slightly higher than the rate in our study. However, the Medicaid study did not evaluate the impact of postdischarge access to care on readmission rates. One study assessed the impact of postdischarge access to care, but it focused on patients with comorbid substance use and psychiatric disorders and found that postdischarge addiction care, and not psychiatric care, reduced readmissions (
25). A recent study evaluated postdischarge follow-up by a mental health professional or by a primary care provider among patients discharged with a diagnosis of depression or schizophrenia and included psychiatric readmission as an outcome (
6). Postdischarge follow-up did not reduce readmission rates in that study, but the study had limited generalizability because it included only Medicaid recipients and employed a complex intervention to integrate and coordinate care for individuals with complex chronic conditions. Thus, to our knowledge, our study is one of the first to systematically evaluate the impact of postdischarge physician follow-up among patients with schizophrenia.
Although seeing any physician was associated with a modest reduction in the readmission rate for the entire cohort, the most striking finding was the impact for patients at high risk of readmission. By 210 days, more than one in four of those at highest risk experienced a psychiatric readmission, and physician follow-up reduced the risk of readmission by up to 19%. The fact that patients at high risk of readmission benefited from postdischarge physician follow-up is consistent with evidence that interventions to help with the transition from the hospital to community-based settings are most effective among patients with high readmission risk (
5). By contrast, postdischarge physician follow-up had no impact on readmission rates in the lowest risk category. However, postdischarge follow-up is associated with a number of processes of care, such as adherence to the pharmacological treatment, that helped stabilize the individual during hospitalization and engagement with other services that support postdischarge stabilization. The patients at low and medium risk of readmission may have benefited from physician follow-up in ways not captured by our primary outcome of readmission.
Our study had some strengths and limitations. It was a population-based study that captured all hospitalizations and postdischarge readmissions associated with a diagnosis of schizophrenia in Ontario during the study period. We had access to a wide array of sociodemographic and clinical variables that allowed us to more comprehensively control for clinical severity than is typical for studies using administrative databases. However, we cannot exclude the possibility of unmeasured confounding; for example, family support, which we were unable to measure, may be associated with both a higher likelihood of physician follow-up and a reduced likelihood of readmission. Also, we did not have information about nonphysician postdischarge care in the community, which could have affected readmission rates. However, follow-up care only by nonphysicians is uncommon in Ontario, whereas there is anecdotal evidence that follow-up care with physicians only is common, particularly in rural areas with fewer community-based resources than urban centers. Finally, this was an observational study and thus we cannot assume that postdischarge follow-up was a causal factor affecting readmission; individuals who received postdischarge follow-up may also have been less likely to be readmitted, and there are factors that may affect readmission (such as access to non–physician-based services postdischarge) that we were not able to measure and that may have confounded the findings. However, if such selection bias existed, it was not observed equally across all readmission risk categories, and it seems unlikely that it would be a factor only among individuals with high readmission risk. Finally, we did not measure the quantity and timing of outpatient visits; these factors should be a focus of future research.
Conclusions
A substantial proportion of patients with schizophrenia did not see any physician within 30 days of discharge, and they experienced a high rate of readmission postdischarge. Seeing a physician was associated with a modest reduction in readmission risk. Results indicate that physician follow-up is mostly likely to have an impact on the majority of patients at high risk of readmission. Postdischarge physician follow-up is a quality indicator, and our study provides evidence that physician follow-up has the greatest impact among patients at high risk of readmission and, therefore, with the greatest need for follow-up. Other factors that contribute to the high readmission rate of patients with schizophrenia need to be better understood in order to design interventions that improve their postdischarge outcomes.