On January 1, 2013, the American Medical Association implemented significant revisions to the Current Procedural Terminology (CPT) code set for psychiatry and psychotherapy services (
1). These changes eliminated more than 30 of the most commonly used psychiatry CPT codes and introduced several new codes (
2). CPT codes are the main framework under which services provided by physicians and other health care professionals are documented and reimbursed. These codes also are used for prior authorization determination, quality measurement, pay-for-performance assessment, and other essential U.S. health care system activities (
3). CPT code changes have the potential to influence medical practice (
4).
The 2013 CPT revisions were designed to improve the ability of the codes to account for varying levels of psychotherapy and medical management, to represent the greater intensity and complexity of psychiatric services related to the increased number of patients with comorbid conditions and complications, and to reflect the shift from inpatient to outpatient settings, with higher intensity of work in outpatient settings (
1).
In addition to ensuring that the codes reflect the current practice of psychiatry, the updates were designed to align psychiatric billing and documentation with the model for billing and documentation used by other specialties (
5). Before the changes were implemented, the time that psychiatrists spent prescribing psychiatric medications or monitoring patients for medications’ treatment efficacy and side effects had been billed under a psychiatric-specific CPT code called pharmacologic management (90862). Prior to 2013, this CPT code was one of the codes most commonly used by psychiatrists (
6). Under the new coding schema, this code was eliminated; psychiatrists now bill for time spent addressing psychiatric medication using generic evaluation and management (E/M) codes for pharmacologic management. These are the same codes used by all other medical specialties.
The Centers for Medicare and Medicaid Services establishes the guidelines for determining how E/M codes can be used (
7). There are currently 10 different outpatient E/M codes that vary depending on whether the patient is new or established, the type of setting (outpatient, inpatient, or nursing facility), and the complexity of the service provided (for example, case history, examination, and medical decision making) as determined by the nature of the presenting problem.
The new CPT coding also changed the way that psychiatrists bill for visits that involve both medication management and psychotherapy. Prior to 2013, psychiatrists billed for visits that included both psychotherapy and medical evaluation services by using CPT codes specific to psychiatry that combined these services. For example, outpatient individual psychotherapy with medication management provided for 20–30 minutes would be billed using CPT code 90805. In contrast, starting in 2013, psychiatrists billed for this type of visit using an E/M code in conjunction with a psychotherapy add-on code. An add-on code describes work performed in addition to the primary service and is never used alone. Therefore, in 2013, this same visit would be coded using CPT E/M code 99213 (for example, indicating an established patient who has a presenting problem of low to moderate severity) and the CPT add-on 90833 code (indicating 16–37 minutes of psychotherapy).
The purpose of this study was to examine whether the change in the CPT coding schema altered the types of services for which psychiatrists billed insurance companies. In particular, we examined whether the coding changes affected the probability that a visit to a psychiatrist included billing for psychotherapy.
Methods
We used 2012–2014 data from the Truven Health Analytics MarketScan Commercial Claims and Encounters (MarketScan) database. The MarketScan database reflects the entire claims experience of approximately 30 million individuals with private insurance annually, representing approximately 15% of all individuals with private health insurance in the United States. The data reflect a variety of health insurance carriers and include all states in the United States. They include all insured services received by enrollees, including any services covered by a behavioral health managed care specialty plan (a “carve-out”). The data are deidentified.
The sample in this study was restricted to office visits to psychiatrists in 2012 (prior to the CPT code changes) and in 2013 and 2014 (the two years after the CPT code changes). To ensure that trends observed were not influenced by changes in the mix of psychiatrists, the sample was restricted to psychiatrists with paid claims in each of the calendar years studied. The analytic sample of visits to psychiatrists comprised 227,191, 222,391, and 222,980 patients, who collectively had 778,445, 748,317, and 754,760 visits in 2012, 2013, and 2014, respectively. The sample of visits was generally consistent across years in terms of patient characteristics. [Further details about the characteristics of the sample are available in an
online supplement to this article.] The most prevalent diagnoses grouped according to the Agency for Healthcare Research and Quality’s Clinical Classification Software were mood disorders (53%), anxiety disorders (18%), and attention-deficit, conduct, and disruptive behavior disorders (14%) (
8).
To understand how the CPT code changes may have influenced the billing of psychotherapy, we classified visits into four mutually exclusive categories: visits with any documented psychotherapy, visits with evaluation and management or psychotropic prescribing but not documented psychotherapy, visits with diagnostic evaluation but not documented psychotherapy, and all other types of services (for example, qualitative drug screen testing).
To control for other changes that may have occurred over this time period and may have influenced the billing of psychotherapy, we estimated a multivariable linear probability model to predict receipt of any psychotherapy during a visit to a psychiatrist. Our independent variables of interest were dichotomous variables indicating whether the service took place in one of the years after the CPT coding changes occurred (that is, either in 2013 or 2014). Independent variables were gender, diagnosis, age, region, and size of the physician’s practice. We included insurance plan fixed effects to control for differences among insurance plans. Analysis was conducted using SAS 9.4.
Results
The most common CPT code used in 2012 was 90862 (pharmacological management), followed by 90805 (individual psychotherapy codes with E/M, 20–30 minutes), and 90807 (individual psychotherapy with E/M, 45–50 minutes). In 2013, the most common CPT code was the E/M code 99213 (established patient office visit, low to moderate severity), followed by the E/M code 99214 (established patient office visit, moderate severity), and the 90833 add-on code (individual psychotherapy, 16–37 minutes). [The specific 10 most common CPT codes used for psychiatrist office visits are available in the online supplement.]
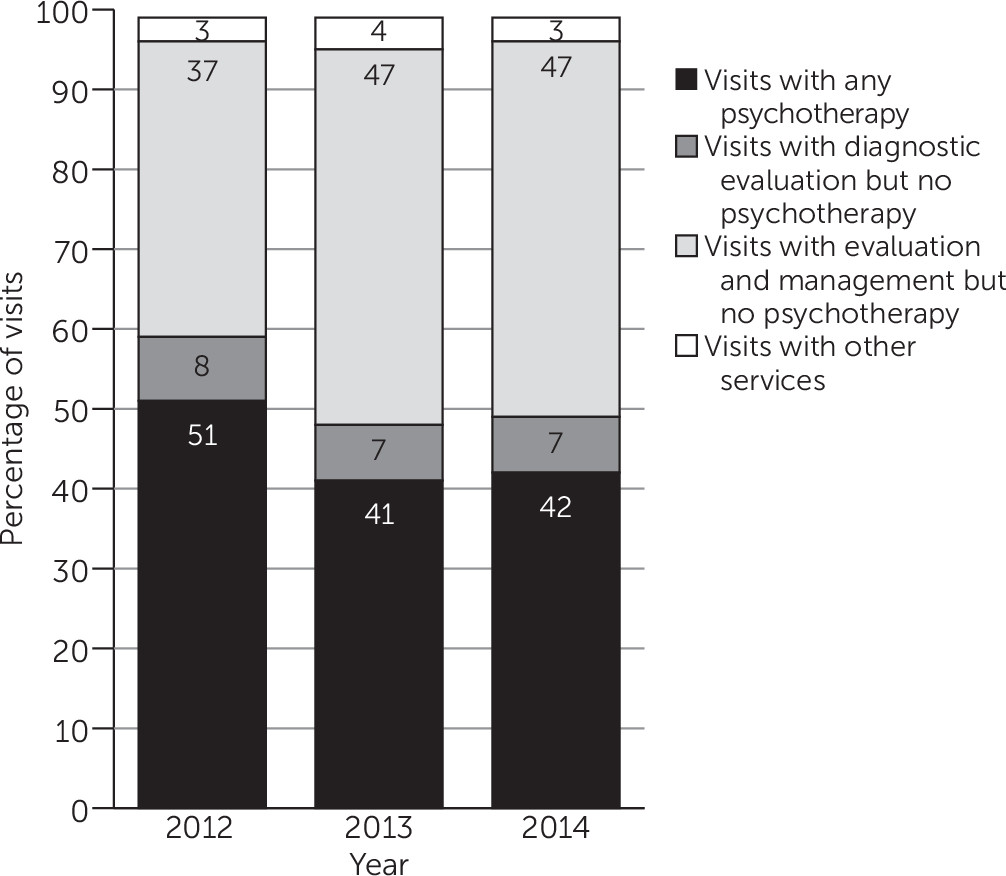
Figure 1 presents the type of services billed by psychiatrists from 2012–2014. Across these three years, the percentage of visits that included any psychotherapy billing code declined from 51% in 2012 to 41% in 2013 and 42% in 2014. In contrast, the percentage of visits that included E/M but no psychotherapy billing code increased from 37% in 2012 to 47% in 2013 and 2014. This decline among visits to psychiatrists corresponds to a decline in the proportion of patients who were billed as receiving any psychotherapy from a psychiatrist during the three-year period of this study, from 50% in 2012 to 40% in 2013 and 39% in 2014.
After controlling for factors related to the patient, practice, and health plan in a linear probability model with plan-level fixed effects, we found a mean±SE decrease of 9.82±.17 percentage points (p<.001) and 9.34±.18 percentage points (p<.001) from 2012 to 2013 and 2014, respectively, in the probability of a visit to a psychiatrist billed with any psychotherapy service. [Further details about the probability model are available in an online supplement to this article.]
Discussion
This study examined whether the changes implemented in the 2013 CPT code revision to psychiatric coding had an impact on the billing of psychotherapy during visits to psychiatrists paid for by private insurance. We found that after the CPT coding changes were implemented, the proportion of psychiatric visits in which the claim included a psychotherapy billing code significantly decreased in the first year of use and remained at that level in the following year. It cannot be determined with certainty from insurance claims data whether this decline reflects an actual decrease in the provision of psychotherapy or a change in coding practices. It may be that prior to the CPT coding changes, some psychiatrists who coded for a psychotherapy visit were not providing psychotherapy but rather were having discussions with patients consistent with an E/M visit (for example, recommended tests or test results; impressions; prognosis; risks and benefits of treatment options; instructions for management, treatment, or follow-up care; treatment compliance; risk factor reduction; and other forms of education).
After the coding changes, it was clarified that discussions of this nature should be billed as E/M and not as psychotherapy. To bill for psychotherapy, the use of add-on codes made it clear that psychiatrists had to spend at least 16 minutes providing psychotherapy, in addition to the time spent delivering E/M services. Although it is also possible that some of the decline resulted from the adjustment to using a new system that required additional time and supplemental codes for documentation (
9,
10), the new documentation requirements likely would not explain the percentage difference that remained in the second year of use.
The change in billing procedures may represent a more accurate reflection of the way in which services are delivered. In some settings, psychiatrists focus primarily on medication management and very short counseling, with other professionals, such as psychologists and social workers, providing longer psychotherapy (
11). Further study of the economic and clinical effects of the provision of services by different mental health service provider types, particularly in integrated, multispecialty, or coordinated practices, may be warranted.
Our study had several limitations. First, we were only able to assess provider billing behavior and not clinical practice. Future work should consider whether the changes documented here reflect changes in services provided during patient visits. A second limitation is that our results are limited to visits by patients with private insurance. Third, our study did not present a global view of the provider. The data in our database are from approximately 15% of individuals who have private insurance but do not necessarily include all the patients treated by the provider who were not covered by the insurers captured in the MarketScan database.
The change in CPT psychiatric billing codes resulted in a significant decline in documented psychotherapy by psychiatrists among privately insured patients. Whether this was due to a change in actual treatments provided or a clarification of the extent to which psychotherapy was actually being provided (must be at least 16 minutes in length) is an issue that requires further investigation. Future work should also investigate the rates of psychotherapy provided by other providers for the same patients. Given that the majority of visits to psychiatrists included E/M services only, efforts and incentives could be used to increase care coordination, treatment in teams, and colocation of mental health services to support the provision of mental health care.
Acknowledgments
The authors thank Nils Nordstrand, who provided excellent programming support, Christine Walsh, who provided excellent assistance creating the programming specifications and reviewing output for accuracy, and Susan Busch, Ph.D., who provided assistance in conducting this study.