Mental health courts and outpatient civil commitment (also known as assisted outpatient treatment [AOT]) are legal mechanisms to help people with serious mental disorders engage in treatment, prevent relapse, and increase time spent living in the community. Mental health courts serve justice-involved individuals with severe mental illness, and AOT primarily serves those who have repeated psychiatric hospitalizations. Both programs mandate treatment, either through the criminal justice system (mental health courts) or through the civil commitment system (AOT). Both programs provide access to treatment while minimizing institutional confinement. Mental health courts seek to reduce future incarcerations, whereas AOT seeks to increase community tenure and shorten the length of any needed hospitalizations.
Typically candidates for AOT do not engage voluntarily with community-based treatment, and they move in and out of institutional settings (
1–
3). Use of AOT tends to follow a general pattern—an individual becomes psychotic, meets civil commitment criteria, is involuntarily hospitalized, and is treated and stabilized. Upon discharge from the hospital, the individual discontinues treatment, decompensates, and may be rehospitalized. AOT interrupts this cycle, using the authority of the court to mandate monitoring and treatment to increase tenure in the community. Depending on the jurisdiction, forced medication is not typically part of an AOT court order. Nonadherence to the treatment plan can result in being picked up by the police for rehospitalization (
1,
3,
4). Despite the program’s weak enforcement powers, participation in AOT is involuntary.
Mental health courts seek to prevent future justice involvement by connecting offenders with mental illness to community-based treatment (
5–
11). Mental health courts were founded on the principles of the criminalization hypothesis, suggesting that people with mental illness become justice-involved because of behavior that is labeled as criminal but that stems from symptomatic, untreated mental illness (
12–
14). Mental health courts use the principles of therapeutic jurisprudence to engage participants in community-based mental health services with the goal of improving clinical and criminal justice outcomes. Although participants volunteer for the program, which mandates treatment, it has strong enforcement powers for participants who do not adhere to the treatment plan.
The notion that mental illness can be criminalized suggests that the people being arrested could just as likely be the people who are hospitalized for mental illness (
3,
13–
17). Because of a reduction in available mental health services, including hospital beds, and a lack of training or other options among first responders, a person with symptomatic mental illness may end up in jail instead of in a crisis center or a hospital. Where such individuals end up might depend on circumstances other than the nature of the person’s behavior. If the individual is incarcerated, he or she might be a candidate for mental health court. If, however, the individual is hospitalized, he or she might be a candidate for AOT. Some individuals may be admitted to either program at different times or to both programs at the same time. However, the extent to which there is overlap among users of these programs is unknown.
Recently some researchers have challenged the criminalization hypothesis, finding that symptoms of mental illness are not the precipitant of most incarcerations of individuals with serious mental illness (
18–
20). This suggests that a substantial proportion of people with severe mental illness who end up in the justice system have different characteristics than those who end up in the civil commitment system. These differences include demographic and diagnostic characteristics as well as different jail and hospitalization histories and service use histories.
AOT and mental health courts are complex community interventions with different selection criteria and processes. Summit County (Akron), Ohio, has utilized AOT under the Ohio civil commitment statute since 1994. Following guidelines developed by Geller (
21), patients are eligible for AOT if they have a history of hospitalizations, respond to treatment when hospitalized, and have a pattern of discontinuing treatment after discharge.
The Akron Municipal Court operates a mental health court, serving misdemeanants with a mental illness, primarily schizophrenia, schizoaffective disorder, or bipolar disorder. Individuals must be competent to agree voluntarily to the program and its requirements, which provides two years of closely supervised, community-based treatment.
Although there is mounting evidence in support of the effectiveness of both programs in reducing justice involvement and encouraging treatment engagement (
2,
22–
26), questions remain about the individuals for whom the services may be most appropriate and effective. Selection requirements shape who ends up in AOT or mental health court, yet there is scant research examining the characteristics of clients engaged in these programs. If there are clear differences in those served by these programs, the programs are likely to require the use of different assessments and interventions tailored to the specific needs of participants.
The purpose of this study was to examine whether demographic or diagnostic characteristics, prior service utilization, prior incarcerations, and prior hospitalizations differentiate people who are in AOT from those in mental health court. Our research questions were, To what extent did those who participated in mental health court also participate in AOT during the study period? Are there demographic and diagnostic differences among individuals in these programs? and Do prior services, psychiatric hospitalizations, or incarcerations differentiate AOT and mental health court participants?
Methods
The sample consisted of people who were committed to the Summit County Alcohol, Drug Addiction and Mental Health Services (ADM) Board for at least six months during 2001–2007 (AOT sample) or participated in mental health court in the same community during the same seven-year period. Participants in either program received care from a single mental health provider agency. Data were from administrative databases provided by the Summit County ADM Board, the provider agency, the Akron Municipal Court, the Summit County Sheriff, and the Ohio Multi-Agency Community Services Information System. Only participants with complete data for history of incarcerations, hospitalizations, and mental health services at least six months before program participation were included. Data were also collected on gender, race, age, substance use disorder, and principal psychiatric diagnosis.
Services examined were alcohol and drug assessment, alcohol and drug case management, alcohol and drug counseling, alcohol and drug pharmacological management, alcohol and drug residential treatment, mental health assessment, mental health case management, mental health counseling, mental health crisis care (includes residential crisis care and crisis intervention and stabilization), mental health day treatment, mental health pharmacological management (i.e., primarily outpatient psychiatric services), mental health residential treatment, and mental health vocational training. For comparison, we converted available data to one year (annualized) for days of incarceration and hospitalization and units of mental health services based on the amount of time prior to entering a program.
We used t tests and multivariate logistic regression to assess potential differences in sociodemographic characteristics, psychiatric diagnoses, mental health service utilization, hospitalizations, and incarcerations for participants in both programs. Data were analyzed by using SPSS, version 24. The institutional review boards at Kent State University and Northeast Ohio Medical University approved the study.
Results
The sample consisted of 261 people with at least six months of service data prior to any program participation (range 184 days to over six years; mean±SD=2.1±1.1 years). We first determined whether the same individuals participated in AOT and mental health court over a seven-year period. We found that only eight people (3%) participated in both AOT and mental health court during the seven-year study period. This suggests that there is little overlap among participants of the programs. We do not know how many individuals with AOT histories may have refused a previous offer to participate in mental health court.
Because there were too few people who participated in both programs to enable studying individual characteristics, we removed these eight individuals from further analyses, leaving a total of 253 participants, 70 in AOT and 183 in mental health court. Next, we examined characteristics that differentiated clients in these programs. We found that the AOT group was older, had a lower percentage of persons from a racial minority group (primarily African Americans), and had fewer members with alcohol- and drug-related disorders. The majority of AOT participants (83%) had schizophrenia-spectrum diagnoses, compared with 42% of mental health court participants (
Table 1). In addition, the annualized average number of hospital days prior to entry to the program was significantly higher in the AOT (41.4+52.2) than in the mental health court group (2.2+5.9). The number of days hospitalized before entering the program and the number of days incarcerated before entering the program were not significantly correlated (data not shown).
All AOT participants received at least one type of service other than hospitalization in the period prior to program participation, compared with 85% of mental health court participants. The use of four services (mental health residential crisis care, mental health crisis intervention [includes assessment, stabilization, and determining level of care], mental health case management, and mental health residential treatment) were significantly different between program participants, according to bivariate analyses (
Table 1). The AOT group received more of these four mental health services prior to program entry than did participants in mental health court. Services for which there were no significant differences between the AOT and mental health court group are not presented in the table.
Using logistic regression, we found that participants in mental health court were younger, more likely to have an alcohol use disorder, and more likely to have a diagnosis of bipolar disorder. Days hospitalized prior to any program participation significantly decreased the likelihood of being in mental health court versus AOT. Jail days prior to any program participation significantly increased the likelihood of being in mental health court versus AOT. In addition, receipt of mental health residential crisis care decreased the likelihood of being in mental health court versus AOT (
Table 2).
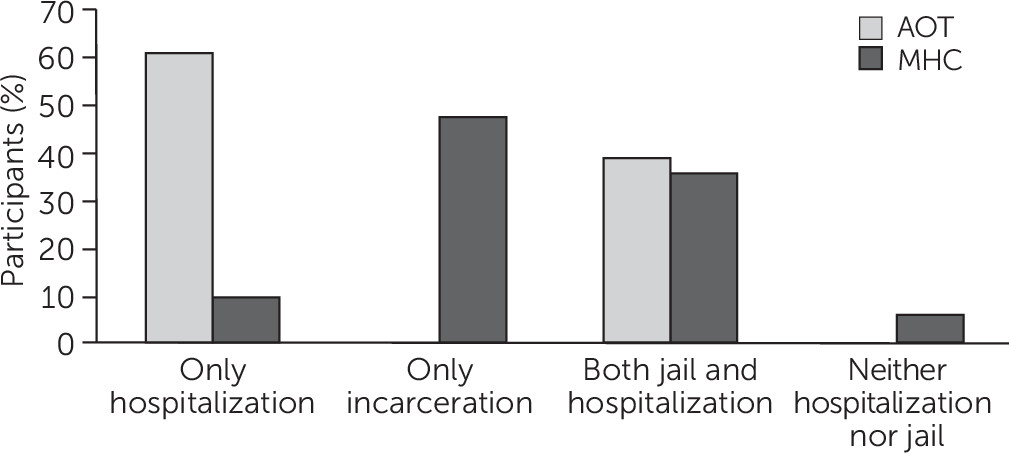
We then looked at the occurrence of hospitalizations and incarcerations prior to entering either program. For AOT participants, 61% (N=43) had only hospitalizations and 39% (N=27) had both hospitalizations and incarcerations before entering AOT. For mental health court participants, 48% (N=88) had incarcerations (jail) only, 36% (N=66) had both hospitalizations and incarcerations, 10% (N=18) had only hospitalizations, and 6% (N=11) had neither prior hospitalizations nor incarcerations (jail) (
Figure 1). These findings suggest that there were fundamental differences in prior hospitalization and incarceration among people enrolled in AOT or mental health court.
Discussion
In a single county that has mental health court and AOT programs, both of which are longstanding, very few individuals (3%) participated in both programs during a seven-year period, suggesting that there was essentially no overlap among participants of these programs. Both programs appear to be serving individuals with different psychiatric diagnoses, sociodemographic characteristics, service histories, and incarceration histories. This finding also suggests that potential participants in these two distinct mandated treatment programs had different needs that should be addressed to maximize desired outcomes.
Specifically, AOT participants were more likely than the mental health court sample to have schizophrenia (compared with bipolar disorder) and to have been hospitalized and have used crisis mental health services in the period before enrollment. We also found that a subset of the AOT sample (39%) had prior criminal justice involvement, even though those individuals rarely participated in the mental health court program during the study period.
The selection criteria of these programs were designed to target people with prior hospitalization (AOT) or recent justice involvement (mental health court), but there were no selection factors that precluded co- enrollment or participation in both programs. Given that 39% of individuals in the AOT group had a previous incarceration, one might have expected that some of these individuals would have been referred to mental health court. That such referrals were apparently rare suggests that mental health and court personnel who screen for appropriate mental health court candidates found reasons not to refer those individuals, who ended up in AOT. It is also possible that these individuals declined to participate in mental health court. Agreeing to participate in mental health court requires a willingness to engage in extended treatment rather than face what could be a short jail sentence. It is possible that individuals with more antisocial attitudes and beliefs (criminogenic needs) are more likely to refuse mental health court. Without referral, screening, or assessment data, however, we cannot tell if these factors explain why AOT participants with a prior incarceration did not participate in mental health court. Research is needed to explore how the voluntary or involuntary nature of these programs shapes the types of clientele served.
Compared with people in mental health court, AOT participants were older, used more crisis services, including psychiatric hospitalizations, and were more likely to have a diagnosis of schizophrenia instead of bipolar disorder. These characteristics suggest that individuals who used AOT had different clinical needs and appeared to use more crisis services compared with those in mental health court.
The findings of this study underscore that multiple factors and prior behaviors contribute to participation in programs for persons with serious mental illness. They also highlight the need for mental health systems to better understand the differences among participants in various programs. Program administrators will increasingly be called upon to recognize the multiple factors that contribute to institutionalization of people with mental illness and to consider these needs in the context of available community-based programming. A central task of future research in this area is to identify what those needs are and to tailor an appropriate treatment, supervision, and service approach.
Practice is already shifting toward identifying how community-based programs, such as mental health courts and AOT, can identify and address clients’ risks and needs across multiple domains, including mental health and substance use treatment needs, criminogenic risk, and violence risk (
22,
27–
29). A recent recommendation calls for using the risk-need-responsivity framework to address criminogenic risk and criminal thinking among persons with serious mental illnesses (
30). Clearly this recommendation applies to those at high risk of incarceration. For these individuals, specialized probation, mental health courts, and forensic assertive community treatment (FACT) programs may be good options (
29,
31,
32). AOT appears to help individuals at high risk of hospitalization and may have a secondary impact on reducing incarcerations among those at risk for both (
1,
2,
33,
34).
Given the high prevalence of service engagement for people who enter both programs, there is an opportunity for mental health service providers to identify clients’ areas of need along with other clinical assessments (i.e., suicide, violence risk, and clinical needs). Such assessment may help in determining program placement or the need for community-based services. Given the prevalence of prior justice involvement among participants in both mental health court and AOT, it is imperative that program administrators are aware of and address criminogenic risk factors, once clinical stability is achieved, to prevent future incarceration.
For high jail utilizers with few prior hospitalizations, mental health courts appear to be an appropriate intervention to reduce recidivism and divert the individual into the mental health treatment system. It is important that such programs address not only participants’ mental health and addiction treatment needs but also factors that may increase the risk of failure in the program (
35). These factors include dynamic criminogenic needs—including antisocial behaviors, personality patterns, antisocial peers, and criminal thinking—as well as social factors—such as housing and transportation. FACT teams may be an option for those who are eligible for mental health court but refuse to participate (
31). For those with repeated hospitalizations without frequent incarcerations, AOT may be an effective intervention.
Although the sample was relatively large and included seven years of data, this was an uncontrolled naturalistic experiment that used a convenience sample, which may represent what happens in a real-world setting but limits generalizability. A limitation of this study involved the use of different selection criteria for each program and how these criteria potentially shaped the pool of eligible participants (
36). Selection into mental health court requires criminal adjudication, whereas there is no such criterion for AOT.
Furthermore, the mental health court serves residents of the city of Akron, whereas the AOT program serves all residents of the county, offering a broader and potentially more middle-class demographic. Although we were unable to account for where participants lived or for individual-level socioeconomic status, all participants from both programs were clients of a single provider agency, where most clients receive disability benefits (93%), live in an urban setting (65%), and have an annual income below the federal poverty level (76%) (
37,
38). However, future research should examine the effects of socioeconomic status and where participants live, perhaps by geocoding by zip code, to determine if such factors shape program participation.
Another limitation was that we could not compare the characteristics of AOT and mental health court clients in this study with those of clients of the community mental health system who were not engaged in these programs, despite being appropriate candidates for participation. The mental health court in the study is a misdemeanor court, so individuals charged with felonies were not included in the sample. Although we had incarceration data, we were not able to access arrest data or information on the specific nature of the crimes (e.g., type of offense). Finally, beyond history of incarcerations, we did not have criminogenic risk assessment data for individuals in this study.
Conclusions
The results of this study suggest that there were differences among individuals with severe mental illness who participated in mental health court or AOT. Our data suggest that the programs serve clients with different demographic characteristics and clinical and criminal histories, with mental health court serving those at risk of incarceration and AOT serving those at risk of repeated hospitalization. The AOT program also serves individuals who were at risk of both incarceration and hospitalization.
Both AOT and mental health court use legal authority to mandate community-based treatment. However, at present, it is unknown whether or how these programs meet the criminogenic needs of clients served. There are recent calls for program administrators to assess and identify clinical and criminogenic needs of clients (
26,
39). To be most effective, interventions seeking to maintain community tenure among high utilizers of institutional service should recognize the multiple needs of clients and respond appropriately.