The projected shortage of physicians in the United States is garnering attention in academic circles, the media, and among health care providers. As of April 2016, the total physician shortfall is projected to be between 61,700 and 94,700 by 2025 (
1). Although much attention is focused on primary care and surgical (
2,
3) specialties, recent data provide evidence for a significant shortage in the specialty of psychiatry. A recent, in-depth analysis of the projected shortage has not been conducted. Previous estimates of the current shortage of psychiatrists vary considerably, ranging from 2,800 (
4) to 45,000 (
5). To address the shortage in light of the growing U.S. population and the fact that mental illness has become the most costly condition in the United States, at $201 billion annually (
6), the estimated shortage must first be quantified. In this review, our objective was to examine the current workforce of psychiatrists, provide an estimate of the projected workforce given the wide range of published estimates, and begin a discussion for addressing the workforce needs of the future.
Discussion
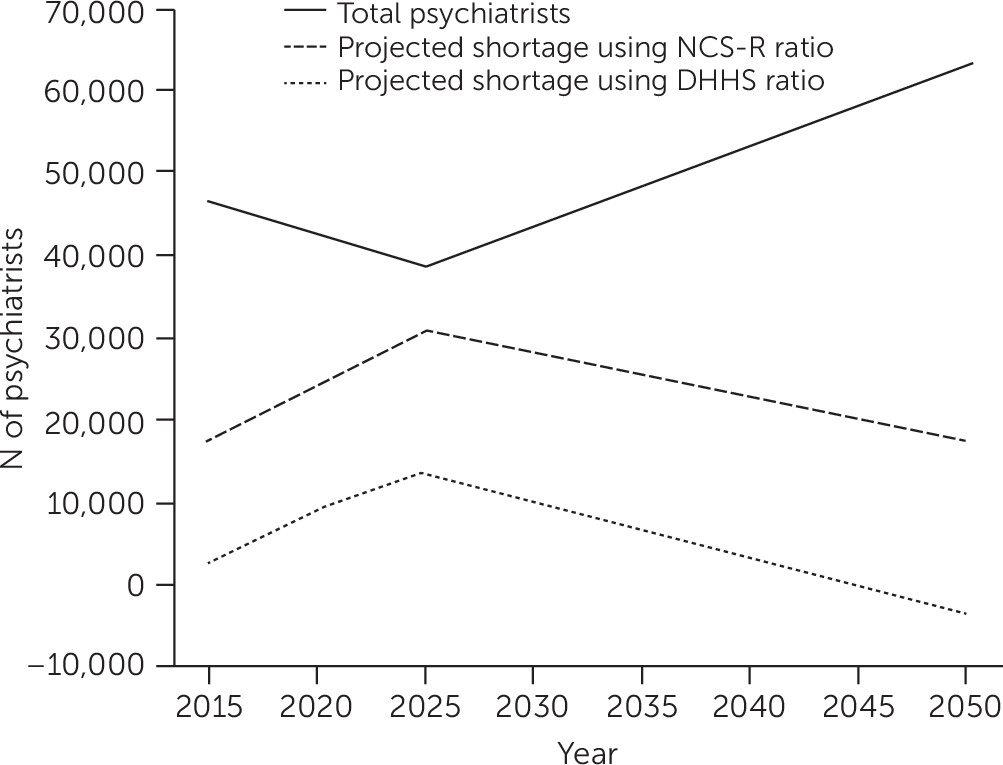
We aimed to quantify and assess the projected workforce of U.S. psychiatrists through 2050. The analysis led to several important findings. First, in the absence of actions to address it, the shortage of psychiatrists will worsen before it improves. With 55% of the total psychiatrist workforce expected to retire within the next ten years, the number of psychiatrists leaving the workforce exceeds the number entering by a multiple of two. The contraction of the workforce will continue through 2024. Second, there will be an inflection point at the end of 2024 wherein this trend reverses, because the large cohort of pending retirees will have left the workforce. At that time, there will be an estimated 38,821 psychiatrists and a shortage of 14,280–31,091 psychiatrists, depending on which established psychiatrist-to-population ratio is used (
Figure 1). Third, beginning in 2025, the supply of psychiatrists will begin to expand because the flow of new psychiatrists into the workforce will exceed the number exiting due to retirement. This entails a gradual process, however. For example, a return to the estimated 2017 shortage of psychiatrists (5,529–20,701) is not expected to occur until approximately 2039.
The inflection point marked by the end of 2024 is critical because it delineates two time frames to target in addressing the shortage: the present through 2024 and 2025 onward. Some strategies may be implemented with clear intent to curb the extent of the shortage at the inflection point, whereas others may aim to curtail the shortage over the next 30 years. As an example, a strategy such as increasing the number of psychiatry residency positions would be expected to build the workforce over decades given the time required to attract and train psychiatrists. In contrast, innovative models of care (for example, collaborative care), an increase in prescribers (for example, nonphysician behavioral health care providers), or use of technologies (for example, telepsychiatry and new interventions) may affect workforce needs prior to 2024.
Fourth, given that these projections extend more than 30 years into the future, it is difficult to determine whether the shortage will be completely alleviated by 2050 without any intervention. Projections based on the proposed DHHS ratio indicate a minimal surplus by 2050, whereas Konrad colleagues’ proposed ratio would result in a continued shortage. Fifth, it is important to note that when viewed both in isolation and in the context of previous studies on this topic, these results are consistent with the existence of a pending and significant shortage of psychiatrists in the United States. The precise amount of the shortage, however, varies among studies. Compared with the 2016 U.S. DHHS HRSA study (
22), our 2013 data show a similar number of psychiatrists (45,580 and 45,533, respectively) and project a similar number of psychiatrists entering the workforce by 2025 (20,470 and 22,947, respectively). However, our data project fewer psychiatrists retiring through 2025, which accounts for the differing projections of supply of psychiatrists (45,210 in the DHHS HRSA study and 39,819 by our estimate) as well as for the overlapping but different projections of the shortage in 2025 (6,080–15,400 and 13,671–30,712, respectively) (
22).
As with any set of projections, this analysis was limited by the assumptions built into the model. We assumed that the number of new entrants into the workforce each year was equivalent to the number of newly granted ABPN psychiatric board certifications. We acknowledge that physicians who are not board certified may operate as psychiatrists and thus increase the effective workforce. However, 2010 data showed that 75% of physicians with an active license were in fact certified by one or more American Board of Medical Specialties boards and that this percentage was “dramatically” higher (to 86%) among physicians age 30 and older as they enter the workforce (
23). The projected number of annual ABPN psychiatric board certifications was also held constant in our model. On the basis of the literature, it was also assumed that psychiatrists would retire at age 65; however, some psychiatrists instead may elect to reduce their commitment to practice over time. U.S. Census Bureau population projections were also assumed to be accurate. Finally, we assumed that the psychiatrist-to-population ratio will remain constant. However, we acknowledge that changes in models of care, demand for new services, new technologies, treatment innovations, and payment and policy reforms could alter the psychiatrist-to-population ratios used in this model.
Conclusions
Because of steady population growth and the expected retirement of more than half the current psychiatrist workforce, the workforce of U.S. psychiatrists will continue to contract through 2024—to a projected shortage of 14,280–31,091 psychiatrists—if no interventions are implemented. Beginning in 2025, the workforce will begin a gradual process of expansion, but it is unclear whether the shortage will have completely resolved by 2050. Future research should focus on developing strategies to address this quantified shortage, in an effort to curb the worsening shortage through 2024 and to address workforce needs in the coming decades.