Suicide is the 10th leading cause of death in the United States and imposes substantial economic costs; estimates associated with suicide and suicide attempts are around $95 billion annually (
1,
2). This substantial social and economic toll has prompted calls for more research and intervention to help prevent suicide and self-harm behaviors. Attention has been focused on emergency departments (EDs) as a currently underutilized location for suicide prevention efforts (
3,
4). In the United States, approximately 500,000 suicide-related visits to the ED occur annually, and up to 25% of individuals presenting for suicide attempts in the ED will make another attempt (
5,
6).
Few studies have examined screening and intervention as an approach to suicide prevention (
7–
11), and findings from these studies suggest that screening and follow-up interventions may be effective or cost-effective, compared with usual care. For example, Denchev and colleagues (
7) estimated the expected cost-effectiveness, compared with usual care, of three outpatient interventions (i.e., follow-up postcards and care letters, follow-up telephone outreach, and suicide-focused cognitive-behavioral therapy) to reduce suicide risk among individuals presenting at hospital EDs. They found each of these interventions to be cost-effective, compared with usual care, based on an assumption of a willingness to pay ≥$50,000 per life-year.
This study aimed to add to the knowledge base by analyzing the cost-effectiveness of suicide screening and intervention implemented as part of a larger suicide prevention study—the Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE) study.
ED-SAFE Study Design
Participants in the ED-SAFE study were recruited in eight general EDs across seven states from August 2010 through November 2013 (
12). The participating EDs ranged from small community hospitals to large academic center hospitals (
13). The sites were randomly assigned to one of four cohorts, with each cohort assigned to a different start date from which it progressed through three study phases sequentially. The three phases were treatment as usual (phase 1), universal screening (phase 2), and universal screening plus intervention (phase 3).
In the treatment-as-usual phase, participants were screened and treated per the ED’s existing suicide-related protocols to establish a study baseline and comparison group. In the universal screening phase, a universal screening protocol for suicidality was added to treatment as usual and implemented by ED nurses. The universal screen, the Patient Safety Screener–3 (PSS-3), is a three-item measure that assesses depressed mood, active suicidal ideation in the past 2 weeks, and lifetime suicide attempt (
12).
In the universal screening plus intervention phase, screening was enhanced by adding an assessment of the level of suicide risk through a physician-led secondary suicide risk assessment for patients who screened positive on the PSS-3. The intervention included the provision of a self-administered personal safety plan (a structured tool to identify early warning signs of suicidal behavior and internal and external coping resources), mental health treatment information, and suicide hotline resources at ED discharge. Following discharge, participants in the universal screening plus intervention phase were contacted through a series of telephone calls. These intervention telephone calls were based on the Coping Long Term with Active Suicide Program (CLASP) protocol and modified for use with ED patients (
14). CLASP-ED telephone calls were provided by a centralized team of psychologists and counselors that served all eight EDs. Each participant who screened as needing the intervention was eligible to receive up to seven telephone sessions, and a participant’s significant other or family member was eligible to receive up to four telephone sessions. These sessions were spread out over the course of 1 year. The sessions evaluated current suicide and psychological status and reviewed the patient safety plan (
12).
Study participants were enrolled in the ED-SAFE study by research assistants at each ED site. Individuals with any level of harm ideation or behavior upon entry to the ED were eligible to be approached for study inclusion. Across all phases, 1,376 participants were enrolled; of these, 1,339 had sufficiently complete data to be included in the cost-effectiveness analysis reported here. Only 3% of enrolled participants, proportionally distributed over the three phases, were excluded because of missing data.
Methods
Cost Estimates
Screening and intervention costs were calculated from the provider perspective (i.e., the hospital ED) to provide critical information to entities evaluating whether they should expand suicide prevention services. We worked with the study’s clinical staff from December 2011 to June 2016 to identify clinical activities typically performed as part of the screening and intervention. The economic study was deemed not to be human subjects research and waived by the institutional review board. We did not include costs incurred by other entities or costs incurred by patients (e.g., travel costs). We also did not include costs associated with research activities because these activities were not part of real-world clinical care. We used a microcosting approach and collected cost data at the activity level from each site for each study phase. This information was collected through two telephone interviews with each site’s principal investigator, other ED administrative staff or research assistants as needed, and supervisory staff performing the CLASP-ED component.
Data on resources used to perform the activities were combined with price data, such as hourly wages and rents, to produce a total unit cost estimate for each activity. Hourly wages and other salary data were collected for each staff type and, if a specific staff wage was not available, we used the mean hourly wage for that staff type from the Bureau of Labor Statistics Wage Data by Metropolitan Area (
http://www.bls.gov/oes/current/oessrcma.htm) adjusted to 2015 U.S. dollars by use of the Consumer Price Index. Space costs were estimated by using an average rental rate for medical and hospital office space where each site was located as obtained from real estate listings found on LoopNet (
www.loopnet.com) and cross-referenced with findings from the Newmark Grubb Knight Frank National Office Market Report (
15).
The activities performed for each patient were multiplied by the estimated unit cost for each activity to produce a cost per patient by site and phase. The quantity of activities performed for each patient was tracked as part of the ED-SAFE study through chart reviews of the patient’s index ED visit. Summing across patients within a phase and site yielded the total cost of the phase at a site. We then calculated the average across sites to get an average cost for each phase at the site level. All costs were calculated in 2015 U.S. dollars.
Cost-Effectiveness Analysis
Effectiveness measures (screening and suicide outcomes).
Screening outcome measures for the cost-effectiveness analysis included the percentage of ED patients screened for suicide risk and the percentage of ED patients who screened positive for suicide risk. These measures were developed by using screening data from the study’s screening log database that included nearly 250,000 patients entering the eight ED sites during each phase of the ED-SAFE study. For each site, the percentage of ED patients screened was calculated by dividing the number of screened patients at the ED site by the total number of patients entering the ED site during the relevant phase. Because the universal screening approach was the same in the universal screening and the universal screening plus intervention phases, the percentage of clients screened was averaged across these two phases to calculate a single value for the percentage of patients screened for each site. This percentage was compared with each site’s treatment-as-usual screening percentage. A similar calculation was done for the percentage of patients who screened positive.
Suicide outcome measures included a suicide composite measure that documented any suicide attempts or death by suicide over the 12 months following the index ED visit (
14). This measure was operationalized as patient-level counts of the number of suicidal acts over the 12-month period following the index ED visit.
Following the methodology used in the study’s main suicide outcome report, we used a negative binomial model to calculate predicted values for the number of suicidal acts as a way to account for overdispersion in the outcome (
16). Each model included categorical variables for study phase and dichotomous variables for ED site. The model also included several patient-level variables representing patient demographic factors and baseline status (
16).
Cost-effectiveness.
Separate cost-effectiveness analyses were performed to compare the three phases across the screening and suicide outcome effectiveness measures. In each case, we calculated an incremental cost-effectiveness ratio (ICER) that combined differences in cost and effect between the phases (
17). We first ranked the phases in increasing order of average cost. The ICER was then computed as the difference in average cost divided by the difference in average effectiveness.
For the screening measures, we examined use of a universal screen compared with treatment as usual. We divided the ED sites into two groups—those without any screen prior to the study (N=4) and those with an informal, nonuniversal screen prior to the study (N=4)—and conducted separate cost-effectiveness analyses for each group. This allowed us to examine the cost-effectiveness associated with going from no screening to universal screening and with going from an informal nonuniversal screen to universal screening. An informal screen was defined as use of a set of nonstandardized questions to determine suicidal ideation or behavior; therefore, these screens were not equivalent to universal screening. Costs used for these analyses were the average screening costs per month per site.
For the suicide outcome measure, we compared the three phases—universal screening plus intervention, universal screening (added to treatment as usual), and treatment as usual alone—with all eight ED sites included in the analysis. For these analyses, we used total phase costs per patient.
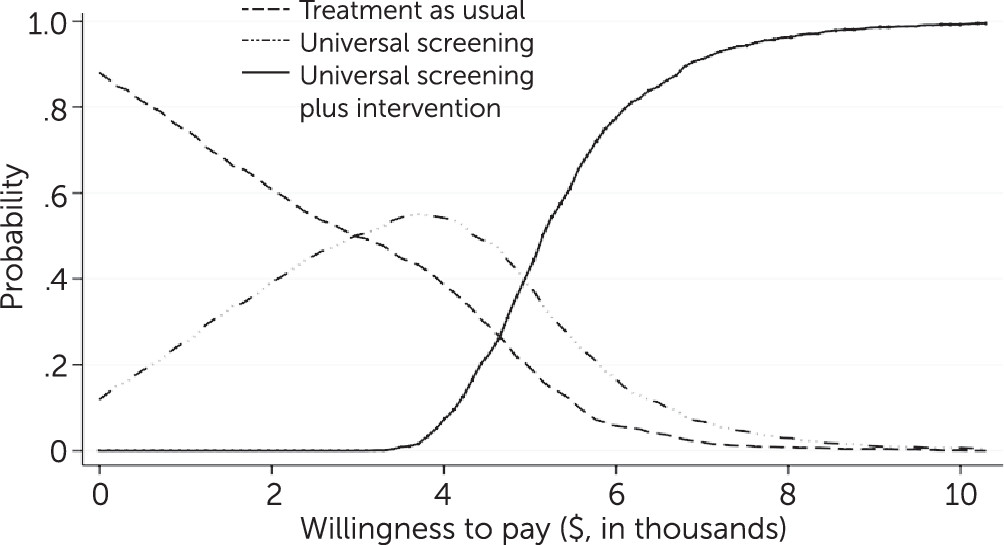
Cost-effectiveness acceptability curves.
Using a nonparametric bootstrap method, we calculated a cost-effectiveness acceptability curve (CEAC) to show the probability that a given phase was the cost-effective option as a function of a decision maker’s willingness to pay for the suicide composite outcome. The CEAC incorporated the joint variability of the cost and effectiveness estimates and allowed us to better capture the variability in our cost-effectiveness analysis in lieu of calculating confidence intervals for the ICERs (
18,
19).
Results
Screening
Table 1 presents costs and outcomes associated with the addition of universal screening for four sites without a formal screen in the treatment-as-usual phase. As shown, the mean percentage of patients screened substantially increased moving from treatment as usual to universal screening—from 8% to 71% (p<0.01). The percentage of patients screening positive for suicidality also increased, from 3.3% to 6.8% (p<0.01). The addition of universal screening was associated with an average increase in monthly site-level costs of $604 (p<0.05). Dividing the increase in costs ($604) by the change in screening rates (71%−8%) yielded an ICER of approximately $10 per 1 percentage point increase in the monthly screening rate. Similarly, for the percentage of patients who screened positive for suicidality, the ICER comparing universal screening to treatment as usual was approximately $174 per 1 percentage point increase in the rate of individuals who screened positive for suicidality.
Table 2 presents results for the ED sites that already had informal screening approaches prior to the implementation of universal screening. These sites increased their screening rates by 46 percentage points—from 37% to 83%. They also increased the percentage of patients who screened positive by approximately 2 percentage points—from 2.7% to 4.8%. The increase in costs was $215. For overall screening rates, the ICER for universal screening relative to treatment as usual was approximately $5 per 1 percentage point increase in the monthly screening rate. For positive screens for suicidality, the ICER was approximately $106 per 1 percentage point increase in the rate of individuals who screened positive for suicidality.
Participants
Of the 1,376 participants enrolled in the study, the median participant age was 37, and 56% (N=769) were women. Sixty-seven percent (N=928) were non-Hispanic white, 15% (N=205) were non-Hispanic African American, 12% (N=171) were Hispanic, and 5% (N=72) identified as non-Hispanic other. Over 70% (N=967) of the sample had a history of previous suicide attempts and over one-third (N=459) had made a suicide attempt in the week prior to the ED visit (
16).
Suicide
As shown in
Table 3, the average per-patient costs for treatment as usual and for the universal screening phase were estimated as $513 and $566 per month, respectively. Universal screening plus intervention costs were significantly higher at $1,063 per patient per month (p<0.01); the addition of the telephone sessions drove this increase. The universal screening plus intervention phase was also more effective in averting suicide attempts and deaths by suicide, compared with both universal screening and treatment as usual. Similarly, the universal screening phase was more costly but more effective compared with treatment as usual, although this cost difference was not statistically significant. Moving from treatment as usual to universal screening decreased the average number of suicide attempts and deaths by suicide by approximately 0.02 (0.454–0.435, not significant), increased the cost by $53 (not significant), and yielded an ICER of $2,789 per averted suicide attempt or death by suicide over the 12 months post-ED visit. Moving from universal screening to universal screening plus intervention further decreased suicide attempts and deaths by 0.099 (0.435–0.336, p<0.01) and increased costs by $497 (p<0.01), yielding an ICER of $5,020 per averted suicide attempt or death by suicide. [Incremental cost and outcome scatterplots are presented in an
online supplement to this article.]
Figure 1 includes the CEACs for the number of suicides attempts or deaths by suicide. The CEACs show the probability that a given phase was cost-effective relative to the two alternatives for a given willingness-to-pay amount. The treatment-as-usual and universal screening phases had the highest probability of being cost-effective for low willingness-to-pay values (<$5,000). However, once the willingness-to-pay amount was greater than $5,000, universal screening plus intervention had the highest probability of being cost-effective, and this probability was greater than 80% for willingness-to-pay values exceeding $6,000. If a decision maker is willing to pay over $6,000, then the universal screening plus intervention phase has the highest probability of being cost-effective and would be their optimal choice.
Discussion
Suicide detection and prevention efforts that target individuals presenting at EDs are a critical component in reducing suicide attempts and death by suicide given the high number of suicide-related ED visits that occur annually in the United States. Understanding the cost-effectiveness of these services can aid in their implementation and dissemination as well as in the development of further suicide prevention efforts.
Implementing universal screening increased average costs between $215 and $604 dollars per site per month depending on whether the ED already had an informal screening process in place. However, with the increased use of universal screening, the percentage of participants screened and the percentage of participants who screened positive for suicide risk increased. The calculated ICER showed that it cost about $106 to $174 per 1 percentage point increase in the monthly screened-positive rate.
These results suggest that universal screening may be a cost-effective screening intervention, compared with treatment as usual. However, once a patient is positively identified as being at risk of suicide, a cost-effective treatment is needed. Universal screening plus intervention showed a reduction in the per-person number of suicide attempts and deaths by suicide, compared with treatment as usual and universal screening. The effectiveness study conducted by Miller et al. (
16) showed that these results are statistically significant. However, this reduction comes at a cost: universal screening plus intervention costs for each ED site were almost double those of treatment as usual and universal screening. Although universal screening plus intervention costs more than treatment as usual and universal screening, the increased effectiveness suggests that universal screening plus intervention may be more likely to be the optimal choice among the three alternatives. Our analysis showed that for willingness-to-pay values above $5,000 per suicide attempt or death by suicide, universal screening plus intervention had the highest probability of being the cost-effective choice.
For the suicide outcome with an estimated ICER of $5,020 per averted suicide attempt or death by suicide, it is possible to illustrate the potential cost savings of the universal screening plus intervention with existing literature. Although deaths by suicide were captured in our data, we focused on suicide attempts because deaths were a rare event during the study follow-up period. Shepard et al. (
2) estimated the annual cost of nonfatal attempted suicides in the United States at $5.34 billion (2015 dollars), with 395,000 suicide attempts officially reported annually. Calculating a per-person cost yields an estimated annual cost of $13,522 per attempt. Therefore, universal screening plus intervention would yield a cost savings of $8,502 per averted suicide attempt from a societal perspective ($13,522–$5,020). Based on the annual 395,000 reported suicide attempts, if even just 25% of these attempts were averted each year through use of universal screening plus intervention, society would benefit by cost savings of almost $840 million annually. These results show that the combination of suicide screening in the ED and a post-ED intervention for those who screen positive provides both economic and clinical value to society (
16).
Our study had a few limitations. First, we relied on the judgment of the study’s principal investigators (PIs) in regard to which activities were primarily research related and which would be used in best ED practice. Furthermore, study PIs provided data on labor time needed to complete activities in each phase; this approach was used instead of relying on time logs or other mechanisms for direct measurement because such approaches were deemed too burdensome for the ED staff. Second, we did not include all the costs associated with administrating a universal screening, such as ongoing training and quality control measures (e.g., record checks). Finally, our analysis was conducted in the context of an ED; the effectiveness and cost estimates presented here are unlikely to apply in other clinical settings.
Conclusions
Despite its limitations, our study makes an important contribution to the literature by providing further economic evidence of the value of suicide screening and intervention in an ED setting. Our study demonstrates the potential cost-effectiveness of both universal screening and intervention, compared with universal screening added to treatment as usual or treatment as usual alone, in detecting and reducing suicide acts at 12 months post-ED visit. Although the choice of universal screening plus intervention as an economically optimal intervention depends on the value placed on these outcomes by decision makers, our results suggest that there is the potential for significant societal cost savings in implementing such suicide prevention measures.
Acknowledgments
The authors thank the following individuals who served as ED-SAFE investigators: Marian E. Betz, M.D., M.P.H., University of Colorado Hospital, Aurora; Jeffrey M. Caterino, M.D., Ohio State University Wexner Medical Center, Columbus; Talmage Holmes, Ph.D., M.P.H., University of Arkansas for Medical Sciences Medical Center, Little Rock; Maura Kennedy, M.D., M.P.H., Beth Israel Deaconess Medical Center, Boston; Frank LoVecchio, D.O., M.P.H., Maricopa Medical Center, Phoenix; Lisa A. Uebelacker, Ph.D., Memorial Hospital of Rhode Island, Providence; Wesley Zeger, D.O., University of Nebraska Medical Center, Omaha.